Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Turning Cramps into Comfort: A Review of Yogas Role in Alleviating Primary Dysmenorrhea and Promoting Reproductive Health
Authors: Taruni Sarva, Avilash Mohapatra, Ganesh Kumar Subudhi
DOI Link: https://doi.org/10.22214/ijraset.2025.66546
Certificate: View Certificate
Abstract
Dysmenorrhea, the most frequent menstrual problem in adolescence, is a widespread condition affecting women globally. It is highly prevalent, affecting around 50–90% of the female population, with a global prevalence rate of 71.1% according to a meta-analysis spanning 38 countries. Primary dysmenorrhea (PD) is a common menstrual disorder affecting many women and significantly impacting their quality of life. The symptoms of PD are lower abdominal or pelvic pain, which may radiate to the back or legs, typically starting 6 to 12 months after menarche. Dysmenorrhea caused significant effects, including school absenteeism, poor performance, difficulty in daily activities, and social life disruption. Yoga, as non-pharmacological alternative medical intervention, has been increasingly studied for its potential benefits in managing PD. The purpose of this review is to highlight Yoga therapy as most effective alternative treatment in this cutting-edge era for primary dysmenorrhea. This study reviewed English-language literature published from 2000 to 2024, searching databases like PubMed, Google Scholar, and Scopus using keywords “yoga” and “menstrual pain” or “dysmenorrhea.” Out of 1,453 articles, 12 studies met the selection criteria and were included in the final review. This review of 12 RCTs’ highlights the effectiveness of yoga therapy for managing primary dysmenorrhea. Various yoga practices, including asanas, Yoga Nidra, and pranayama, significantly alleviated pain and improved symptoms. This study concludes the positive effectiveness of yoga therapy in managing primary dysmenorrhea. Yoga practices significantly alleviated pain and improved physical, psychological and social aspects of health, suggesting yoga as a holistic and beneficial treatment for dysmenorrhea.
Introduction
I. INTRODUCTION
Dysmenorrhea, the most frequent menstrual problem in adolescence, is a widespread condition affecting women globally. Its impact on quality of life is considerable, often leading to absenteeism from both work and social events. Menstrual disorders are a common issue globally, affecting women in different regions [1]. These disorders can impact their work, education, quality of life, and contribute to various health problems [2]. There is a lack of longitudinal studies on the natural history of dysmenorrhea and the potential impact of various modifiable risk factors. Let's talk about dysmenorrhea and primary dysmenorrhea before getting into the review.
Dysmenorrhea, defined as painful menstrual cramps of uterine origin, is the most common gynecological condition among women of reproductive age [3]. 'Dysmenorrhea' originates from the Greek words 'dys’, which signifying difficult or painful, 'meno' for month, and 'rrhea' for flow, describing the painful or abnormal menstrual flow. It is categorized basically into two types: primary dysmenorrhea (PD), which lacks any underlying organic disease, and secondary dysmenorrhea (SD), which is associated with pelvic pathology [4]. Primary dysmenorrhea is defined as painful, spasmodic cramping in the lower abdomen, just before and/or during menstruation, in the absence of any discernable macroscopic pelvic pathology [3].
As we know that women's health plays a crucial role in the overall well-being of society, as women make up nearly half of the global population. As of 2024, the global sex ratio; across all ages, the global population is nearly balanced, with 101 males for every 100 females [5]. As women reach puberty, they begin their monthly menstrual cycle. The blood loss during menstruation can lead to iron deficiency, which may negatively impact a woman's health. During menstruation, many women experience symptoms such as lower abdominal or lower back pain, mood changes like irritability and mood swings, headaches, digestive issues and fatigue [6]. These symptoms can impact women's physical, social, and psychological well-being, leading to a decline in workforce participation and affecting the global economy [7].
A detailed study conducted by the NICHD (National Institute of Child Health and Human Development) found that 14% to 25% of women of reproductive age reported experiencing menstrual irregularities, highlighting a significant gap in women's healthcare needs (NICHD, 2023) [8]. A study revealed that 71.96% of adolescent girls reported dysmenorrhea, with 33.95% experiencing it monthly and 16.90% suffering from it most months [9]. Dysmenorrhea affects between 45% and 95% of women of reproductive age worldwide, leading to notable disruptions in daily life, including reduced school and work productivity [10]. In a study by Chauhan & Kodnani (2016), 28% of participants had irregular periods, and 67% experienced moderate to heavy flow and 85% girls had family history of dysmenorrhea. Dysmenorrhea caused significant effects, including school absenteeism (65%), poor performance (56%), difficulty in daily activities (73%), and social life disruption (64%). Common physical symptoms were lower abdominal pain (42%) and backache (35%), while psychological symptoms like irritability (61%) and emotional instability (46%) were also commonly reported [11]. Menstrual pain affects approximately 25–50% of adult women and about 75% of adolescents. Among women, 5–20% report experiencing severe dysmenorrhea that prevents them from engaging in their regular activities [12].
According to the UNESCO MHHM (United Nations Educational, Scientific and Cultural Organization Menstrual Health and Hygiene Management) survey and gap analysis report, it is essential to begin educating children about menstrual health and hygiene management by the age of 10 [13]. The author believes that this education will boost society's well-being in addition to empowering women. Determining the epidemiology of primary dysmenorrhea is complicated by the fact that it is perceived differently by women and by the variation in the diagnostic criteria often used. Adolescent girls, almost always, silently suffer the pain by dysmenorrhea and the discomfort associated with it due to lack of knowledge about reproductive health. It is probable that this also affects their academic and social performance [9].
Yoga, an ancient practice from the Indus Saraswati Valley civilization, has long been recognized for its benefits to both physical and mental well-being. Widely regarded as a form of harmonious medicine, it is particularly effective in managing menstrual disorders such as dysmenorrhea [14]. Studies show that yoga helps alleviate menstrual pain and supports the mind-body connection by reducing stress hormones like cortisol and adrenaline, while promoting endorphin release for natural pain relief. Research indicates that 70.2% of individuals experience dysmenorrhea, with most favoring non-pharmacological methods, such as yoga, over medication [15]. The aim of this study is to provide a comprehensive narrative review on primary dysmenorrhea (PD), exploring its underlying mechanisms and the debilitating symptoms, it causes. Additionally, the paper seeks to examine the therapeutic role of yoga in alleviating pain and discomfort associated with PD, highlighting the potential benefits and effectiveness of yoga as an alternative treatment approach.
II. METHODOLOGY
A. Literature Search
To conduct this narrative review, an extensive search of electronic databases, including PubMed, Google Scholar, and Scopus was carried out. The focus of the search was on studies published from 2000 to 2024 to ensure the inclusion of recent developments in the field of yoga and women’s disorders. Keywords such as “yoga” AND “dysmenorrhea” OR “menstrual pain” were employed in various combinations to identify relevant articles.
B. Study Selection
Only original research articles relevant studies to the review topic were included. The inclusion criteria were limited to randomized control trials (RCTs) that evaluated the impact of yogic practices on symptoms of primary dysmenorrhea and menstrual discomfort. Exclusion criteria included articles not available in English and those published before 2000. Duplicate articles and those exclusively featuring other therapies without yogic intervention were also excluded. Outcome measures for assessing the efficacy of interventions included various questionnaires, such as the Visual Analogue Scale (VAS) and the Numerical Rating Scale (NRS) for pain.
C. Data Abstraction
A total of 1,453 records were identified through database searches and other sources. After eliminating 20 duplicate studies, and based on title and abstract review, 1345 studies were excluded for reasons such as being thesis, dissertations, case reports, perspective articles, personal accounts, reviews, encyclopaedia entries, posters, or book chapters, 88 records underwent screening. After this, 12 full-text articles were reviewed for eligibility, while 76 were excluded due to unavailability of full text, combined therapy approaches, other menstrual disorders or not being randomized controlled trials (RCTs). Ultimately, 12 studies (Table 1) fulfilled the inclusion criteria and were selected for the final analysis.
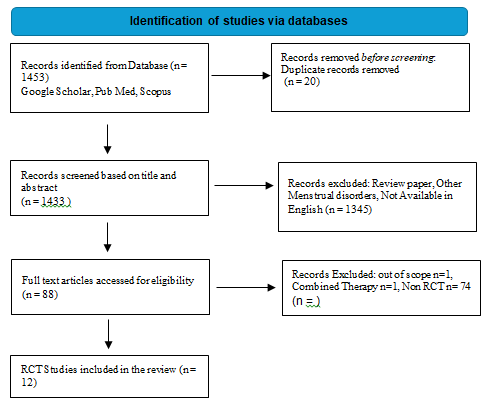
Figure 1: Selection process of Included studies
TABLE I
List of included 12 RCT studies of Yoga on Dysmenorrhea
|
Citation details
|
sample size Age |
Intervention |
Outcome measure |
Result and Conclusion |
|
Rakhshaee et al. 2011 [16] |
Yoga group (n = 50) Control group (n = 42) 18-22 years old |
Experiment group: yoga 20 minutes for 14 days at luteal phase Control group: no intervention |
Menstrual characteristic questionnaire (e.g., pain intensity and duration), VAS |
Greater reduction in pain intensity (p < 0.05) in the Intervention group as compared with the control group. |
|
Sakuma et al. 2012 [17] |
Yoga (n = 67) Control group (n = 31) 20-64 years old |
Experiment group: yoga for 4 weeks Control group: no intervention |
VAS, GHQ-30 |
Participants reported reduced dysmenorrhea (p = 0.044) at 4 weeks. Decrease in GHQ score was observed that showed improvement in menstrual distress |
|
Monika et al. 2012 [18] |
Yoga (n = 75) Control group (n = 75) |
Experiment group: 35-40 min yoga nidra for 6 months + medication Control group: medication |
Autonomic function test (CANwin) & Variowin |
Significant (p < 0.05) reduction in dysmenorrhea |
|
Rani et al. 2013 [19] |
Yoga (n = 75) Control group (n = 75) |
Experiment group: yoga Nidra + medication Control group: medication |
Blood test, |
Significant reduction in pain (p < 0.006), gastrointestinal, cardiovascular and urogenital symptoms in intervention group as compared to control group |
|
Nag, Usha; Kodali, Madhavi; 2013 [20] |
Yoga (n = 60) Control group (n = 53) 18-23 years old |
Experiment group: 40-minute yoga session, pranayama, meditation for 3 months Control group: No intervention |
Semi structured proforma & NRS |
Significant reduction in pain & absenteeism in the study group compared with the control group |
|
Yang et al. 2016 [21] |
Yoga (n = 20) Control group (n = 20) |
Experiment group: 60 min yoga for 12 weeks Control group: no intervention |
VAS, SF-MDQ |
significant reduction in dysmenorrhea intensity (p < 0.001) and distress in intervention group and compared to the control group |
|
Yonglitthipagon, et al. 2017 [22] |
Yoga group= 17 Control =17 18-22 years old |
12 week , for one 30 min session Control group: no intervention |
VAS, SF-36 |
Reduce menstrual pain intensity, improve flexibility & leg muscle strength and QOL in experimental group than control group |
|
Aggarwal et al. 2020 [23] |
Group A: 12 Group B: 12 Group C: 12 18-22 years old |
Group A: Three asanas Group B: pranayama Group C: combined all three asanas with pranayama |
NPRS, VMSS |
Combined yoga asana with pranayama enhancing QOL reduce pain. |
|
Geetha, K; Elangovan, R; 2022 [24] |
Yoga group: 15 Control group: 15 18-22 years old |
Yoga group: Yogic practices for 12 weeks, 6 days in a week Control group: No intervention |
Menstrual frequency |
Results are statistically significant (P<0.05). Yogic practices help to reduce menstrual frequency |
|
Haryono, Ignatio et al. 2023 [25] |
Yoga group: 25 Control group: 25
|
Hata yoga: 3 days in a week for 12 weeks Control group: No intervention |
NRS |
Significantly reduce pain intensity. |
|
Kulkarni, Pratiksha; 2023 [26] |
30 students divided in group A and B 14-18 |
Yoga asanas: 4 weeks to 30 minutes control group: no intervention |
VAS |
significant reduction in the VAS score of group A (P=0.0002) and group B did not show any difference in the VAS score post treatment |
|
Deepika, S; 2024 [27] |
Experimental group: 30 Control group: 30 14-18 years old |
Structured yoga intervention: 6 days in a week for 12 weeks control group: no intervention |
BMI, VAS |
significant reduction in pain level with P value <0.001, highlighting yoga efficacy in elevating PD symptoms. |
III. RESULTS
All RCTs focused on the effects of yoga programs in managing primary dysmenorrhea. The assessment methods used in these studies included various questionnaires such as VAS and NRS for pain, GHQ-30 for menstrual distress, SF-36 for quality of life, WALIDD for diagnosis, modified SF-MDQ to assess both psychological and physical aspects, VMSS for dysmenorrhea severity, blood tests for hormonal profiles, and BMI for weight. The interventions comprised a range of yoga practices, including yoga poses, Yoga Nidra, and pranayama. Among the 12 studies, six had no intervention in the control group, while one included medication in the control group. Pain measurement was primarily assessed using VAS in 10 studies and NPRS in 2 studies. These findings suggest that yoga is an effective intervention for managing PD. All the included studies reported significant improvements in relieving symptoms through various yoga practices, such as asanas, pranayama, meditation, and Yoga Nidra relaxation techniques.
IV. REVIEW
A. Ways to Identify Primary Dysmenorrhea
The symptom of PD is lower abdominal or pelvic pain, which may radiate to the back or legs, typically starting six to twelve months after menarche, coinciding with the initiation of ovulatory cycles [28]. Symptoms usually start in adolescence and can result in absenteeism from school and work, as well as limitations in social, academic, and sports activities [29].
Another study revealed that adolescent girls with dysmenorrhea experience a range of symptoms, including gastrointestinal issues such as nausea and appetite changes, psychological symptoms like irritability and trouble concentrating, elimination problems such as constipation and diarrhea, and physical symptoms like fatigue, headaches, and joint pain, all of which significantly impact their overall well-being [9]. The pain in the lower abdomen or pelvis generally lasts for 8 to 24 hours, often starting with menstrual flow. Additional symptoms may include lower back and thigh pain, headaches, diarrhea, fatigue, and sometimes nausea or vomiting [4]. PD can result in chronic pain, psychological stress, and substantial effects on quality of life and productivity in school and workstation. It is highly prevalent, affecting around 50–90% of the female population, with a global prevalence rate of 71.1% according to a meta-analysis spanning 38 countries. In the UK and parts of Europe, community studies report prevalence rates between 45% and 97%, while a survey in Canada found that 60% of menstruating individuals experience primary dysmenorrhea [30].
Dysmenorrhea is pelvic pain, often radiating to the lower back or thighs or upper legs, described as cramping, pressure, or heaviness, and typically ending with menstrual flow [31]. Young women with menstrual pain commonly reported fatigue, nausea, and vomiting, along with other symptoms like dizziness, headaches, depression, diarrhea, and general discomfort during their periods [6].
B. Measurement of symptoms in primary dysmenorrhea
In 1979, the International Association for the Study of Pain (IASP) introduced the widely accepted definition of pain as "An unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage," a formulation recommended by the Subcommittee on Taxonomy and adopted by the IASP Council. However, it is now proposed that this definition be revised to: "An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage." This revised definition broadens the understanding of pain, allowing for greater flexibility in capturing the complex nature of pain experiences, including those that may not be directly linked to tissue injury but are still perceived as painful [32]. Two commonly used tools for assessing the severity of dysmenorrhea include a verbal multidimensional pain scoring system and a visual analogue scale (VAS). The verbal multidimensional pain scoring system evaluates pain severity by considering its impact on daily activities, associated systemic symptoms, and the need for analgesics. In contrast, the VAS involves the patient rating the intensity of dysmenorrhea on a linear scale, providing a simple yet effective measure of pain severity. Both tools offer valuable insights into the extent of pain experienced, allowing healthcare providers to tailor appropriate interventions [33].
C. Impact of Primary Dysmenorrhea on Hormonal Balance
The pathophysiology of primary dysmenorrhea (Figure 2) is not fully understood but reports suggest that dysmenorrhea has inflammatory components that stimulate endometrial cells to release prostaglandins, which cause pain before or during menstruation. The intensity of dysmenorrhea symptoms can differ among women and from cycle to cycle, with individuals suffering from depression, anxiety, and stress being more likely to experience severe symptoms [7]. Pathophysiology of primary dysmenorrhea involves two key mechanisms: uterine contractions and vasoconstriction, along with inflammation, the release of inflammatory mediators, and the activation of pain fibers [5]. Prostaglandins (PG) play a crucial role in the development of primary dysmenorrhea. The condition arises from excessive PG production in the uterus, which causes forceful myometrial contractions. These contractions diminish uterine blood flow, leading to ischemia and pain. Ovarian hormones, under the influence of gonadotropins, enhance prostaglandin production, while vasopressin further intensifies uterine contractions [34]. Prolactin and psychological factors can increase pain sensitivity, with neural pathways mediating its perception. Cervical and other contributing factors have a lesser or less established role. These combined processes lead to the characteristic symptoms of primary dysmenorrhea [35].
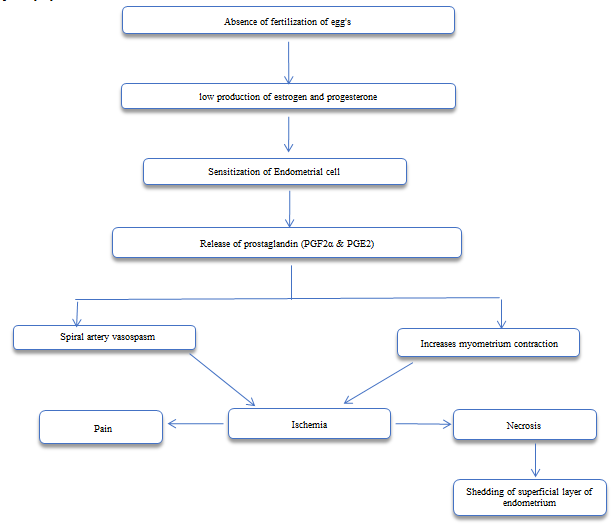
Figure 2: Pathophysiology of primary Dysmenorrhea
PD is strongly associated with stress from work, and life. By inhibiting follicle-stimulating and luteinizing hormone release, stress impairs follicular development, which can disrupt progesterone production and influence prostaglandin activity [36]. Severe dysmenorrhea is linked to high stress and reduced productivity, with 20–24% of students missing school and 37% cutting back on social and sports activities. It causes 1–2 lost workdays per month for 10–30% of women, costing the U.S. economy about $2 billion annually [7].
Let us delve into a brief exploration of the ancient origins of yoga and its profound impact on alleviating the symptoms of primary dysmenorrhea. Yoga, regarded as an enduring cultural legacy of the Indus Saraswati Valley civilization, which dates to around 2700 B.C., has consistently contributed to both the material and spiritual well-being of humanity. The practice of yoga originated millennia ago, long before the emergence of the first religions or belief systems [14]. Yoga, originating in ancient India, is widely acknowledged as a form of harmonious medicine and alternative therapy, offering significant benefits for the mind-body connection [37]. Several studies showed that yoga is beneficial for cure of menstrual disorders like dysmenorrhea [38]. Yoga is a foundational mind-body practice that empowers individuals to achieve and sustain sukha sthanam, a state of holistic well-being encompassing physical, mental, and spiritual harmony [39].
About 70.2% of participants experienced dysmenorrhea, with 68.3% reporting consistent pain. Despite this, only 25.5% used medication, and 14.2% sought medical advice, favoring non-pharmacological methods [15]. Nonpharmacological methods such as relaxation therapy can effectively reduce menstrual pain. This also plays a role by reducing stress hormones like cortisol and adrenaline, while stimulating endorphins that naturally relieve pain and elevate mood [40].
A growing body of evidence supports the belief that yoga benefits physical and mental health via down-regulation of the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system (SNS). Yoga may be a safe and cost-effective intervention for managing menstrual problems [41]. A study found that practice of yoga exercise can be applied as an alternative method to reducing menstrual pain and as a reference to adolescent girls about the non-pharmacological treatment of dysmenorrhea [42]. Another recent study suggests that yoga to be as safe as usual care or exercise and yoga practice can effectively alleviate menstrual pain, and the symptoms associated with dysmenorrhea [41].
V. DISCUSSION
As most of the studies focusing on pain aspect of dysmenorrhea, so in this article we mainly trying to find the mechanism behind the pain management through yogic interventions. One study focusing on pranayama for pain reduction in dysmenorrhea. In a study by Karel Nespor (1991) on pain management, voluntary change of respiratory pattern, like lengthening exhalation & avoiding the breath retention after inhalation, may induce more relaxation & may also decrease pain [43]. The experimental study by Aggarwal et al., 2020, supporting the existence of a relationship between alternate nostril breathing and pain reduction . In their study the pranayama session (alternate nostril breathing) began with equal durations of inspiration and expiration (4:4 seconds) for the first three days, progressing to 8:8 seconds by day 4–5, and 16:16 seconds by day 6–7. By the second week, the ratio advanced to 1:2 (16 seconds of inspiration and 32 seconds of expiration). In weeks three and four, participants practiced 4-count inhalation through one nostril, 16-count retention, and 8-count exhalation through the opposite nostril, alternating sides. In this pattern they emphasize the lengthening expiration to manage the pain [23]. In a study by Marcy C. McCall, 2013, the benefits of yoga are commonly attributed to its direct influence on sympathetic and parasympathetic activity in the autonomic nervous system. Reduced sympathetic activation, increased GABA (gamma-aminobutyric acid) levels, and regulation of the HPA(Hypothalamic-Pituitary-Adrenal) axis through pranayama, dhyana, and asanas have been linked to improved mood, reduced stress, enhanced well-being, and anxiolytic effects [44]. In a study by Rakhshaee, 2011, Yoga is thought to reduce pain by regulating the spinal cords gate-control mechanism and enhancing natural painkiller secretion. Breathing exercises promote relaxation, reduce tension, and support pain management through calmer, slower respiration [16]. In a study by Gupta et al., the role of mind-body practices in modulating pain signals is explored. Inflammatory pain, resulting from nociceptor activation via inflammatory mediators released by damaged cells, can be influenced by psychological factors as outlined in the gate control theory. This theory posits that pain perception by the brain through the nervous system can be inhibited or amplified. Mind-body practices such as yoga are suggested to inhibit pain signals, potentially altering the individual’s perception and experience of pain [45]. Yang & Kim, 2016 suggest that the effectiveness of yoga in managing primary dysmenorrhea may be attributed to the downregulation of the HPA axis and the sympathetic nervous system. This mechanism is supported by the sequential practice of yoga, which combines exercise, relaxation, and deep breathing techniques [21]. Yonglitthipagon et al., 2017 suggest that yoga activates the brain’s pain-modulating system, enhancing beta-endorphin secretion, and improving quality of life (QOL) domains like vitality, mental health, and general well-being. The integration of movement and breathing triggers a relaxation response, benefiting metabolism, heart rate, blood pressure, and muscle tension [22].
Kanchibhotla et al., 2023 explains that an increase in vasoactive prostanoids results in myometrial hyperactivity, reduced uterine blood flow, and tissue ischemia, contributing to pain or dysmenorrhea during the menstrual cycle. Yoga, particularly pelvic asanas, is noted to enhance blood flow in the pelvic region, thereby alleviating pain [38].
Conclusion
In conclusion, this study highlights the promising effects of yoga therapy in managing primary dysmenorrhea. The studies included in the review utilized a variety of assessment tools to measure pain, menstrual distress, quality of life, and other related factors, demonstrating a comprehensive approach to evaluating the impact of yoga interventions. The yoga practices investigated, including yoga poses, Yoga Nidra, pranayama, and meditation, consistently led to significant improvements in symptom relief. Notably, the studies reported that yoga interventions were effective in reducing pain and alleviating both the psychological and physical aspects of dysmenorrhea. Overall, the findings suggest that yoga can be a beneficial and holistic treatment option for individuals suffering from primary dysmenorrhea, with positive effects on both pain management and overall well-being.
References
[1] Esan DT, Ariyo SA, Akinlolu EF, Akingbade O, Olabisi OI, Olawade DB, et al. Prevalence of dysmenorrhea and its effect on the quality of life of female undergraduate students in Nigeria. Journal of Endometriosis and Uterine Disorders. 2024 Mar;5:100059. [2] Attia GM, Alharbi OA, Aljohani RM. The Impact of Irregular Menstruation on Health: A Review of the Literature. Cureus [Internet]. 2023 Nov 20 [cited 2024 Dec 16]; Available from: https://www.cureus.com/articles/197833-the-impact-of-irregular-menstruation-on-health-a-review-of-the-literature [3] Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015 Nov;21(6):762–78. [4] Proctor M, Farquhar C. Diagnosis and management of dysmenorrhoea. BMJ. 2006 May 13;332(7550):1134–8. [5] \"Field Listing—Sex ratio\". CIA Factbook. The Central Intelligence Agency of the United States. Retrieved 2024-04-18. (2023 estimates) [6] Abreu-Sánchez A, Parra-Fernández ML, Onieva-Zafra MD, Ramos-Pichardo JD, Fernández-Martínez E. Type of Dysmenorrhea, Menstrual Characteristics and Symptoms in Nursing Students in Southern Spain. Healthcare. 2020 Aug 26;8(3):302. [7] Ishikura IA, Hachul H, Tufik S, Andersen ML. Dysmenorrhea and Sleep. Sleep Medicine Clinics. 2023 Dec;18(4):449–61. [8] NICHD Eunice Kennedy Shriver National Institute of Child Health and Human Development. Available at: https://www.nichd.nih.gov/health/topics/factsheets/menstruation (Accessed: 16 December 2024). [9] Agarwal AK, Agarwal A. A study of dysmenorrhea during menstruation in adolescent girls. Indian J Community Med. 2010 Jan;35(1):159–64. [10] Kirsch E, Rahman S, Kerolus K, Hasan R, Kowalska D, Desai A, et al. Dysmenorrhea, a Narrative Review of Therapeutic Options. JPR. 2024 Aug;Volume 17:2657–66. [11] Chauhan G, Kodnani A. A study of prevalence and impact of dysmenorrhea and its associated symptoms among adolescent girls residing in slum areas of Vadodara city, Gujarat. Int J Med Sci Public Health. 2016;5(3):510. [12] Harlow SD, Campbell OMR. Epidemiology of menstrual disorders in developing countries: a systematic review. BJOG. 2004 Jan;111(1):6–16. [13] Osayande AS, Mehulic S. Diagnosis and initial management of dysmenorrhea. Am Fam Physician. 2014 Mar 1;89(5):341-6. PMID: 24695505. [14] Büssing A, Michalsen A, et.al ,Effects of yoga on mental and physical health: a short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. doi: 10.1155/2012/165410. Epub 2012 Sep 13. PMID: 23008738; PMCID: PMC3447533. [15] Omidvar S, Bakouei F, Amiri FN, Begum K. Primary Dysmenorrhea and Menstrual Symptoms in Indian Female Students: Prevalence, Impact and Management. GJHS. 2015 Dec 18;8(8):135. [16] Rakhshaee Z. Effect of Three Yoga Poses (Cobra, Cat and Fish Poses) in Women with Primary Dysmenorrhea: A Randomized Clinical Trial. Journal of Pediatric and Adolescent Gynecology. 2011 Aug;24(4):192–6. [17] Sakuma Y, Sasaki-Otomaru A, Ishida S, Kanoya Y, Arakawa C, Mochizuki Y, et al. Effect of a Home-Based Simple Yoga Program in Child-Care Workers: A Randomized Controlled Trial. The Journal of Alternative and Complementary Medicine. 2012 Aug;18(8):769–76. [18] Monika null, Uma Singh, Ghildiyal A, Kala S, Srivastava N. Effect of Yoga Nidra on physiological variables in patients of menstrual disturbances of reproductive age group. Indian J Physiol Pharmacol. 2012;56(2):161–7. [19] Rani M, Singh U, Agrawal GG, Natu SM, Kala S, Ghildiyal A, et al. Impact of Yoga Nidra on menstrual abnormalities in females of reproductive age. J Altern Complement Med. 2013 Dec;19(12):925–9. [20] Nag U, Kodali M. MEDITATION AND YOGA AS ALTERNATIVE THERAPY FOR PRIMARY DYSMENORRHEA. 2013;03. [21] Yang NY, Kim SD. Effects of a Yoga Program on Menstrual Cramps and Menstrual Distress in Undergraduate Students with Primary Dysmenorrhea: A Single-Blind, Randomized Controlled Trial. The Journal of Alternative and Complementary Medicine. 2016 Sep;22(9):732–8. [22] Yonglitthipagon P, Muansiangsai S, Wongkhumngern W, Donpunha W, Chanavirut R, Siritaratiwat W, et al. Effect of yoga on the menstrual pain, physical fitness, and quality of life of young women with primary dysmenorrhea. Journal of Bodywork and Movement Therapies. 2017 Oct;21(4):840–6. [23] Aggarwal A, Rao T, Palekar T, Paranjape P, Singh G. Effect of Yogasanas and Pranayama on Pain, Severity and Quality of Life in Primary Dysmenorrhea 2020 feb 06. [24] Kachapeswaran G, R. Elangovan. EFFECT OF YOGIC PRACTICES ON SELECTED RISK FACTORS AMONG ADOLESCENT GIRLS SUFFERING WITH DYSMENORRHEA [Internet]. Unpublished; 2022 [cited 2024 Nov 19]. Available from: https://rgdoi.net/10.13140/RG.2.2.28231.37280 [25] Haryono IR, Sudarman JP, Prastowo NA, Lilis L. The effect of Hatha Yoga on pain intensity in severe primary dysmenorrhea among students: A randomized controlled trial. JNKI. 2023 Apr 14;11(1):95. [26] Kulkarni DP. Effectiveness Of Yoga Therapy Ongirls (Age Group 14- 18 Years) With Primary Dysmenorrhea. (2581). [27] Deepika S, Jayanthi R, Parthiban V. Efficacy of Yoga on Primary Dysmenorrhea Among Adolescent Girls. Intern J Zool Invest. 2023;9(Special Issue 2):228–32. [28] Menstrual health & hygiene management (MHHM) survey & gap analysis report https://unesdoc.unesco.org/ark:/48223/pf0000385512 [29] Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med. 2000 Dec;154(12):1226–9. [30] MacGregor B, Allaire C, Bedaiwy MA, Yong PJ, Bougie O. Disease Burden of Dysmenorrhea: Impact on Life Course Potential. IJWH. 2023 Apr;Volume 15:499–509. [31] Durain D. Primary dysmenorrhea: assessment and management update. J Midwifery Womens Health. 2004;49(6):520–8. [32] Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020 Sep 1;161(9):1976–82. [33] De Sanctis V, Soliman A, Bernasconi S, Bianchin L, Bona G, Bozzola M, et al. Primary Dysmenorrhea in Adolescents: Prevalence, Impact and Recent Knowledge. Pediatr Endocrinol Rev. 2015 Dec;13(2):512–20. [34] Stewart K, Deb S. Dysmenorrhoea. Obstetrics, Gynaecology & Reproductive Medicine. 2014 Oct;24(10):296–302. [35] Åkerlund M. PATHOPHYSIOLOGY OF DYSMENORRHEA. Acta Obstet Gynecol Scand. 1979 Jan;58(S87):27–32. [36] Ju H, Jones M, Mishra G. The Prevalence and Risk Factors of Dysmenorrhea. Epidemiologic Reviews. 2014;36(1):104–13. [37] Visweswaraiah NK, Telles S. Randomized trial of yoga as a complementary therapy for pulmonary tuberculosis. Respirology. 2004 Mar;9(1):96–101. [38] Kanchibhotla D, Subramanian S, Singh D. Management of Dysmenorrhea Through Yoga: A Narrative Review. Front Pain Res. 2023 Mar 30;4:1107669. [39] Bhavanani, A.B. (no date) (PDF) yoga: The original mind body medicine. Available at: https://www.researchgate.net/publication/237077700_YOGA_THE_ORIGINAL_MIND_BODY_MEDICINE (Accessed: 17 December 2024). Programme Co-ordinator ACYTER, JIPMER, Pondicherry, India. [40] Çelik AS, Apay SE. Effect of progressive relaxation exercises on primary dysmenorrhea in Turkish students: A randomized prospective controlled trial. Complementary Therapies in Clinical Practice. 2021 Feb;42:101280. [41] Ko HN, Le SS, Kim SD. Effects of yoga on dysmenorrhea: a systematic review of randomized controlled trials. Alternative & Integrative Medicine. 2016;5(4):1-5. [42] Carolin BT, Maesari I, Hisni D. Yoga Exercise on Reduction of Menstrual Pain among Adolescent Girls. nhs. 2022 Apr 1;2(2):29–33. [43] Nespor K. Pain management and yoga. Int J Psychosom. 1991;38(1-4):76-81. PMID: 1723397. [44] C. McCall M. How might Yoga Work? An Overview of Potential Underlying Mechanisms. J Yoga Phys Ther [Internet]. 2013 [cited 2024 Dec 10];03(01). Available from: https://www.omicsonline.org/how-might-yoga-work-an-overview-of-potential-underlying-mechanisms-2157-7595.1000130.php?aid=12042 [45] Gupta S, Gautam S, Kumar U, Arora T, Dada R. Potential Role of Yoga Intervention in the Management of Chronic Non-malignant Pain. Anand V, editor. Evidence-Based Complementary and Alternative Medicine. 2022 May 28;2022:1–15.
Copyright
Copyright © 2025 Taruni Sarva, Avilash Mohapatra, Ganesh Kumar Subudhi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET66546
Publish Date : 2025-01-16
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

