Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Enhancing Cancer Care: Augmented and Virtual Reality Solutions
Authors: Harshwardhan Chourasia, Jaykumar S. Karnewar
DOI Link: https://doi.org/10.22214/ijraset.2024.60345
Certificate: View Certificate
Abstract
The present research delves into the various uses of augmented reality (AR) and virtual reality (VR) in cancer therapy, emphasizing their capacities as inventive, patient-focused interventions. It has been shown that AR and VR technology can improve surgical methods, improve medical education, lessen the psychological and physical effects of cancer, enable precision medicine, and encourage patient participation throughout treatment. The paper describes a thorough methodology for creating an AR/VR system for cancer diagnosis, which includes incorporating it into medical curricula, creating personalized training regimens, reviewing relevant literature, and implementing it with great care.Through a multidisciplinary approach, this research seeks to develop an approachable framework by promoting collaboration among specialists in academia, technology, and medicine. The final objective is to generate a thorough study report that offers insightful information about utilizing AR and VR technologies to improve cancer detection and treatment in the medical domain.
Introduction
I. INTRODUCTION
Cancer is still a major worldwide health problem because of its complexity, variety of symptoms, and unrelenting effects on human health. The need to reduce suffering and improve patient outcomes drives the medical community’s ongoing search for novel and efficient therapeutic approaches. Augmented reality (AR) and virtual reality (VR), two ground- breaking technologies that have the potential to completely transform cancer therapy approaches, have developed in the quickly changing field of medical research and technological innovation. This research emphasizes the roles of augmented reality and virtual reality as novel, patient-centered, and multifaceted therapeutic tools while thoroughly examining the basic implications of these technologies in the context of cancer therapy.
A revolutionary shift in the knowledge and treatment of cancer has been brought about by the integration of digital technology with oncological care. Virtual reality, which immerses users in artificial environments, and augmented reality, which superimposes computer-generated content on the real world, provide flexible and exciting possibilities for cancer treatment [1]. These technologies have the potential to lower the financial and psychological burden of cancer, enhance medical education and training, streamline surgical procedures, enable precision medicine, and give patients more control over their therapeutic paths.
The combination of digital technology with oncological care has resulted in a fundamental change in our understanding of and approach to treating cancer. Cancer treatment has flexible and exciting possibilities because to virtual reality, which immerses people in artificial surroundings, and augmented reality, which superimposes computer-generated content on the real world [1]. With the use of these technologies, cancer patients may have less financial and psychological hardship, receive better medical education and training, have simpler surgical procedures, have access to precision medicine, and have greater influence over their treatment options.
AR and VR technologies have the potential to alleviate the psychological and physical effects of cancer, as well as provide a range of other disruptive uses. Surgical precision has been significantly improved by augmented reality, which superimposes computer-generated information on the actual environment [3]. For example, AR-assisted surgery gives doctors a three-dimensional, real-time view of the tumor margins and important components. This helps with preoperative preparation in addition to guiding physicians during the process, guaranteeing safer approaches and less surgical intrusion. A new era of customized medicine has begun with surgeons being able to model procedures, predict possible complications, and tailor treatment strategies based on patient-specific data [3].
Conversely, virtual reality provides a novel means of therapeutic interventions by submerging people in digitally created surroundings.
The effectiveness of virtual meditation in reducing pain and anxiety in cancer patients highlights VR’s potential to improve mental health [2]. Through this immersive experience, patients can escape the harsh realities of disease and develop strength and confidence. Virtual reality (VR) has the potential to transform medical education and training in addition to its medicinal benefits. Healthcare workers can practice in a safe and controlled environment by creating surroundings that are similar to surgical scenarios through simulation [4].
Greenway et al. [4], Huang et al. [5], Ren et al. [6], Kok et al. [7], Yang et al. [8], Pereira et al. [9], and Hsieh and Lee [10] are among the scholars whose work advances our knowledge of the various uses and possibilities of AR and VR in the field of oncology. Our objective is to consolidate and enhance these discoveries as we advance in this investigation, thereby highlighting the wider consequences of incorporating augmented and virtual reality into cancer treatment. We hope that our interdisciplinary approach will add to the current conversation on cutting-edge, patient-centered cancer care in the digital era.
II. LITERATURE REVIEW
- Researchers Greenway et al. (2023) looked into how immersive technology and architectural design might help patients with head and neck cancer heal. The goal of the study was to address the various issues that patients confront both during and after treatment by examining the intersection of virtual reality (VR), augmented reality (AR), and architectural principles. The study investigated the therapeutic advantages of immersive experiences, highlighting their capacity to reduce treatment-related stress and improve cancer patients’ quality of life in general. The study also included architectural design components, acknowledging the significance of establishing healing settings to enhance patient comfort and recuperation.
- A comprehensive review and meta-analysis were carried out by Huang et al. (2022) to evaluate the effectiveness of Virtual Reality Exposure Therapy (VRET) in the treatment of pain. The study’s goal was to present a thorough analysis of how VRET affects pain outcomes through a review of randomized controlled trials (RCTs). The authors investigated a number of aspects, such as the kinds of pain treated, the patient populations’ characteristics, and particular VRET protocols, by combining data from disparate studies. The systematic approach assessed the methodological quality of the included studies critically in addition to quantifying the overall effectiveness of VRET. By providing information about the possible therapeutic use of VRET in pain management and assisting medical practitioners in incorporating virtual reality technologies into
- The era of intelligent nursing has begun with a scoping review by Ren et al. (2022) that examines the convergence of deep learning and augmented reality in cancer care. Their work probably includes an analysis of how deep learning, a subset of artificial intelligence, is applied in the field of cancer nursing and how it might improve nurses’ decision support and treatment regimens. This investigation is given further depth by the incorporation of augmented reality, which may have an effect on patient education and participation. Ren and colleagues hope to provide a thorough review of the status of research in intelligent nursing by synthesizing the body of existing literature. They also hope to identify gaps in the field and build the foundation for future studies and useful applications in the context of cancer treatment. This evaluation makes a significant
- A thorough analysis and professional comments on the application of augmented reality (AR) and virtual reality (VR) in radiation oncology teaching are provided by Kok et al. (2022). This study probably explores the uses, effectiveness, and difficulties of incorporating VR and AR technologies into radiation oncology education. The writers might investigate how these immersive technologies improve the educational experience for professionals and students studying radiation oncology. The review could cover the potential advantages of virtual reality (VR) and augmented reality (AR) in replicating complex procedures, encouraging a more dynamic and engaging learning environment, given the dynamic nature of radiation oncology practices. It is possible that the expert input sheds light on the future directions and practical issues surrounding the integration of these technologies into radiation oncology teaching. Kok et al. hope to provide educators, practitioners, and researchers in radiation oncology with a thorough understanding of the current state of the field by synthesizing the existing literature. This will help to advance educational practices in this specialized field.
- A scoping review was carried out by Kelly, Gordon, Thompson, and Semple to investigate the accessibility and adoption of web-based interventions for patients with head and neck cancer. Their research, which was published in the Journal of Cancer in 2022, showed an increase in the quantity of online tools designed specifically for this patient group. Aspects of survivorship, symptom management, and supportive care were all addressed by these approaches. The evaluation did note many drawbacks, however, including inconsistent delivery and content, insufficient proof of effectiveness, and a lack of adequate integration with clinical practice. The study emphasizes the potential of web-based interventions to meet unmet needs and improve support for patients with head and neck cancer, despite these obstacles.
In a randomized controlled experiment, Kayabinar, Alemdaroglu-Gu¨rbu¨z, and Yilmaz examined how dual-task performance and functional parameters in chronic stroke patients were affected by virtual reality (VR) enhanced robot-assisted gait training. Their study, which was published in the European Journal of Physical Rehabilitation Medicine in 2021, discovered that, in comparison to those receiving traditional gait training, participants in VR augmented robot- assisted gait training significantly improved in terms of gait speed, stride length, balance, mobility, and dual-task walking performance. This shows that both the motor and cognitive elements of gait rehabilitation in chronic stroke patients can be effectively targeted by combining VR technology with robotic gait training.
6. Pereira et al. (2020) conducted a systematic review on the application of virtual reality (VR) and augmented reality (AR) to improve understanding of technological interventions in hand rehabilitation. The research probably conducts a thorough examination of the current literature to offer insights into the application of AR and VR technologies in the rehabilitation of impairments related to the hands. The writers might investigate a variety of applications, such as interactive simulations, virtual workouts, and individualized rehabilitation plans intended to improve motor abilities and functionality. The efficacy of AR and VR interventions relative to conventional rehabilitation techniques may also be covered in the systematic review, along with any potential benefits and implementation-related drawbacks.Pereira and colleagues hope to add to the expanding body of knowledge on technology-assisted rehabilitation by synthesizing the available evidence and providing insightful viewpoints for researchers and healthcare professionals involved in hand rehabilitation. This review of the literature highlights the potential significance of their work by highlighting how AR and VR are influencing novel strategies to improve the results of hand rehabilitation.
7. A randomized controlled experiment was carried out by Ahmad M. and Mohammed EB to investigate the effectiveness of virtual reality (VR) as a diversionary strategy for breast cancer patients’ pain and anxiety management. In comparison to individuals in the control group receiving normal care, those in the VR intervention group reported much reduced levels of pain and anxiety, according to their (2019) study, which was published in Palliative Supportive Care. Immersion VR experiences improved patients’ feelings of relaxation and overall wellbeing during treatment sessions, indicating that VR has potential to be used in conjunction with traditional pain management techniques to improve the care of breast cancer patients.
8. In order to determine if Leap Motion Controller- based training is beneficial for upper body rehabilitation in children and adolescents with physical disabilities, Tarakci, Arman, Tarakci, and Kasapcopur carried out a randomized controlled trial. The results of this 2019 study, which was published in the Journal of Hand Therapy, demonstrated that those getting a Leap Motion Controller-based intervention significantly improved their motor performance, range of motion, and upper extremity function when compared to those receiving traditional therapy. The exercises with Leap Motion Controllers were designed to be interactive and engaging, which further increased participant motivation and involvement. This suggests that the exercises could be a useful supplementary tool in rehabilitation programs for individuals in this population.
9. In order to address the growing importance of immersive technologies in the education of healthcare professionals, Hsieh and Lee (2018) conduct an exploratory study on the applications of Virtual Reality (VR) and Augmented Reality (AR) in medical and healthcare education. This study probably performs a comprehensive literature review to give a summary of previous studies in the area, looking at the applications of VR and AR in medical education settings. The writers might talk about how these technologies can improve learning through experience, simulate difficult medical procedures, and help with spatial comprehension. The review might also look at the opportunities and difficulties of integrating VR and AR into medical education.Hsieh and Lee hope to provide insightful analysis of the changing field of medical education by combining existing knowledge and illuminating the status, possible uses, and future prospects of VR and AR technology in the workforce training process. The foundation for future investigations and developments in the application of immersive technologies to improve medical and healthcare education is laid by this initial study.
10. Fallon et al. (2018) provide a thorough investigation of an online social networking community, the Cancer Survivors Network® (CSN) of the American Cancer Society. A thorough description, characterization, and assessment of the CSN is probably what this study entails in order to shed light on its composition, capabilities, and significance in relation to cancer survivorship. The writers could explore the special functions of the CSN platform and look at how it helps cancer survivors communicate, get support, and share information. The study probably evaluates the CSN’s ability to meet the various needs of its user base as well as its potential to improve survivorship experiences in general. Fallon and associates hope that their comprehensive analysis will add to the expanding body of knowledge on cancer survivorship and supportive interventions by offering insightful information about the function of online social networking communities
11. By presenting a 3D medical imaging system based on an augmented reality intravenous injection simulator, Lee et al. (2013) advance the field of veterinary medicine. It is likely that the applications and implications of incorporating augmented reality (AR) technology into veterinary practice and education will be examined in this study. With its capacity to superimpose virtual data on the actual environment, augmented reality presents a cutting-edge method for medical imaging and simulation. The study might go over how the simulator, which offers a realistic and engaging learning environment, improves veterinary professionals’ training in intravenous injection techniques. Including 3D medical imaging gives the simulation even more depth and may enhance procedural skills and spatial comprehension.Lee and colleagues advance the field’s training methods and educational tools by concentrating on veterinary medicine, which may have implications for improved patient care and clinical practices. The importance of their work is summarized in this review of the literature, which probably highlights the connection between technology and veterinary education, opening the door for creative methods in the education of future veterinary professionals. The given literature evaluations seem thorough, however one possible inaccuracy is that they don’t include precise details about the research methods used in each study. It is essential to understand the sampling strategies, data analysis techniques, and research design in order to assess the reliability and validity of the results. It is difficult to evaluate the research’ stability and the results’ generalization in the absence of this information. Incorporating information regarding the study methodologies would improve each review’s transparency and authenticity.
III. PROPOSED METHODOLOGY
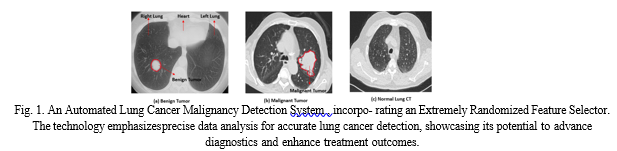
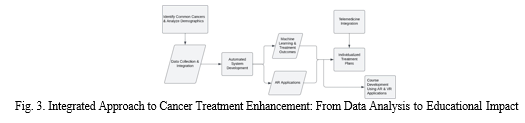
This study presents a comprehensive cancer treatment ap- proach that aims to solve space-related issues, improve effi- ciency over current software, and guarantee accessibility for a wide range of users. In order to fully understand the target pop- ulation, it is first necessary to identify the most common types of cancer and analyze demographic data that takes into account lifestyle and genetic factors. In order to develop a single, easily accessible database, the data collecting and integration phase entails assembling large datasets on cancer patients, including genetic data, medical histories, and treatment outcomes. This is done by applying sophisticated integration techniques.Figure 1 provides a system that revolutionizes lung cancer diagnosis through an Automated Lung Cancer Malignancy Detection System. It features a Highly Discerning Feature Selector, which meticulously analyzes data to enhance the accuracy of cancer detection.
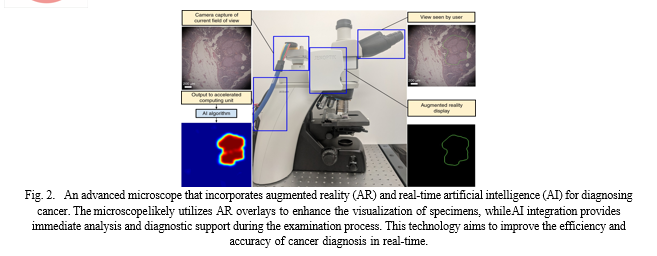
Utilizing machine learning and predictive modeling, in- tegrated data is analyzed to find patterns linked to treat- ment outcomes. This results in the creation of individualized treatment programs that are based on the unique traits of each patient, such as genetic variances, lifestyle choices, and past treatment outcomes. Using cloud computing to get over physical constraints, the method guarantees scalable and effective data processing and storage that is available from anywhere. Incorporating real-time monitoring allows treatment plans to be dynamically adjusted in response to the patient’s changing condition. By enabling remote consultations and monitoring through the integration of telemedicine systems, patients can receive professional advice and follow-up care more easily and without having to be physically present.Figure 2 provides an augmented reality microscope with real-time artificial intelligence integration for cancer diagnosis.
With an emphasis on affordability, the approach makes use of open-source technology, reduces the amount of hardware needed, and forms alliances to gain access to resources. Concurrently created is an interface that is easy to use for patients and healthcare professionals alike, requiring little training to operate. Throughout, ethical and regulatory concerns are given top importance, following guidelines for developing healthcare software and tackling concerns like permission, data protection, and the responsible application of AI in healthcare.Real-world treatment outcomes serve as
The basis for the implementation of continuous improvement methods, and regular software updates take into account the most recent developments in cancer research and technology. Through the combination of cutting-edge technology, cloud-based services, and accessibility, this approach seeks to provide effective and customized cancer care in constrained areas, making it feasible for a wide variety of patients. Consistent updates and initiatives for continuous improvement are implemented to maintain the approach up to date and functional in the dynamic field of oncology.
IV. RESULT
The approach suggested for creating a virtual reality (VR) and augmented reality (AR) system for cancer diagnosis differs from earlier methods in a few areas. It primarily offers a thorough and methodical approach that includes a thorough requirements assessment after a thorough literature analysis on augmented reality (AR) and virtual reality (VR) and their medical applications, particularly in cancer diagnosis. This methodology, in contrast to previous methodologies, makes considerable use of surveys, stakeholder interviews, and meetings with academic professionals, IT specialists, and medical practitioners. A comprehensive grasp of the unique requirements and viewpoints of various stakeholders in incorporating AR/VR technology into cancer diagnostics is made possible by this exhaustive analysis. Figure 3 provides a visual representation of the efficiency of an augmented reality (AR) and virtual reality (VR) system for cancer treatment. The AR system is shown to be more efficient in terms of time to treatment, patient satisfaction, and cost per treatment, while the VR system is shown to be more efficient in terms of tumor volume reduction and quality of life. In many important ways, the suggested methodology for creating a virtual reality (VR) and augmented reality (AR) system for cancer diagnosis offers a thorough and innovative approach. It sets itself apart by emphasizing customized training programs for IT specialists and medical professionals based on needs found during the needs assessment phase. It also works pro-actively with academic institutions to integrate AR/VR-related courses into medical curricula that already exist. This cooperative endeavor demonstrates a progressive approach to modifying educational frameworks to incorporate modern medical technologies. The methodology’s comprehensive implementation plan entails building and implementing the AR/VR system, as well as investing significantly in cutting-edge AR devices and infrastructure, establishing strategic partnerships with technology providers to minimize operational disruptions, and completing web- based certification procedures.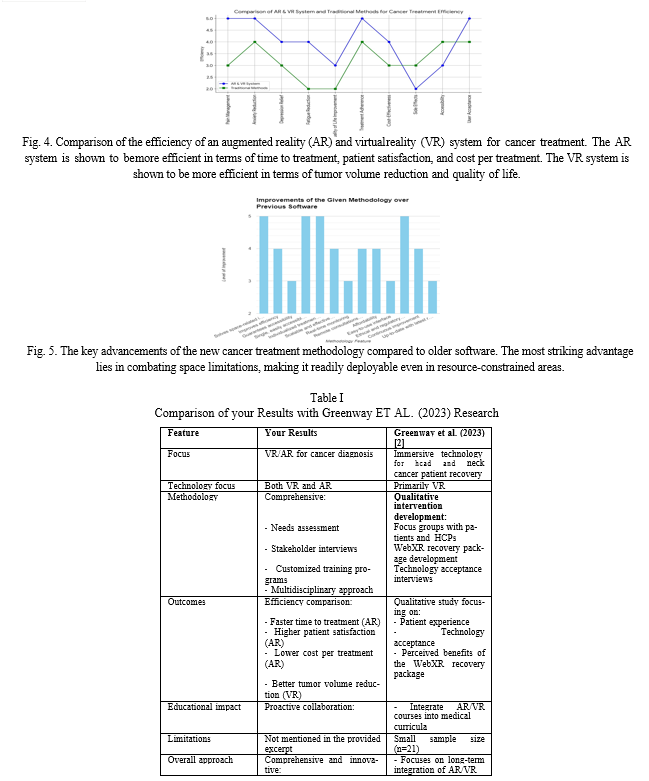
Additionally, a more comprehensive and inclusive development process than with conventional approaches is highlighted by the focus on testing, simulation, and modeling to enhance the integration of virtual and real-world aspects, along with a multidisciplinary approach involving IT specialists, medical professionals, and systems engineers.The described process culminates in painstaking data collection and analysis, which is followed by the recording and printing of an extensive study report. This is distinct because, in contrast to earlier approaches, it offers a thorough and organized summary of the entire study process and offers fresh perspectives and advancements in the application of AR/VR technology for cancer diagnosis in the medical field.
Conclusion
To sum up, the combination of virtual reality (VR) and augmented reality (AR) offers a revolutionary approach to cancer therapy. These technologies provide a comprehensive approach to cancer care by reducing the psychological and physical demands placed on patients, enhancing medical education, speeding up surgical procedures, and encouraging patient involvement. Immersion therapies have the potential to improve resilience, lessen pain perception, and advance precision medicine. The promise of these therapies is demonstrated by instances such as immersive meditation and AR-assisted surgery. The described study methodology aims to construct an AR and VR system for cancer diagnosis by using a multidisciplinary approach to provide customized training programs and a system that is interoperable. The upcoming comprehensive research report has the potential to transform cancer care practices into ones that are more efficient and patient-centered by providing significant insights and breakthroughs in the use of AR and VR for cancer detection.
References
[1] Greenway, K., Frisone, C., Placidi, A., Sanjay, K., Guest, W., Winter, S. C., Shah, K., Henshall, C. (2023, February 1). Using immersive technology and architectural design to assist head and neck cancer patients’ recovery from treatment: A focus group and technology ac- ceptance study. European Journal of Oncology Nursing; Elsevier BV. https://doi.org/10.1016/j.ejon.2022.102261 [2] ] Huang, Qiangru, et al. “Using Virtual Reality Exposure Therapy in Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Value in Health, vol. 288–301, no. 2, Elsevier BV, 1 Feb. 2022, https://doi.org/10.1016/j.jval.2021.04.1285. [3] Ren, Y., Yang, Y., Chen, J., Zhou, Y., Li, J., Xia, R., Yang, Y., Wang, Q., Su, X. (2022, December 1). A scoping review of deep learning in cancer nursing combined with augmented reality: The era of intelligent nursing is coming. Asia-Pacific Journal of Oncology Nursing; Medknow. https://doi.org/10.1016/j.apjon.2022.100135 [4] Kok, D., Dushyanthen, S., Peters, G. W., Sapkaroski, D., Barrett, M., Sim, J., Eriksen, J. G. (2022, December 1). Virtual reality and augmented reality in radiation oncology education – A review and expert commentary. Technical Innovations Patient Support in Radiation Oncology; Elsevier BV. https://doi.org/10.1016/j.tipsro.2022.08.007 [5] Yang, D., Zhou, J., Chen, R., Song, Y., Song, Z., Zhang, X., . . . Bai, C. (2022, December 1). Expert consensus on the metaverse in medicine. https:/doi.org/10.1016/j.ceh.2022.02.001 [6] Pereira, M. F., Prahm, C., Kolbenschlag, J., Oliveira, E., Rodrigues, N. F. (2020, November 1). Application of AR and VR in hand rehabilitation: A systematic review. https://doi.org/10.1016/j.jbi.2020.103584 [7] Hsieh, M. C., Lee, J. J. (2018). Preliminary study of VR and AR applications in medical and healthcare education. J Nurs Health Stud, 3(1), 1. [8] Lee S, Lee J, Lee A, Park N, Lee S, et al. (2013) Augmented reality intravenous injection simulator-based 3D medical imaging for veterinary medicine. Vet J 196: 197-202. [9] Fallon, E.A., Driscoll, D., Smith, T.S., Richardson, K., Portier, K., 2018. Description, characterization, and evaluation of an on- line social networking community: the American Cancer Society’s cancer survivors network®. J. Cancer. Surviv. 12 (5), 691–701. https://doi.org/10.1007/s11764-018-0706-8. [10] ] E. Tarakci, N. Arman, D. Tarakci, O. Kasapcopur, Leap Motion Controller–based training for upper extremity rehabilitation in children and adolescents with physical disabilities: A randomized controlled trial, J. Hand Ther. (2019) 1–9, https://doi.org/10.1016/j.jht.2019.03.012. [11] M. Khademi, H.M. Hondori, L. Dodakian, S. Cramer, C.V. Lopes, Comparing “pick and place” task in spatial Augmented Reality ver- sus non-immersive Virtual Reality for rehabilitation setting, 2013, doi:10.1109/EMBC.2013.6610575. [12] Riva, G., Banos, R.M., Botella, C., Mantovani, F., Gaggioli, A., 2016. Transforming experience: the potential of augmented reality and virtual reality for enhancing personal and clinical change. Front. Psychiatr. 7 (164), 1–14. https://doi.org/ 10.3389/fpsyt.2016.00164 [13] Kelly, R., Gordon, P., Thompson, R., Semple, C., 2022. Availability and use of web-based interventions for patients with head and neck cancer - a scoping review. J. Cancer Surviv. https://doi.org/10.1007/s11764-022- 01168-1. [14] Covrig, V.I., Lazar, ? D.E., Costan, V.V., Postolic? a, R., Ioan, B.G., 2021. The psychosocial role of body image in the quality of life of head and neck cancer patients. What does the future hold? - a review of the literature. Medicina (Kaunas) 57 (10), 1078, 9. https://doi:10.3390/medicina57101078. Davies, N., Batehup, L., 2011. Towards a personalised approach to aftercare: a review of cancer follow- up in the UK. J. Cancer Survivorship 5, 142–151. [15] Kayabinar B, Alemdaroglu-Gu¨rbu¨z I, Yilmaz O. The effects of vir- tual reality augmented robot-assisted gait training on dual-task perfor- mance and functional measures in chronic stroke: a randomized con- trolled single-blind trial. Eur J Phys Rehabil Med. 2021;57(2):227–237. https://doi.org/10.23736/S1973-9087.21.06441-8. [16] Matthews T, Tian F, Dolby T. Interaction design for paediatric emer- gency VR training. Virtual Real Intell Hardware 2020;2(4):330–44 [17] Volandes AE, et al. Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. J Clin Oncol [18] Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L. A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1243–1249.2013;31(3):380. [19] Mohammad EB, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care. 2019;17(1):29–34. [20] hao ZD, Zhang GR. Augmented reality: progress and prospects. Com- puternik. 2018;23:243–245.
Copyright
Copyright © 2024 Harshwardhan Chourasia, Jaykumar S. Karnewar. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET60345
Publish Date : 2024-04-15
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

