Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
A Review on Post Pandemic Cardiac Arrests
Authors: Dr. G. Usha Kiran, D. Durga Prasad, SK. Khaja Mohiddin, B. Daniel, B. Ravi Teja, K. Gopi Varun
DOI Link: https://doi.org/10.22214/ijraset.2024.63607
Certificate: View Certificate
Abstract
The COVID-19 pandemic has profoundly impacted global healthcare systems, with a significant increase in cardiac arrests reported during and following the peak phases of infection. This review examines the epidemiology, pathophysiology, clinical characteristics, and outcomes of post-pandemic cardiac arrest. It explores the complex interplay between viral infection, systemic inflammation, and cardiovascular complications, highlighting key risk factors such as pre-existing comorbidities and delayed medical interventions. Furthermore, the review discusses the challenges faced by healthcare providers in managing cardiac arrest cases amidst pandemic-related disruptions in healthcare delivery and emphasizes the importance of tailored resuscitation protocols and post-resuscitative care strategies. Insights from this review underscore the need for proactive public health measures, robust healthcare infrastructure, and ongoing research to mitigate the long-term impact of pandemics on cardiovascular health.
Introduction
I. INTRODUCTION
Numerous infectious microbes, including viruses, bacteria, fungi, protozoa, and helminths, are present in the human body and can damage tissue through distinct systems. Among these five categories of infectious organisms, viruses are different due to their ability to specifically alter the host-cell apparatus and their constant evolution to thrive in all species [1].
In December 2019, an unusual respiratory illness emerged in Wuhan, China, quickly spreading beyond the city. It was determined that this outbreak was caused by a new type of coronavirus, named severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2 or 2019-nCoV). The illness caused by this virus was named Coronavirus Disease 2019 (COVID-19), and the World Health Organization (WHO) declared it a pandemic. COVID-19 has affected many people globally, with cases reported in nearly 200 countries and territories [2, 3].
As of April 7th, 2020, approximately 1.4 million cases have been reported globally, according to the Centre for Systems Science and Engineering (CSSE) at Johns Hopkins University.[4].
The viral family group that infects birds and mammals includes coronaviruses (CoV). "Corona Virus" is the term given to a pandemic new coronavirus disease 2019'' (2019-nCoV) in Geneva, Switzerland, by the World Health Organization (WHO). The 2019 coronavirus is now known as the SARSCoV-2 pandemic since its RNA pattern is more similar to that of SARS. It is a member of the realm Riboviria, order Nidovirales, family Coronaviridae, and subfamily Orthocoronavirinae.
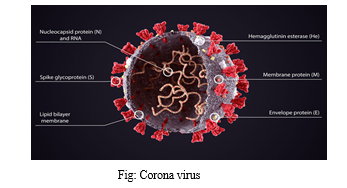
When Corona is viewed in two dimensions using transmission electron microscopy, the virions have a distinctive "crown-like" appearance. This led to the virus being named "Corona," which translates to "crown" or "halo" in Latin. It is a deadly third-generation virus belonging to the Corona family.
II. PATHOPHYSIOLOGY
Since the China outbreak, SARS-CoV-2 has become widespread worldwide. Early in April 2020, the United States had the largest reported number of COVID-19 patients, followed by Germany, France, Spain, Italy, and China. Italy was severely impacted by the China pandemic.
In the Chinese series, the mortality rate was likewise greater in the elderly population. According to the Italian report, the case-fatality rate was 7.2%. [5].
Based on data from February 2020, the Chinese Centre for Disease Control and Prevention (China CDC) reported that children under 10 years old and those between the ages of 11 and 19 accounted for 1% of all cases. [6].There is increasing interest in the relationship between COVID-19 severity and gender. While the data showed an equal number of cases between males and females, it suggested that more men experienced severe disease and fatalities. Adverse COVID-19 outcomes were linked to comorbidities like hypertension, cardiovascular disease, and lung disease, which are more common in men and associated with smoking and alcohol consumption. Additionally, studies on protective behaviours during pandemics found that women were about 50% more likely than men to engage in behaviours such as hand washing, mask-wearing, and avoiding crowds, which may contribute to the differences in outcomes. [7].
III. MECHANISM
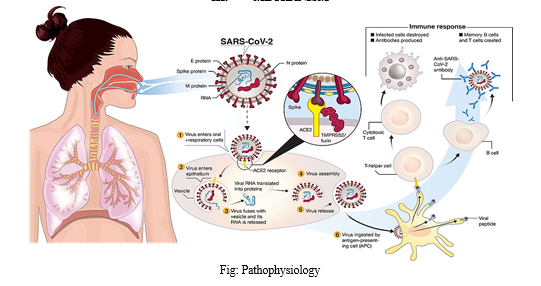
Coronaviruses are enveloped, positive-sense, single-stranded RNA viruses with genomes of approximately 30kb, capable of infecting a wide range of host species. The α and β coronaviruses infect only mammals. In contrast, SARS-CoV, Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2 are classified as β coronaviruses. The virus life cycle within a host involves five steps: attachment, penetration, biosynthesis, maturation, and release. During attachment, the viruses bind to host receptors. They then enter host cells via endocytosis or membrane fusion (penetration). Once inside, viral RNA is released and enters the nucleus for replication. Viral mRNA is used to produce viral proteins (biosynthesis), new viral particles are assembled (maturation), and then they are released from the host cell. Coronaviruses consist of four structural proteins: Spike (S), membrane (M), envelope (E), and nucleocapsid (N) [8].
IV. SYMPTOMS
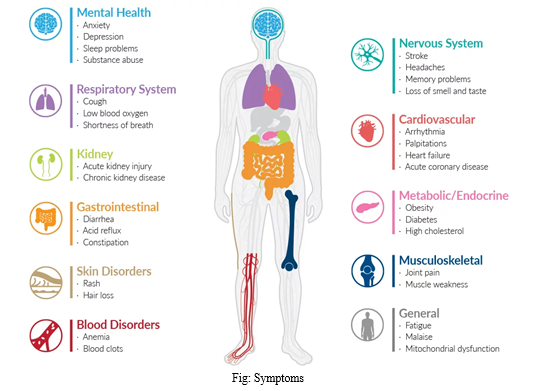
COVID-19 patients exhibit a wide spectrum of symptoms, ranging from mild to moderate, severe, rapidly progressing, and even fulminant disease. The symptoms are non-specific, and the disease can present as anything from asymptomatic to severe pneumonia. Asymptomatic cases account for 1.6% to 51.7% of infections, with these individuals showing no typical clinical signs or lung abnormalities on computed tomography scans. The most common symptoms include fever, cough, muscle pain (myalgia), or fatigue.
Less common symptoms are sputum production, headache, coughing up blood (hemoptysis), vomiting, and diarrhea. Some patients may experience sore throat, runny nose (rhinorrhoea), headache, and confusion before developing a fever, suggesting that while fever is a critical symptom, it may not be the initial sign of infection. Additionally, some patients report a loss of smell (hyposmia) or taste (hypogeusia), which are now recognized as early warning signs and indications for self-isolation. More severe and rare neurological complications such as strokes, brain inflammation, delirium, and nerve damage [9]
V. EFFECTS ON HEART
SARS-CoV-2 infection can harm the heart directly and has a remarkable capacity to infect cardiomyocytes derived from induced pluripotent stem cells, resulting in a unique pattern of heart muscle cell fragmentation characterized by the "complete dissolution of the contractile machinery." [10].
SARS-CoV-2 infection caused apoptosis and halted beating within 72 hours of exposure. A secondary immune response to the infected heart and endothelial cells (enthesitis) is one of many possible indirect effects. These include dysregulation of the renin-angiotensin-aldosterone system, which controls blood pressure, and the activation of a proinflammatory response involving platelets, neutrophils, macrophages, and lymphocytes, leading to cytokine release and a prothrombotic state. Clotting tendencies in both small and large blood vessels have been reported in multiple autopsy studies and in young COVID-19 patients who have suffered strokes.
COVID-19 presents a wide range of cardiovascular manifestations, from limited necrosis of heart cells (causing injury) to myocarditis and cardiogenic shock (a potentially fatal inability to pump sufficient blood). Cardiac injury, as indicated by elevated levels of troponin (a cardiac muscle-specific enzyme) in the blood, is common with COVID-19. This myocardial injury is a risk factor for in-hospital mortality, and troponin levels correlate with mortality risk. Moreover, patients with higher troponin levels show markers of increased inflammation [including C-reactive protein, interleukin-6 (IL-6), ferritin, lactate dehydrogenase (LDH), and high neutrophil count] and heart dysfunction (amino-terminal pro–B-type natriuretic peptide).
Extensive heart muscle damage can lead to heart failure, acute cor pulmonale (right heart failure and possible pulmonary emboli), and cardiogenic shock.
Recent studies of COVID-19 patients undergoing magnetic resonance imaging (MRI) or echocardiography have provided new insights into cardiac involvement. [11-15].
In contrast, many individuals suffer from long-COVID, a prolonged, often debilitating illness with symptoms like fatigue, difficulty breathing, chest pain, and abnormal heart rhythms. An immunologic basis is likely but not yet determined. These patients have not undergone systematic cardiovascular assessment for myocarditis or other heart abnormalities like fibrosis, which could explain some enduring symptoms.
An intriguing question is why certain individuals are prone to heart involvement after SARS-CoV-2 infection. Initially, it was expected that cardiac involvement would mainly occur in patients with severe COVID-19, but it is more common than anticipated, though the true incidence remains unknown. Understanding the cause is crucial, whether it’s an individual’s inflammatory response, an autoimmune phenomenon, or another explanation. The marked heterogeneity of COVID-19, ranging from asymptomatic cases to fatalities, is poorly understood. This newly emerged virus, circulating widely in the human population with a range of often hidden disease manifestations, has made this particularly challenging to unravel [16]
VI. POST PANDEMIC CARDIAC ARRESTS
During the COVID-19 pandemic, several global geographic locations reported a significant increase in the frequency of out-of-hospital cardiac arrests (OHCA) [17].
In the United States, various regions observed increases in out-of-hospital cardiac arrest (OHCA) rates during the COVID-19 pandemic. Rollman et al. reported a 21% rise in OHCA incidence in Los Angeles County, CA, which has a diverse population of around 10.1 million people. Matthew et al. noted a 62% increase in Detroit, MI, using data from the Cardiac Arrest Registry to Enhance Survival (CARES). Lai et al. documented approximately a threefold higher incidence of OHCA in New York City, NY, a heavily impacted area early in the pandemic with one of the largest EMS systems in the US, serving about 8.4 million people.
Similarly, in Europe, Baldi et al. analyzed data from the Lombardi Cardiac Arrest Registry covering four provinces in Italy and found a 58% increase in OHCA. Marion et al. reported a twofold increase in Paris, France, and its suburbs. A meta-analysis by Lim et al. A 120% increase in OHCA was observed in many investigations encompassing over 35,000 OHCA incidents.
In contrast, several studies did not find significant increases in OHCA rates. Huber et al. found no significant rise in a German community with low COVID-19 prevalence. Elmer et al. similarly reported no significant increase in Pennsylvania, USA, where COVID-19 prevalence was low. Chan et al. observed that OHCA incidence was higher in communities with high COVID-19 mortality rates, suggesting a correlation between OHCA incidence and COVID-19 prevalence in those areas.
Overall, while these studies suggest a link between OHCA incidence and COVID-19 infection rates in communities, they do not imply that most OHCA patients were COVID-19 positive.
Among patients experiencing OHCA during the COVID-19 pandemic, there were also significant alterations in baseline patient characteristics. In contrast to a pre-pandemic control group, Lai et al. observed that OHCA patients were older, less likely to be White, and more likely to have concomitant illnesses like hypertension and diabetes mellitus. Nonshockable cardiac rhythms (asystole and pulseless electrical activity) were also more common during this period.
Further investigations into the relationship between COVID-19 and the initial cardiac arrest rhythm revealed that patients confirmed to have COVID-19 were less likely to present with a shockable rhythm compared to those who tested negative for COVID-19.
The ineffectiveness of bystander CPR in improving survival outcomes when EMS response times are prolonged is likely due to issues such as inadequate sternal compressions in 50% of OHCA cases, delayed initiation of compressions, and the lack of strategies to prevent asphyxial cardiac arrest and facilitate unobstructed gasping, which are critical for improving neurological outcomes Recent proposals include using the 4-finger method for sternal compression to maximize effectiveness and advocating for immediate application without delays caused by instructions to remove clothing or repositioning the patient Additionally, techniques like head rotation to maintain an open airway without hands-on intervention are recommended based on evidence to support better survival outcomes [18].
Animal studies suggest that partially obstructed gasping with room air, which likely affects about 54% of OHCA victims [19], leads to significantly reduced and less effective arterial oxygenation and gasping frequency. The incidence of unobstructed gasping also diminishes greatly if ventricular fibrillation remains untreated for more than 3 minutes; only about 8% of animals remain gasping after approximately 8 minutes, which aligns with the average EMS response time. Head rotation is necessary to notably increase the occurrence of unobstructed gasping by the time EMS arrives, a response time that typically ranges from 6 to 10 minutes in the post-COVID-19 era.
Employing chest compressions using the 4-finger technique without exposing the chest or moving the victim from a supine position on a soft surface to a hard flat surface or floor is crucial to prolong and enhance the frequency of unobstructed gasping so that it is present upon EMS arrival. Oxygen administration during CPR is also critical for promoting spontaneous gasping based on experimental findings [20]
VII. IMPACT OF COVID 19 IN DIFFERENT AGE GROUPS
A. Effect of COVID-19 in Children
According to a study by the Chinese Disease Control Centre, only 2% of people under 20 have been affected by COVID-19. The study analyzed three groups of infected children: 20 from Zhejiang, 37 from Shenzhen, and 9 from various other regions in China. The majority of cases were from the second group, with 65% showing respiratory symptoms and some experiencing diarrhoea, headaches, poor feeding, bluish skin discoloration, and difficulty breathing in severe cases. The third group reported fever in four infants. Nearly all symptomatic children recovered within a short time, and no deaths have been reported among children infected with COVID-19.
It was observed that although adolescents are vulnerable to COVID-19 infection, younger children tend to exhibit milder symptoms compared to those aged 12-19. The 12-19 age group was followed in clinical studies, which showed a decline in their condition. Studies on MERS infection, which mainly affects adults, also reported some pediatric cases. Similarly, for SARS and COVID-19, most infected children were asymptomatic. Diagnoses were often made when an adult family member was screened for MERS infection.
Even though there were few cases of children with COVID-19, they were likely carriers of the virus. Children are susceptible to SARS-CoV-2 but typically do not show noticeable symptoms, potentially acting as intermediaries in virus transmission. Public health strategies, such as avoiding contact with elderly individuals, are recommended to protect vulnerable populations. Asymptomatic "silent carriers" could spread the virus to larger groups undetected. It appears that adolescents might not be as susceptible to severe COVID-19 as previously thought. [21].
B. Effect of COVID-19 in Young Adult
Reports indicate that children tend to exhibit fewer and milder symptoms compared to middle-aged individuals during a COVID-19 outbreak. This often leads to misdiagnosis or missed diagnosis since children with mild or no symptoms might not undergo essential COVID-19 testing. Consequently, an infected child may test negative on throat and nose swabs. However, most infected children were part of household clusters, similar to previous SARS and MERS outbreaks, where 50-80% and 32% of paediatric cases, respectively, were due to family contact.
Children are as likely as adults to contract SARS-CoV-2, but they usually show milder or no symptoms, according to a study published in March 2020. The role of children in spreading the virus is still not fully understood. Additionally, there is no evidence of vertical transmission of SARS-CoV-2 from mother to newborn.
C. Effect of COVID-19 in older population
Although the severity of COVID-19's impacts is still unknown, it is certain that it has a negative impact on mental health. Early studies report increased anxiety and depression, particularly among those facing prolonged lockdowns. These effects are more pronounced in the elderly due to strict lockdowns, higher health risks, and lack of support. Previous research also indicated that older adults experienced more severe symptoms during disease outbreaks, with those having pre-existing mental health conditions being particularly vulnerable.
The rise in mental health issues is concerning not only for the general population but also for the elderly, as cognitive decline in this group is linked to decreased academic performance and a higher risk of Alzheimer’s disease. This suggests that while societies deal with immediate mental health challenges, the long-term consequences could be severe, with increased rates of cognitive decline and Alzheimer's among older adults. The enforced restrictions on movement reduce exercise opportunities, which are crucial for mental health, especially in older adults with cognitive impairments or neuropsychiatric issues.[22]
Loss of social interaction, increased mental stress, and decreased physical activity could have significant adverse effects on the elderly. Although lockdowns may be temporary, their impact on the quality of life for older people could be long-lasting and substantial.The COVID-19 pandemic has led to significant changes globally, including reduced social interaction and prolonged periods of grief.
Lockdowns have drastically altered daily life and restricted access to regular healthcare services, as facilities became overwhelmed with COVID-19 patients. This has increased health risks, especially for the elderly, who have more medical issues and are advised to avoid potentially infectious areas. [23].
There has been a shift towards telehealth to provide medical care safely. However, this transition has been less effective for older adults, with over 40% unable to use telehealth resources due to a lack of necessary skills. Studies showed that telemedicine was most used by those aged 20-44, despite the elderly having the highest number of medical visits annually. Attempts to create interactive geriatric clinics during the pandemic have had mixed results due to technological challenges.
This digital revolution isn't restricted to healthcare; it impacts education, delivery of food online, and COVID-19 news access. While many have adapted successfully, the older generation struggles with slower internet access and less familiarity with technology.
Consequently, those most affected by the pandemic are often the least able to use resources designed to mitigate its impact, highlighting a digital divide between older and younger populations.
D. Impact of COVID-19 pandemic on chronic diseases
Most chronic diseases are silent killers. According to a 2018 WHO report, 63% of deaths were due to chronic illnesses such as heart disease, diabetes, cancer, and respiratory diseases. Currently, the global mortality rate from non-communicable diseases (NCDs) is alarmingly high. Three-quarters of all fatalities worldwide are expected to be linked to NCDs by 2030 [24].
Severe issues are more likely to develop in COVID-19 patients with diabetes, hypertension, and coronary heart disease.
Those with cardiovascular diseases (CVDs) face a higher risk of mortality. Providing routine care for chronic diseases during the pandemic has been particularly challenging [25]
Chronic conditions such as HIV, diabetes, and kidney diseases lead to immunosuppression, increasing patients' susceptibility to infections. Individuals suffering from these chronic diseases who contract COVID-19 have a lower likelihood of recovery. Additionally, COVID-19 is a significant contributor to heart disease, accounting for approximately 5% of acute heart failure cases. Consequently, the mortality rate is elevated among COVID-19 patients with a history of cardiovascular disease (CVD) [26].
Patients diagnosed with asthma and chronic obstructive pulmonary disease (COPD) face varying risks of severe COVID-19, possibly linked to differing activation levels of ACE2 receptors. To achieve improved outcomes and monitoring, it is crucial for patients with chronic diseases to receive prompt and effective access to care. Furthermore, individuals with chronic conditions necessitate ongoing follow-up to effectively manage their health.
The impact of chronic diseases is increasingly significant in low-income countries. Over 80% of deaths from heart disease and diabetes, and nearly 90% of deaths from chronic obstructive pulmonary disease, occur in low- and middle-income countries (LMICs). Heart disease is the leading cause of death worldwide, with an estimated annual death toll exceeding 17.3 million. According to the WHO, out of the 38 million annual deaths from chronic diseases, approximately 14 million occur in individuals aged 30-70 years, with 85% of these deaths happening in developing countries [27].
Conclusion
In conclusion, the COVID-19 pandemic has starkly illustrated the intersection of infectious disease and cardiovascular health, with a notable increase in cardiac arrest cases observed during and after the pandemic\'s peak. The pathophysiological mechanisms linking viral infection to cardiovascular complications, including myocardial injury and arrhythmogenesis, underscore the need for heightened vigilance in at-risk populations. Challenges in healthcare delivery, ranging from resource constraints to altered treatment paradigms, have necessitated innovative approaches in cardiac arrest management and resuscitative efforts. Moving forward, integrating lessons learned from this crisis into public health policies, clinical guidelines, and healthcare preparedness strategies will be crucial in mitigating the impact of future pandemics on cardiovascular outcomes. Continued research efforts focusing on optimal resuscitation strategies, post-resuscitative care pathways, and long-term cardiovascular sequelae are essential to improve outcomes for individuals affected by post-pandemic cardiac arrest.
References
[1] Almutairi MA. The coronavirus disease 2019 (COVID-19) outbreak: Challenges for paediatric dentistry. J Res Med Dent Sci 2021, 9:116-121 [2] M. Zheng, Y. Gao, G. Wang, G. Song, S. Liu, D. Sun, Y. Xu, Z. Tian, Functional exhaustion of antiviral lymphocytes in COVID-19 patients, Cell Mol Immunol. (2020), https://doi.org/10.1038/s41423-020-0402-2. [3] J. Zhang, M. Litvinova, W. Wang, Y. Wang, X. Deng, X. Chen, M. Li, W. Zheng, L. Yi, X. Chen, Q. Wu, Y. Liang, X. Wang, J. Yang, K. Sun, I.M. Longini Jr., M.E. Halloran, P. Wu, B.J. Cowling, S. Merler, C. Viboud, A. Vespignani, M. Ajelli, H. Yu, Evolving epidemiology and transmission dynamics of coronavirus disease 2019 outside Hubei province, China: a descriptive and modelling study, Lancet Infect Dis. (2020), K. Yuki, et al. [4] JHUoMCrcenter, Journal (2020), https://coronavirus.jhu.edu/map.html [5] G. Onder, G. Rezza, S. Brusaferro, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy, JAMA (2020), https://doi.org/10.1001/ jama.2020.4683. [6] Z. Wu, J.M. McGoogan, Characteristics of and important lessons from the Coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Centre for Disease Control and Prevention, JAMA (2020), https://doi.org/10.1001/jama.2020.2648 [7] N. Chen, M. Zhou, X. Dong, J. Qu, F. Gong, Y. Han, Y. Qiu, J. Wang, Y. Liu, Y. Wei, J. Xia, T. Yu, X. Zhang, L. Zhang, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet 395 (2020) 507–513 [8] R. Channappanavar, J. Zhao, S. Perlman, T cell-mediated immune response to respiratory coronaviruses, Journal 59 (2014) 118–128. [9] Dane S, Akyuz M. Symptom spectrum and the evaluation of severity and duration of symptoms in patients with COVID-19. J Res Med Dent Sci 2021; 9:262-266. [10] J. A. Perez-Bermejo et al., bioRxiv 265561, (2020) [11] A. Sharma et al., Cell Rep. Med. 10.1016/j.xcrm. 2020.100052 (2020). [12] R. O. Bonow, G. C. Fonarow, P. T. O’Gara, C. W. Yancy, JAMA Cardiol. 5, 751 (2020). [13] E. Baldi et al., LombardiaCARe Researchers, N. Engl. J. Med.383, 496 (2020). [14] S. Shaigany et al., Lancet396, e8 (2020). [15] V. O. D. Puntmann et al., JAMA Cardiol. 10.1001/ jamacardio.2020.3557 (2020). [16] M. R. Dweck et al., Eur. Heart J. 21, 949 10.1093/ehjci/ jeaa178 (2020). [17] Rollman JE, et al. Emergency medical services re sponses to out-of-hospital cardiac arrest and sus pected ST-segment-elevation myocardial infarction during the COVID-19 pandemic in Los Angeles county. J Am Heart Assoc 2021;10(12): e019635 [18] Cournoyer A, Grunau B, Cheskes S, Vaillancourt C, Segal E, de Montigny L, et al. Clin icaloutcomes following out-of-hospital cardiac arrest: the minute-by-minute im pact of bystander cardiopulmonary resuscitation. Resuscitation. 2023 Jan 13:109693. https://doi.org/10.1016/j.resuscitation.2023.109693. [19] Tanu Singhal. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr 2020; 87:281–286. [20] Safar P, EscarragaLA, Chang F. Upper airway obstruction in the unconscious patient. J Appl Physiol. 1959 Sep;14:760–4. [21] Ahmed MZ, Ahmed O, Aibao Z, et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr 2020; 51:102092. [22] Meda N, Pardini S, Slongo I, et al. COVID-19 and depressive symptoms in students before and during lockdown. MedRxiv 2020. [23] Lazzerini M, Barbi E, Apicella A, et al. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020; 4:e10–11. [24] (NCDs): a silent scourge threatening to overwhelm global health. Advancing Science for Global Health 2011; 10: 7-13. [25] Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S and Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr 2020; 14: 965-7. [26] McDonald HI, Thomas SL and Nitsch D. Chronic kidney disease as a risk factor for acute community-acquired infections in high-income countries: a systematic review. BMJ Open 2014; 4. e004100 [27] Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, De Ferranti S, Després JP, Fullerton HJ and Howard VJ. Heart disease and stroke statistics-2016 update: a report from the american heart association. Circulation 2016; 133: e38-e360.
Copyright
Copyright © 2024 Dr. G. Usha Kiran, D. Durga Prasad, SK. Khaja Mohiddin, B. Daniel, B. Ravi Teja, K. Gopi Varun. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET63607
Publish Date : 2024-07-11
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

