Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Awareness of Night Eating Syndrome Among College Students (18-29 Years) Native to Manipur
Authors: S. Ferhinn Chisti, Navaneetha R
DOI Link: https://doi.org/10.22214/ijraset.2024.58762
Certificate: View Certificate
Abstract
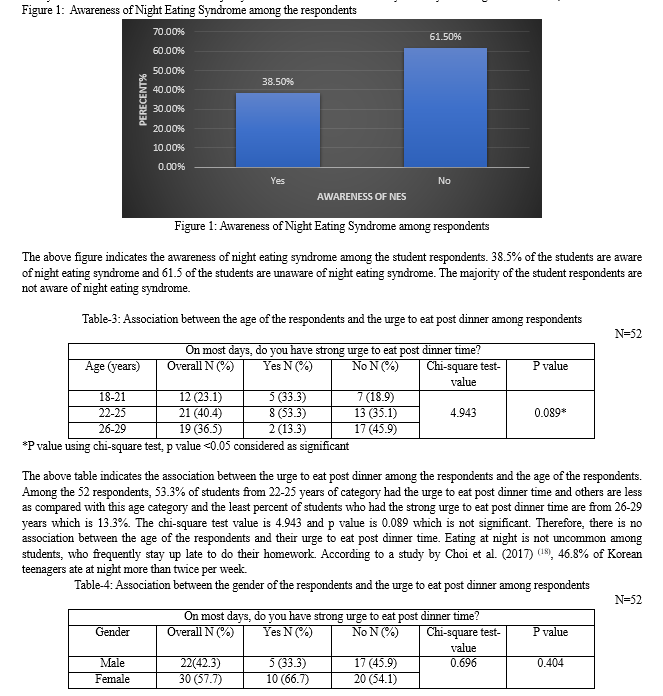
Night Eating Syndrome (NES) is a stress-related disorder characterized by morning aphagia, evening hyperphagia and insomnia with the presence of nocturnal ingestions and mood variations which worsen in the evening and night. Presence of eating disorders, psychological disorders, sleep issues like trouble getting to sleep or staying asleep also contribute to this disorder . Night eating syndrome may lead to obesity, metabolic syndrome, diabetes and other life style disorders. The aim of this study is to create awareness of NES and its consequences among college students aged 18-29 years who are native to Manipur. The study collected demographic details and anthropometry measurements of the students and also studied their awareness of NES. Their knowledge about the association of regularly eating post dinner and adverse health outcomes was also studied. The following parameters were considered like age, gender, educational status, BMI category, physical level to study and to create awareness of NES among them. The study used descriptive and exploratory survey design with a quantitative approach to collect data from college students (18-29 years) who are native to Manipur. The sample size was 78 (as per inclusion criteria) consisting of both males and females together. This study revealed that the college students with a percentage of 61.5% from among the total respondents of 52, were not aware of NES and it’s consequences. The limitations of the study suggest further research in the area of Night Eating Syndrome to increase the awareness amongst the population and prevent the occurrence of lifestyle diseases.
Introduction
I. INTRODUCTION
Stunkard et al. (1955) described Night Eating Syndrome (NES) as a stress-related eating disorder characterised by morning anorexia, evening hyperphagia, and insomnia for the first time [1]. The symptoms of NES include a disruption in the circadian rhythm, disconnection between eating and sleeping, as well as a delay in the onset of morning appetite and the continuation of eating in the evening [2]. The increased awareness of NES over the last decade has resulted in several changes to its core diagnostic criteria, which has aided in a better understanding of factors which can lead to Night Eating Syndrome [3]. The absence of a consensus definition of NES has hampered its detection and made it challenging to compare studies on the said illness (4).
To address this issue, diagnostic criteria for NES were proposed in 2010(3). The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders included NES as well (5). The following are the diagnostic requirements for NES: 1) recurrent episodes of night eating, as shown by eating right after waking up from sleep or by consuming too much food right after dinner, 2) awareness of those eating episodes, and 3) significant distress or impairment brought on by the disorder. Binge eating disorder or any other mental illness are considered as exclusion factors (5).
NES shares several characteristics with other mental conditions, particularly with eating and sleeping disorders such as sleep-related eating disorders (SRED). But there are some significant distinctions between NES and these conditions. According to a study by Allion KC and Tarves EP (2011), the most crucial factor is accurate diagnosis of NES which will greatly help in offering them with the best care (6).
NES can be assessed using self-report questionnaires and semi-structured diagnostic tools such as the Night Eating Questionnaire (NEQ), Night Eating Syndrome Questionnaire (NESQ), Night Eating Diagnostic Questionnaire (NEDQ), Night Eating Symptom Scale (NESS), Eating Disorder Examination (EDE), and Night Eating Syndrome History and Inventory (NESHI) (7).
Studies have produced conflicting results about the link between NES and obesity ever since NES was originally defined. Studies conducted over an extended period of time revealed that night eaters experienced significant weight gain, supporting the idea that NES may one day contribute to the development of obesity (8,9).
Few researchers have looked at the connection between NES and diabetes mellitus (DM). According to the study samples used for diagnosing NES, it was estimated that between 3.8 and 12.4% of DM patients had NES (10,11,12). There are studies showing that night eating is linked to poorer diet management, inadequate glucose monitoring, diabetes and obesity (13).
The syndrome is one of the leading causes of some of the non-communicable diseases among young adults (18-29 years) as well in later years. In India, there are more than 135 million obese people (14). Type2 Diabetes Mellius affects more than 69 million people in India now, and by 2040, that number is expected to rise to 140 million, with more than half of them remaining untreated (15). According to researchers, India has an overall prevalence of dyslipidemia that ranges from 10% to 73% (16). Further ICMR-INDIAB study found that 26.3% of the population were not aware that they had hypertension (17). Therefore it is necessary to create awareness about Night Eating Syndrome especially among the young adults (18-29 years) and its consequences so that they can make the necessary lifestyle changes to prevent the onset of non-communicable diseases. The young adults between 18-29 years were chosen for this study because of lack of adequate studies regarding NES in India in this age group.
The current study aimed to create awareness of night eating syndrome and its consequences among college students (18-29 years) native to Manipur. The main objectives of the study were:
- To study the awareness of night eating syndrome among college students (18-29 years) native to Manipur.
- To study the association between urge to eat post dinner time and NES with base line parameters (Age, Gender, BMI and Type of activity) among the college students (18-29 years) native to Manipur.
- To study association between the consumption of food to satisfy the urge to eat post dinner time and NES with base line parameters (Age, Gender, BMI and Type of activity) among the college students (18-29 years) native to Manipur.
II. MATERIALS AND METHODS
- Study Design: Descriptive and exploratory survey design with a quantitative approach.
- Location: Cities and towns across Manipur where college students (18-29 years) native to Manipur are residing.
- Sample: College students native to Manipur (residents of Manipur) of around the age 18 to 29 years living across cities and towns in Manipur.
- Inclusion criteria: Healthy college students, who consented to take part in the study, both male and female between the age of 18 to 29 years native to Manipur and who are aware of the Manipuri local foods.
- Exclusion criteria: Subjects with chronic illness or who are on long term medication, who are non-native to Manipur.
- Sampling technique: Non-probability purposive sampling using structured questionnaire.
- Setting and data collection: A google form was shared with 78 college students who suited the inclusion criteria of this study.They were given a brief explanation of the purpose of the study and the eligibility criteria for participation. Informed consent form was shared and consents were obtained from the participants.
- Tools used for data collection: Structured questionnaire, administered through google form.
- Components studied through the survey:
a. Personal and socio-economic information of the respondents
Demographic parameters like name, age and gender of the respondents, their contact number and email address, educational status, their family size and type and monthly income were gathered.
b. Anthropometric information of the respondents
Nutritional anthropometric values of height, weight waist and hip circumferences were gathered to calculate the BMI of the respondents. A detailed instruction on how to measure the waist and hip circumferences was given in the questionnaire itself.
c. Health, diet and lifestyle followed information of the respondents
Here information on the respondents’ consumption of health supplement(s), physical activity level, their dietary habit, number of meals consumed and their amount of water intake per day were gathered.
d. Night Eating Syndrome and lifestyle related information of the respondents.
Here information on respondents’ awareness on Night Eating Syndrome, what is Night Eating Syndrome, their dinner time, bed time and wake-up time, their sleep duration, their urge to eat and consumption of food, frequency of consumption and kinds of food consumed post dinner, their trouble in getting to sleep and its causes, their awareness as night eater, the mood they are generally in, their appetite after getting up in the morning, the activities they enjoy and time spent on these activities were gathered.
e. Educational aid shared to create awareness of NES among respondents:
A short video of 26 seconds was created on awareness of NES and was shared to the respondents .
Statistical methods: Kolmogorov-Smirnov test was used to test the normality. Continuous variables were presented with mean and Standard deviation or median and Inter quartile range (IQR) as appropriate. Categorical variables were reported with frequency and percentage The results were considered statistically significant at the level of alpha <0.05 in all analysis. Statistical analysis was performed using IBM SPSS Statistics 27.0.
III. RESULTS AND DISSCUSSION
Table-1: Anthropometric measurements of the respondents
N=52
|
Anthropometric measurements |
Mean |
Standard Deviation |
|
Height (cm) |
163.13 |
8.564 |
|
Weight (kg) |
61.029 |
9.541 |
|
BMI (kg/m2) |
22.61 |
4.136 |
|
Waist circumference (cm) |
81.58 |
9.215 |
|
Hip circumference (cm) |
90.85 |
10.740 |
The above table indicates the descriptive statistic parameters of 52 respondents. Among the respondents, the mean height was 163.13 cm and SD±8.56; the mean weight was 61.02kg and SD± 9.54; the mean BMI was 22.61 kg/m2 and SD±4.13; the mean waist circumference was 81.58cm and SD±9.21 and the mean hip circumference was 90.85cm and SD± 10.74.
Table-2: Demographic characteristics of the respondents (Age, Gender, Educational qualifications, Family size and Family monthly income)
N=52
|
Demographic characteristics |
Frequency (N) |
Percent (%) |
|
|
Age (years) |
18-21 |
12 |
23.1 |
|
22-25 |
21 |
40.4 |
|
|
26-29 |
19 |
36.5 |
|
|
Gender |
Male |
22 |
42.3 |
|
Female |
30 |
57.7 |
|
|
Educational status |
Under graduate |
22 |
42.3 |
|
Post graduate |
24 |
46.2 |
|
|
Ph.D. |
0 |
0 |
|
|
Others |
6 |
11.5 |
|
|
Family size |
Up to 5 |
30 |
57.7 |
|
>5 |
22 |
42.3 |
|
|
Family monthly income (?) |
≥78,063 |
17 |
32.7 |
|
39,033-78,062 |
11 |
21.2 |
|
|
29,200-39,032 |
11 |
21.2 |
|
|
<29,000 |
13 |
25.0 |
|
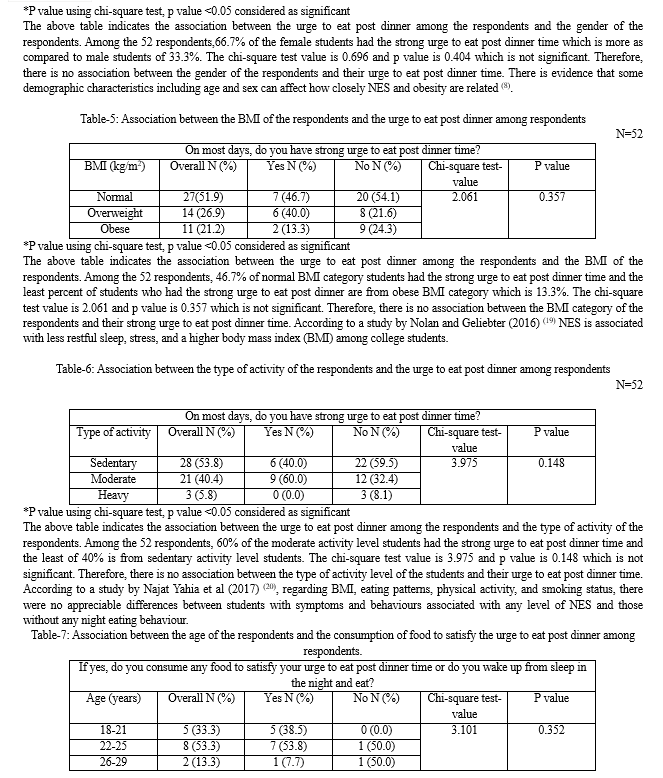
Table 2, indicates the demographic details (age, gender, educational qualifications, family size and family monthly income) of the student respondents. 23.1% of the students are among the age group of 18-21 years and 40.4% are among the 22-25 years of age group and 36.5% are among the age group of 26-29 years. The majority of the student respondents are from the age group of 22-25 years. 42.3% of the students are male and the remaining 57.7% students are female. The majority of the student respondents are female.42.3% of the students are pursuing their under graduate, 46.2% of the students are doing their post graduate and 11.5% of the students are engaged in other academic pursuits are than under graduate or post graduate or Ph.D.
The majority of the student respondents are pursuing their post graduate. 57.7% of the students have a family size of up to 5 and 42.3% of the students have a family size more than 5. The majority of the student respondents have their family size of up to 5. 32.7% of the students have their family monthly income greater than ?78,063, 21.2% of the students have their family income between ?39,033-78,062, 21.2% of students have their family income between ?29,200-39,032 and 255 of the students have their family income lesser than ?29000. The majority of the students have their family monthly income greater than ?78,063.
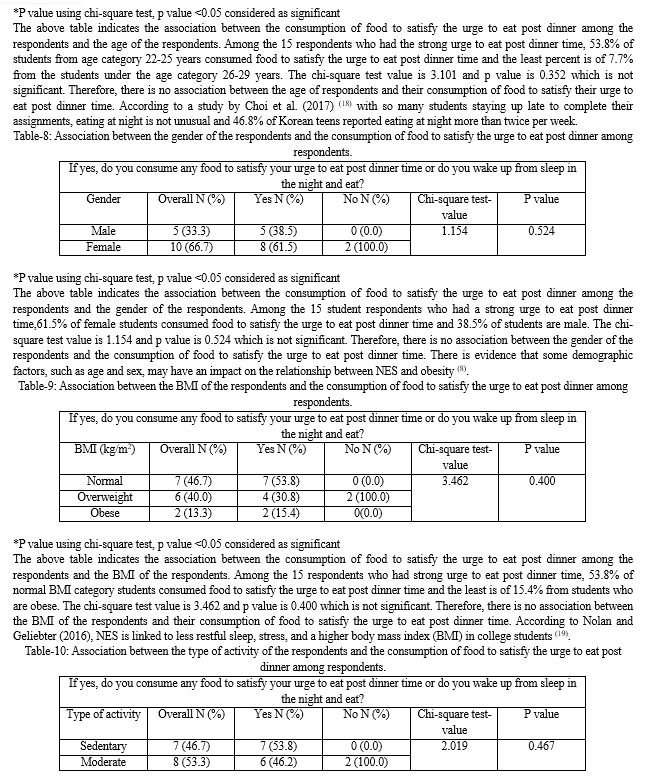
*P value using chi-square test, p value <0.05 considered as significant
The above table indicates the association between the consumption of food to satisfy the urge to eat post dinner among the respondents and the type of activity of the respondents. Among the 15 students who had strong urge to eat post dinner time, 53.8% of sedentary activity level students and 46.2% of students of moderate activity level consumed food to satisfy the urge to eat post dinner time. The chi-square test value is 2.019 and p value is 0.467 which is not significant. Therefore, there is no association between the activity level of the respondents and their consumption of food to satisfy the urge to eat post dinner time. According to a study by Najat Yahia et al (2017) (20), in terms of BMI, eating patterns, physical activity, and smoking status, there were no appreciable differences between students who demonstrated symptoms and behaviours consistent with any degree of NES and those who did not.
Conclusion
The study found that most of the student respondents are among the age group of 22-25 years (40.4%) who were pursuing their post-graduation (46.2%) and the female students were in majority (57.7%). Most of the participants were sedentary students (53.8%) and were non-vegetarian (78.8%). The study can be concluded with the points that: (?) The majority of the participants (61.5%) were not aware of Night Eating Syndrome and what it encompasses. (?) There does not exist a significance level in the association of the baseline demographic parameters and lifestyle followed with that of Night Eating Syndrome among the respondents. There is a need to have follow up on the intervention awareness educational programme on Night eating Syndrome among the college students (18-29 years), native to Manipur, so that they become aware of the syndrome and what it encompasses as well as the adverse outcomes due to the syndrome. Limitation of the Study: In this survey, Only 52 subjects completed the questionnaire out of the 78 subjects ( as per inclusion criteria) to whom the Google forms were shared during the data collection of this research study.
References
[1] Stunkard A, Grace WJ, Wolff HG. The night eating syndrome: a pattern of food intake among certain obese patients. Am J Med 1955; 19: 78-86. [2] Cleator J, Abbott J,Judd P, Sutton C, Wilding JPH. Night eating syndrome: implications for severe obesity. Nutrition and Diabetes 2012; 2. [3] Allison KC, Lundgren JD, O\'Reardon JP, Geliebter A, Gluck ME, Vinai P, Mitchell JE, Schenck CH, Howell MJ, Crow SJ, Engel S, Latzer Y, Tzischinsky O, Mahowald MW, Stunkard AJ. Proposed diagnostic criteria for night eating syndrome. Int J Eat Disord. 2010 Apr;43(3):241-7. doi: 10.1002/eat.20693. PMID: 19378289; PMCID: PMC4531092. [4] Vander Wal JS. Night eating syndrome: a critical review of the literature. Clin Psychol Rev. 2012;32(1):49–59. [5] American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th ed. Washington, DC: American Psychiatric Association; 2013. [6] Allison KC, Tarves EP. Treatment of night eating syndrome. Psychiatric Clin North Am. 2011;34(4):785–796. [7] Lundgren J. The night eating syndrome: an overview In: Preedy VR, Watson RR, Martin C, editors. Handbook of Behavior, Food and Nutrition. New York, NY: Springer; 2011. [8] Andersen GS, Stunkard AJ, Sorensen TI, Petersen L, Heitmann BL. Night eating and weight change in middle-aged men and women. Int J Obes Relat Metab Disord. 2004;28(10):1338–1343. [9] Gluck ME, Venti CA, Salbe AD, Krakoff J. Nighttime eating: commonly observed and related to weight gain in an inpatient food intake study. Am J Clin Nutr. 2008;88(4):900–905. [10] Allison KC, Crow SJ, Reeves RR, et al. Binge eating disorder and night eating syndrome in adults with type 2 diabetes. Obesity (Silver Spring). 2007;15(5):1287–1293. [11] Hood MM, Reutrakul S, Crowley SJ. Night eating in patients with type 2 diabetes. Associations with glycemic control, eating patterns, sleep, and mood. Appetite. 2014;79:91–96. [12] Schwandt B, de Zwaan M, Jager B. Co-morbidity between type 2 diabetes mellitus and night eating. Psychother Psychosom Med Psychol. 2012;62(12):463–468. [13] Morse SA, Ciechanowski PS, Katon WJ, Hirsch IB. Isn’t this just bedtime snacking? The potential adverse effects of night-eating symptoms on treatment adherence and outcomes in patients with diabetes. Diabetes Care. 2006;29(8):1800–1804. [14] Misra A, Khurana L. Obesity-related non-communicable diseases: South Asians vs. White Caucasians. Int J Obes (Lond). 2011; 35: 167–87 [15] The Growing Danger of Non-Communicable Diseases Acting Now to Reverse Course. The World Bank Human Development Network. Washington 2011. http: //siteresources.worldbank.org/healthnutritionandpopulation/Resources/Peer-Reviewed Publications/WBDeepeningCrisis.pdf (accessed 30 April, 2016). [16] Misra A, Luthra K, Vikram NK. Dyslipidemia in Asian Indians: Determinants and significance. J. Assoc. Physicians India 2004; 52: 137–42. [17] Bhansali A, Dhandhania VK, Mohan D, et al. Prevalence of and risk factors for hypertension in urban and rural India: the ICMR INDIAB study. J Hum Hypertens 2014; 29: 204–9. [18] Choi, M. K., Cho, Y. J., Kim, M. H., & Bae, Y. J. (2017). Night eating status according to body mass index of Korean adolescents. Nutrition & Food Science, 47(1), 89-100. https://doi.org/10.1108/NFS-04-2016-0043 [19] Nolan, L. J., & Geliebter, A. (201). “Food addiction” is associated with night eating severity. Appetite, 98, 89-94. https://doi.org/10.1016/j.appet.2015.12.025 [20] Yahia Najat, Brown C, Potter S, Szymanski H, Smith K, Pringle L, Herman C, Uribe M, Fu Z, Chung M, Geliebter A. Night eating syndrome and its association with weight status, physical activity, eating habits, smoking status, and sleep patterns among college students. Eat Weight Disord. 2017 Sep;22(3):421-433. doi: 10.1007/s40519-017-0403-z. Epub 2017 Jun 2. PMID: 28573425.
Copyright
Copyright © 2024 S. Ferhinn Chisti, Navaneetha R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET58762
Publish Date : 2024-03-03
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

