Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Advancements in Adolescent Idiopathic Scoliosis Diagnosis: A Focus on Non-Invasive Techniques
Authors: Aastha Singh, Amit Kumar Shukla, Anjali Prasad, Leimapokpam Tinashi Devi, Mrs. Savitha P
DOI Link: https://doi.org/10.22214/ijraset.2024.58911
Certificate: View Certificate
Abstract
Adolescent idiopathic scoliosis (AIS) poses a significant health concern, affecting the spinal curvature of adolescents during their growth period. Early diagnosis of AIS is critical for effective intervention and management. However, conventional diagnostic methods often involve repetitive exposure to X-rays, which can lead to radiation-related side effects. This research paper explores the significance of early diagnosis in AIS and emphasizes the utilization of non-invasive techniques, particularly video raster stereography (VRS), combined with deep ensemble neural networks (DNNs) to enhance diagnostic accuracy while minimizing the risks associated with radiation exposure. We delve into the potential of DNNs in analyzing VRS data and compare its efficacy with other machine learning alternatives.
Introduction
I. INTRODUCTION
Scoliosis manifests as a spinal condition characterized by lateral curvature and vertebral rotation. Its origins span a spectrum of causes, including congenital, neuromuscular, syndrome-related, idiopathic, and secondary factors. Among these, idiopathic scoliosis is predominant in clinical settings, presenting a diverse natural history shaped by etiology and age at onset, thus guiding treatment strategies. Crucially, initial evaluation hinges on patient history, physical examination, and radiographic assessment, with particular emphasis on identifying non-idiopathic cases for targeted intervention. For instance, congenital scoliosis necessitates scrutiny for associated cardiac and renal anomalies. While school-based screening once held sway, its efficacy now faces scrutiny.
Treatment protocols for idiopathic scoliosis are multifaceted, contingent upon factors such as age, curve severity, and risk of progression. Options encompass observation, orthotic management, and surgical fusion. Notably, referral to a specialist is warranted if the curvature exceeds 10° in patients younger than 10 years, or surpasses 20° in older patients. Additional indications include atypical features, back pain, or neurological symptoms. This paper elucidates the dynamic realm of scoliosis diagnosis, highlighting innovations that enhance precision while mitigating inherent risks.
II. LITERATURE REVIEW
Caesarendra et al. (2022) develop a Convolutional Neural Network (CNN)-based system for automated Cobb angle measurement in Adolescent Idiopathic Scoliosis. Their study highlights the CNN's accuracy, offering a promising tool for efficient scoliosis diagnosis and monitoring.
Yahara et al. (2022) piloted a deep convolutional neural network to forecast curve progression in Adolescent Idiopathic Scoliosis, showing potential for early detection and treatment planning.
Yip et al. (2020) systematically analyze non-surgical treatments for Adolescent Idiopathic Scoliosis (AIS) through a comprehensive literature review and citation network analysis, aiming to provide insights into the efficacy of various non-invasive interventions.
Anthony et al.'s (2020) study identifies trends in detection and referral of Adolescent Idiopathic Scoliosis (AIS), highlighting challenges in effective treatment due to skeletal maturity and late presentations.
Sekiya et al. (2018) investigate leg length discrepancies in AIS patients, showing functional discrepancies correlated with pelvic obliquity and lumbar Cobb angle.
Dufvenberg et al. (2018) conduct a meta-analysis, indicating decreased postural stability in AIS patients compared to typically developed individuals, emphasizing the importance of studying postural stability in AIS.
Sitoula et al. (2015) validate the Sanders Skeletal Maturity Staging System for predicting curve progression in idiopathic scoliosis, highlighting its strong correlation with initial Cobb angle.
Schimmel et al. (2015) explore treatment options for Adolescent Idiopathic Scoliosis (AIS), including bracing and surgical techniques, while addressing debates around screening efficacy and intervention outcomes.
Komeili et al. (2015) utilize 3D marker-less surface topography for scoliosis monitoring, potentially reducing X-ray requirements through early detection of curve progression.
Schlösser et al. (2014) conduct a systematic review on associated abnormalities in AIS, revealing limited evidence and weak associations, highlighting the challenge in understanding its etiology.
Weinstein et al. (2013) respond to the efficacy of bracing in reducing high-risk curve progression in Adolescent Idiopathic Scoliosis (AIS), emphasizing the role of brace wear duration in achieving successful outcomes.
Paolucci et al.'s (2013) case-control study at Policlinico Umberto I Hospital found that scoliosis patients had higher instability than healthy controls, but wearing a Chêneau brace improved stability, especially in limb load symmetry, sway length, and velocity.
Sahlstrand et al. (2013) examine bone quality profiles in AIS patients, revealing unique changes in trabecular compartments associated with osteopenia.
Lao et al. (2008) explore the impact of somatosensory dysfunction on dynamic balance in AIS, suggesting a link between somatosensory issues and balance control.
Danielsson et al. (2007) present a long-term follow-up study on AIS patients treated primarily with bracing, demonstrating stable curves without surgeries compared to those in the observation group.
Lenke et al. (2001) propose a new classification system for AIS to determine the extent of spinal arthrodesis, highlighting the need for further studies to evaluate its applicability.
Pruijs et al. (1994) assess the reliability of Cobb angle measurement in scoliosis management, emphasizing the importance of standardizing radiograph production.
Morrissy et al. (1990) analyze Cobb angle measurements in scoliosis radiographs, revealing intraobserver and interobserver variability.
Herman et al. (1985) explore the link between impaired axial motor control and idiopathic scoliosis, indicating a high correlation with curve magnitude in vestibular processing variables.
Beekman & Hall (1979) highlight variability in scoliosis measurements, emphasizing the need to distinguish actual changes from measurement variability in exercise programs.
Sahlstrand et al. (1978) study postural control in AIS patients, showing poorer postural control compared to healthy children, with left convex patients exhibiting more pronounced instability.
III. METHODOLOGY
A. Modules
- Numpy: NumPy is a fundamental library for numerical computing in Python. It provides support for multi-dimensional arrays and matrices, along with a wide range of mathematical functions to operate on these arrays efficiently.
- Pandas: Panda is a powerful library for data manipulation and analysis. It offers high-level data structures like DataFrame and Series, which allow for easy indexing, selection, and filtering of data. Pandas is particularly useful for handling tabular data and time series data
- Scikit-learn: It provides a wide range of algorithms for various machine learning tasks, including classification, regression, clustering, dimensionality reduction, and more. It also offers tools for data preprocessing, model evaluation, and model selection.
B. Ensemble Learning Algorithms and Model Training Techniques
- Ensemble Deep Learning: Multiple neural network models are combined to classify scoliosis and healthy subjects based on Video-Raster-Stereography (VRS) data. Each model contributes to the final prediction, enhancing accuracy and robustness.
- Binary Crossentropy Loss Function: It measures the disparity between predicted probabilities and actual binary labels during model training, aiding in learning optimal classification boundaries for scoliosis detection.
- Adam Optimizer: This optimization algorithm adjusts the learning rate for each parameter individually, facilitating faster convergence and improved performance of the neural network models.
- Early Stopping: Implemented as a regularization technique, early stopping monitors model performance on a validation set and halts training if no improvement is observed, preventing overfitting and enhancing generalization.
- Balanced Accuracy Score: It evaluates the ensemble model's performance by considering class imbalances in the dataset, providing a reliable measure of classification accuracy for scoliosis severity prediction.
C. Steps of Implementation
- Data Collection and Preprocessing: Acquired Video-Raster-Stereography (VRS) data from subjects diagnosed with Adolescent Idiopathic Scoliosis (AIS) and healthy individuals. Conducted thorough cleaning and exploratory data analysis (EDA) to ensure data reliability and understand its distribution.
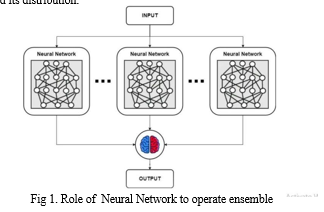
2. Ensemble Deep Learning Model Construction: Developed an Ensemble Neural Network using Keras, comprising multiple Multi-Layer Perceptron (MLP) neural networks with two hidden layers of 64 neurons each.
3. Model Training and Evaluation: Trained the Ensemble Neural Network on a balanced dataset containing both healthy and scoliotic subjects. Assessed model performance using metrics like balanced accuracy, considering sensitivity and specificity.
4. Implementation, Testing, and Validation: Implemented the model using Python and Keras, emphasizing usability, and conducted extensive testing on new data. Compared model performance with existing diagnostic methods and validated accuracy against established approaches
5. Optimization and Documentation: Explored techniques to enhance model efficiency, fine-tuned hyperparameters for optimal performance, and thoroughly documented the entire process for transparency and reproducibility.
6. Results Analysis and Application: Analyzed results to showcase the model's significance in improving diagnostic accuracy for scoliosis and explored potential real-world applications.
IV. FUTURE SCOPE
In the future, the research endeavors to delve deeper into the integration of deep ensemble neural networks (DNNs) with non-invasive techniques such as video raster stereography (VRS) to achieve even higher levels of diagnostic accuracy in adolescent idiopathic scoliosis (AIS). Further advancements in artificial intelligence (AI) and computer vision algorithms will be explored to refine the analysis of VRS data, potentially uncovering subtle patterns and markers for early detection and precise classification of AIS.
Longitudinal studies will validate the effectiveness of these techniques in real-world settings. User-friendly software and mobile apps can enable remote monitoring and proactive patient care. Collaboration and innovation will lead to personalized and effective adolescent idiopathic scoliosis management.
Conclusion
This paper underscores the critical need for early diagnosis of adolescent idiopathic scoliosis (AIS) while mitigating the risks associated with radiation exposure. We advocate for the adoption of non-invasive techniques like video raster stereography (VRS) coupled with deep ensemble neural networks (DNNs) to achieve higher diagnostic precision. Through an extensive review of existing literature and a detailed methodology, we highlight the potential of machine learning algorithms in automating the classification of scoliosis and predicting its progression. Our study not only explores the current landscape of AIS diagnosis but also offers practical insights into the development and application of advanced diagnostic tools. By leveraging ensemble learning and optimizing model training techniques, we demonstrate the feasibility of integrating these innovative approaches into clinical settings. Looking ahead, collaborative efforts and ongoing refinements in algorithmic methodologies will be pivotal in realizing the full potential of these non-invasive techniques, ultimately enhancing patient care and treatment outcomes in AIS management.
References
[1] Yip, Joanne, Jason Pui-Yin Cheung, Kenneth M C Cheung, and Kenny Kwan. \"Non-Invasive Treatment of Adolescent Idiopathic Scoliosis: Systematic Literature Review by Using Citation Network Analysis.\" (2020). [2] Anthony, Alison, Reinhard Zeller, Cathy Evans, and Jennifer Dermott. \"Adolescent idiopathic scoliosis detection and referral trends: impact treatment options.\" (2020). [3] Guan, Tianmin, Yufang Zhang, Adeel Anwar, and Yufen Zhang. \"Determination of Three-Dimensional Corrective Force in Adolescent Idiopathic Scoliosis and Biomechanical Finite Element Analysis.\" (2020). [4] Kelly, John J., Neil V. Shah, and Taylor Freetly. \"Treatment of adolescent idiopathic scoliosis and evaluation of the adolescent patient.\" (2018). [5] Sitoula, Prakash, Kushagra Verma, and Laurens Holmes. \"Prediction of Curve Progression in Idiopathic Scoliosis: Validation of the Sanders Skeletal Maturity Staging System.\" (2015). [6] Schimmel, Janneke J.P., Brenda E. Groen, Vivian Weerdesteyn, and Marinus De Kleuver. \"Adolescent idiopathic scoliosis and spinal fusion do not substantially impact on postural balance.\" (2015). [7] Komeili, Amin, Lindsey M. Westover, Eric C Parent, and Marwan El-Rich. \"Monitoring for Idiopathic Scoliosis Curve Progression Using Surface Topography Asymmetry Analysis of the Torso in Adolescents.\" (2015). [8] Weinstein, Stuart L., Lori Ann Dolan, and James Wright. \"Effects of Bracing in Adolescents with Idiopathic Scoliosis Reply.\" (2013). [9] Paolucci, Teresa, Giovanni Morone, and Annalisa Di Cesare. \"Effect of Chêneau brace on postural balance in adolescent idiopathic scoliosis: A pilot study.\" (2013). [10] Danielsson, Aina J., Ralph Hasserius, Acke Ohlin, and Alf L. Nachemson. \"A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis - A follow-up mean of 16 years after maturity.\" (2007). [11] Abreu, Daniela C., Matheus Machado Gomes, Hildemberg Santiago, and Carlos Fernando P. S Herrero. \"What is the influence of surgical treatment of adolescent idiopathic scoliosis on postural control?\" [12] Lenke, Lawrence G., Randal R. Betz, Jürgen Harms, and Keith H. Bridwell. \"Adolescent Idiopathic Scoliosis: A New Classification to Determine Extent of Spinal Arthrodesis.\" (2001). [13] Bustamante, Karla, Jason Thomas Long, and A Graf. \"Analysis of postural stability following posterior spinal fusion in adolescents with idiopathic scoliosis.\" [14] St-Georges, Maxime, Alisson R. Teles, Oded Rabau, and Neil Saran. \"Adolescent idiopathic scoliosis: Evaluating perioperative back pain through a simultaneous morphological and biomechanical approach.\" (2020). [15] Dufvenberg, Marlene, Fisayo Adeyemi, and Birgitta Oberg. \"Does postural stability differ between adolescents with idiopathic scoliosis and typically developed? A systematic literature review and meta-analysis.\" (2018). [16] Schlösser, Tom P.C., Geert J.M.G. van der Heijden, Anne L Versteeg, and Rene Marten Castelein. \"How ‘Idiopathic’ Is Adolescent Idiopathic Scoliosis? A Systematic Review on Associated Abnormalities.\" (2014). [17] Lao, May, Daniel HK Chow, Xia Guo, and Jack C Y Cheng. \"Impaired Dynamic Balance Control in Adolescents With Idiopathic Scoliosis and Abnormal Somatosensory Evoked Potentials.\" (2008). [18] Sahlstrand, Tage, Roland Örtengren, and Alf Nachemson. \"Postural Equilibrium in Adolescent Idiopathic Scoliosis.\" (1978). [19] Herman, Richard, James Mixon, Anne Fisher, and Ruth Maulucci. \"Idiopathic Scoliosis and the Central Nervous System: A Motor Control Problem.\" (1985). [20] Sahlstrand, Tage, Roland Örtengren, and Alf Nachemson. \"Abnormal bone quality versus low bone mineral density in adolescent idiopathic scoliosis: A case-control study with in vivo high-resolution peripheral quantitative computed tomography.\" (2013). [21] Beekman, Claire E. and Vivian Hall (1979). \"Variability of Scoliosis Measurement from Spinal Roentgenograms.\" [22] Morrissy, R T., G S Goldsmith, E C Hall, and D Kehl. \"Measurement of the Cobb angle on radiographs of patients who have scoliosis.\" (1990). [23] Sekiya, Tatsuhiro, Yoichi Aota, and Kanichiro Kaneko. \"Evaluation of functional and structural leg length discrepancy in patients with adolescent idiopathic scoliosis using the EOS imaging system.\" (2018). [24] Shen, Jesse, Samuel Kadoury, Hubert Labelle, and Marjolaine Roy-Beaudry. \"Geometric Torsion in Adolescent Idiopathic Scoliosis.\" (2017). [25] Pruijs, Hans from University Medical Center Utrecht and M. A. P. (1994). \"Variation in Cobb angle measurements in scoliosis.\"
Copyright
Copyright © 2024 Aastha Singh, Amit Kumar Shukla, Anjali Prasad, Leimapokpam Tinashi Devi, Mrs. Savitha P. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET58911
Publish Date : 2024-03-10
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

