Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Centralized Health Coordination System for Managing Medical Records
Authors: Ekta Yadav, Er. Sarika Singh
DOI Link: https://doi.org/10.22214/ijraset.2024.62687
Certificate: View Certificate
Abstract
Problem Statement: Current healthcare systems often rely on paper-based reporting, leading to delayed access to critical test results for both patients and doctors. Additionally, fragmented health records pose challenges for healthcare professionals in making informed decisions due to scattered data. Moreover, demographic disparities limit access to essential health information. Inefficient workflows among pathologists further exacerbate the delay in delivering crucial data to doctors and patients. These issues collectively hinder efficient healthcare delivery, increase operational costs, and compromise patient outcomes. Criteria Used: Transitions from paper to digital reporting, ensuring immediate access to test results for patients and doctors. It consolidates scattered health records into a comprehensive digital system, empowering healthcare professionals. Using phone numbers as identifiers, it bridges demographic gaps, allowing universal access to health data. Real-time monitoring enables patient empowerment. It streamlines pathologists\' workflow by inputting data directly into the digital system, easily accessible by doctors and patients. This transformation enhances healthcare delivery, cuts costs, and fosters better outcomes for all.
Introduction
I. INTRODUCTION
In the dynamic landscape of modern healthcare, the transition from paper-based record-keeping to digitalized systems marks a monumental leap forward in the quest for more efficient, accessible, and patient-centric care. At the forefront of this transformation lies the Centralized Health Coordination System—an innovative technological marvel poised to revolutionize the way medical records are managed, accessed, and analysed.
Imagine a comprehensive platform that serves as the central nervous system of healthcare coordination, seamlessly integrating the diverse array of stakeholders—doctors, patients, and pathology services—into a unified digital ecosystem. This cutting-edge system transcends traditional boundaries, offering a holistic approach to medical record management that is as intuitive as it is transformative.
At its heart, the Centralized Health Coordination System empowers healthcare providers with powerful tools for recording, analysing, and interpreting medical data. Through intuitive graphical interfaces and sophisticated analytics capabilities, doctors can gain deeper insights into patient health trends, enabling more informed decision-making and personalized treatment plans. Patients, in turn, benefit from unprecedented access to their own medical records, empowering them to take an active role in their healthcare journey.
One of the most profound advantages of this digitalized approach is its ability to overcome the limitations of traditional paper-based systems. No longer bound by physical constraints or the risk of lost or misplaced documents, patients can now access their medical records securely from any location with an internet connection. This newfound accessibility not only enhances patient convenience but also facilitates seamless collaboration between healthcare providers, leading to more coordinated and comprehensive care delivery.
For pathology services, the transition to digitalization represents a paradigm shift in workflow management and efficiency. By digitizing and centralizing medical records, pathologists can streamline record-keeping processes, reduce administrative burdens, and improve the accuracy and timeliness of diagnostic reporting. This not only enhances the quality of patient care but also contributes to cost savings and operational efficiencies across the healthcare ecosystem.
Furthermore, the Centralized Health Coordination System addresses the longstanding challenge of data fragmentation within the healthcare industry. By consolidating patient information into a secure, centralized database, this innovative technology ensures the integrity and confidentiality of sensitive health data while facilitating seamless information exchange between healthcare facilities and providers. This not only improves the continuity of care but also enhances patient safety and satisfaction.
In essence, the Centralized Health Coordination System represents a transformative leap forward in healthcare delivery, harnessing the power of digitalization to create a more connected, efficient, and patient-centric healthcare ecosystem. As healthcare organizations embrace this innovative solution, they stand poised to unlock new opportunities for innovation, collaboration, and improved patient outcomes in the ever-evolving landscape of modern medicine.
This Paper presents the Need for the providing the patient records to doctor and patient remotely also emphasize on the importance of having a digital panel for pathologist to have the editable panel for adding the records of the particular patients. This Paper will also cover many several important aspects for the same.
II. LITERATURE REVIEW
Recent progress in digitalization of medical records in health care sector has sparked interest in understanding what's already known and what questions remain unanswered. Here are some of the important points from the research paper published in this field. This literature review aims to summarize existing research and pinpoint areas where more investigation is needed. The digital transformation is a technological revolution that now penetrates every sphere our community as well as society, including health care systems. To digitalize Paper-based records in health and care, new concepts and innovative solutions are needed. [2] Such innovative solution is Electronic Health Records (EHR’s) and Personal Health Record (PHR). An Electronic Health Record (EHR) serves as a digital representation of a patient's medical history, originally documented in a paper chart, and is managed by a healthcare institution, ensuring access is restricted to authorized healthcare personnel exclusively involved in the patient's treatment (Roman, 2009).[1] Also in paper 3 there is a concept which is the use of ICT in health care is already ubiquitous and its importance is increasing rapidly. Typically, healthcare data is gathered and retained within healthcare facilities, resulting in the distribution of a patient's information across multiple locations. and stored in the local information systems (general practitioner, regional hospital, pharmacy, university hospital, physiotherapist, etc.). In Paper 4 there is a very proper result about the paper-based records versus paperless based records which is giving how crucial is digitalization of patient record in health care industry. So, compared with paper-based records, more paperless records
were fully understandable (89.2% v 69.9%, P=0.0001) and fully legible (100% v 64.3%, P < 0.0001). Paperless records were notably more prone to have least one diagnosis recorded (48.2% v 33.2%, P=0.05), to record that advice had been given (23.7% vs 10.7%, P=0.017), and Paperless records were more inclined to indicate when a referral had been initiated, to contain details of the specialty (77.4% v 59.5%, P=0.03). When a prescription had been issued, paperless records were more likely to specify the drug dose (86.6% 66.2%, P=0.005). Paperless records contained significantly more words, abbreviations, and symbols (P < 0.01 for all). At doctor interview, there was no difference between the groups for the proportion of patients or consultations that could be recalled. Doctors using paperless records were able to recall more advice given to patients (38.6% v 26.8%, P=0.03). is identified with the examination of suppositions, assumptions, assessments, perspectives, and feelings of clients, which they express via web-based networking media and other online assets.[4] In the journey of digitalization. there is a technology which is a Mobile devices and mobile health (mHealth) apps are ubiquitous, readily available approaches to collect real-time data on health behaviours, such as dietary intake, physical activity, and sleep [16-18]. mHealth apps are often designed and marketed to provide behavioural tracking and lifestyle modification support [19-22][6]. They also provide a convenient and efficient method for collecting information to advance knowledge about the relationship between obesity-related behavioural patterns and health outcomes [23-25][6].
III. METHODOLOGY AND EXPERIMENTATION
A. Pathologist Panel
- Registration and Authentication:
- The Pathologist initiates their journey by registering with the software application, providing necessary credentials and personal information.
- Upon successful registration, the Pathologist receives a unique identifier (uniquid) and sets a secure password for future authentication.
- The authentication process employs industry-standard security protocols such as encrypted transmission and secure hashing algorithms to safeguard sensitive login credentials.
- Additionally, multi-factor authentication (MFA) may be implemented to enhance security further, requiring the Pathologist to verify their identity using a secondary method, such as a one-time password (OTP) sent to their registered mobile device.
2. Access to Dashboard:
- Upon logging in, the Pathologist gains access to a sophisticated dashboard tailored to their role and responsibilities.
- The dashboard provides a centralized hub for managing patient records, featuring intuitive navigation and user-friendly interfaces designed to optimize workflow efficiency.
- Leveraging responsive web design principles, the dashboard ensures seamless accessibility across a range of devices, from desktop computers to mobile tablets, enabling the Pathologist to work flexibly in diverse clinical settings.
3. Adding Patient Records:
- Using the dashboard interface, the Pathologist can effortlessly add new patient records, capturing vital medical information such as laboratory test results, diagnostic reports, and treatment histories.
- The system employs standardized data entry forms and validation mechanisms to ensure the accuracy and completeness of the recorded information, minimizing the risk of data entry errors.
- Advanced features such as auto-population of patient demographics and integration with external laboratory equipment streamline the record creation process, saving time and reducing manual effort.
4. Previewing Records:
- Before finalizing the patient record, the Pathologist has the option to preview the entered data, allowing for thorough review and verification of all fields.
- The preview functionality enables the Pathologist to identify and rectify any discrepancies or inaccuracies in the record before submission, ensuring data integrity and quality.
- Interactive validation checks and real-time error prompts highlight potential issues, empowering the Pathologist to make informed decisions and corrections with confidence.
5. Final Submission:
- Once satisfied with the accuracy and completeness of the patient record, the Pathologist proceeds to finalize the submission.
- The submission process triggers comprehensive data validation procedures, including cross-referencing against established clinical guidelines and standards, to ensure compliance and quality assurance.
- Upon successful submission, the patient record is securely stored in the centralized database, accessible to authorized healthcare professionals for reference and analysis.
- Audit trails and version control mechanisms track changes and updates to patient records, providing a transparent record of all interactions and modifications made by the Pathologist.
By seamlessly integrating these steps into the Pathologist's workflow, the Centralized Health Coordination System enhances operational efficiency, data integrity, and patient care outcomes in the realm of pathology services.
B. Doctor Panel
- Registration and Authentication:
- The Doctor initiates their engagement by registering with the software application, providing requisite credentials and personal information.
- Upon registration, the Doctor receives a unique identifier (uniquid) and establishes a secure password for subsequent authentication purposes.
- Robust authentication mechanisms, including encryption protocols and password hashing techniques, ensure the confidentiality and integrity of login credentials.
- Optionally, the system may implement multi-factor authentication (MFA) to add an extra layer of security, requiring the Doctor to verify their identity using additional authentication factors such as a one-time password (OTP) or biometric verification.
2. Access to Dashboard:
- Upon successful authentication, the Doctor gains access to a comprehensive dashboard tailored to their role and responsibilities.
- The dashboard serves as a centralized hub for managing patient records, offering intuitive navigation and user-friendly interfaces optimized for efficient workflow management.
- Utilizing responsive design principles, the dashboard adapts seamlessly to various device types and screen sizes, facilitating flexible usage across desktop computers, tablets, and mobile devices.
3. Patient Validation and Record Access:
- Before accessing a patient's record, the Doctor must first validate the patient's identity and authorization.
- To validate a patient, the Doctor verifies their Aadhar-registered mobile number and initiates an authentication process, typically involving the generation and receipt of a one-time password (OTP) via SMS.
- Upon successful validation, the Doctor gains authorized access to the patient's medical records, ensuring data privacy and compliance with regulatory requirements.
- Advanced security features, such as role-based access control (RBAC) and access logging, further reinforce the confidentiality and integrity of patient information.
4. Adding Suggestions to Records:
- After reviewing the patient's medical record, the Doctor has the capability to provide relevant suggestions or recommendations based on their clinical assessment.
- The system facilitates seamless integration of Doctor's suggestions into the patient's record, allowing for collaborative care management and continuity of treatment.
- Documentation of Doctor's suggestions ensures comprehensive and accurate medical record keeping, supporting informed decision-making and continuity of care across healthcare providers.
5. Reviewing Past Records and Analysing Trends:
- In addition to viewing current patient records, the Doctor can access and review historical medical records to gain insights into the patient's health history and treatment trajectory.
- Advanced data visualization tools enable the Doctor to analyse trends and patterns within the patient's health data, such as fluctuations in vital parameters or laboratory test results over time.
- Trend analysis capabilities empower the Doctor to identify longitudinal changes in the patient's health status, track disease progression, and evaluate the effectiveness of interventions or treatments.
- By leveraging data-driven insights derived from comprehensive record analysis, the Doctor can make informed clinical decisions, personalize treatment plans, and optimize patient outcomes.
By seamlessly integrating these functionalities into the Doctor's workflow, the Centralized Health Coordination System enhances clinical efficiency, facilitates collaborative care management, and promotes evidence-based decision-making in healthcare delivery.
C. Patient Panel
- Registration for New Patients:
- New patients begin their interaction by registering on the portal. They provide essential personal and health details during the registration process.
- Basic information such as name, age, gender, contact details, and medical history is collected to create a comprehensive patient profile.
- Health-related details, including existing medical conditions, allergies, medications, and previous treatments, are also recorded to ensure accurate health management.
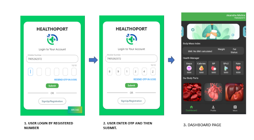
2. Login Process for Returning Patients:
- Returning patients can easily access their accounts by logging in using their registered mobile number and a one-time password (OTP) sent to their mobile device.
- This streamlined login process eliminates the need for patients to remember complex passwords and enhances the overall user experience.
3. Accessing the Dashboard:
- Upon successful login, patients are granted access to their personalized dashboard, which serves as a central hub for managing their health-related information.
- The dashboard provides a comprehensive overview of the patient's health metrics, including height, weight, body mass index (BMI), step count, and blood oxygen saturation (SPO2) levels.
- Additionally, the dashboard displays a list of body parts for which the patient has conducted tests, allowing for easy navigation and access to specific health records.
4. Viewing Health Metrics and Test Results:
- Patients can review their health metrics and test results directly from the dashboard, facilitating proactive health monitoring and management.
- Graphical representations and visualizations of health data enable patients to track trends, identify patterns, and make informed decisions about their health and well-being.
- Test results are organized and categorized based on body parts or medical conditions, enabling patients to quickly locate and review relevant health information.
- Interactive features such as zooming, filtering, and annotation tools enhance the usability of the platform, empowering patients to engage with their health data in meaningful ways.
5. Accessing Graphical Representations of Reports:
- Patients have the ability to access graphical representations of their medical reports, providing visual insights into their health status and progress.
- Graphs, charts, and trend analyses offer a clear visualization of key health indicators, facilitating better understanding and interpretation of medical information.
- By leveraging digital health records and graphical representations, patients can take an active role in managing their health, making informed decisions, and collaborating effectively with healthcare providers to achieve optimal health outcomes.
IV. CASE STUDIES AND SUCCESS STORIES
A. Kaiser Permanente
One of the largest healthcare providers in the United States, Kaiser Permanente, successfully implemented an electronic health record (EHR) system. They reported significant improvements in patient outcomes, including a reduction in medication errors by 75%, faster access to test results, and a 30% decrease in hospital admissions due to improved chronic disease management through digital records. 2. Singapore's National Electronic Health Record System [48]
B. Singapore implemented a nationwide electronic health record system
that centralized patient data across healthcare institutions. This initiative streamlined healthcare delivery, reduced administrative burdens, and allowed for better continuity of care. It led to a 15% decrease in healthcare costs over five years and improved patient satisfaction. 3. Cleveland Clinic: Adopting a comprehensive digital health strategy,
C. Cleveland Clinic
implemented various digital tools, including telehealth services and mobile health applications. This approach significantly enhanced patient engagement, reduced unnecessary visits by 50%, and improved patient compliance with treatment plans, thereby resulting in better health outcomes.
D. Rwanda's Use of mHealth Solutions
Rwanda implemented mHealth solutions to improve maternal and child healthcare. The use of mobile applications allowed community health workers to monitor pregnancies, track immunizations, and provide timely interventions. This initiative led to a significant reduction in maternal and child mortality rates.
V. PRESENTLY EXISTING SYSTEM IN THE FIELD OF DIGITALISATION OF HEALTH-CARE PATIENT REPORT
In the realm of healthcare, the digitalization of patient reports has significantly transformed the landscape, enhancing efficiency, accessibility, and patient care. Presently existing systems in this field encompass a diverse array of technologies and platforms aimed at streamlining the management and dissemination of patient information. Some key components of these systems include:
- Electronic Health Records (EHR) and Electronic Medical Records (EMR): These systems digitize patient health information, including medical history, diagnoses, medications, allergies, and laboratory test results. EHRs and EMRs facilitate seamless sharing of patient data among healthcare providers, leading to improved coordination of care and reduced medical errors.
- Health Information Exchange (HIE): HIE platforms enable the secure exchange of patient information between different healthcare organizations and systems. This interoperability fosters better care coordination, particularly for patients receiving treatment from multiple providers or across different healthcare settings.
- Telemedicine and Remote Monitoring: Telemedicine platforms allow for remote consultations between patients and healthcare professionals, leveraging technology such as video conferencing and secure messaging. Additionally, remote monitoring devices enable continuous tracking of patient vital signs and health metrics, empowering individuals to manage chronic conditions more effectively while minimizing the need for in-person visits.
- Patient Portals and Mobile Apps: Patient portals and mobile applications provide individuals with convenient access to their health records, appointment scheduling, prescription refills, and educational resources. These tools promote patient engagement and empowerment, facilitating active participation in their own healthcare journey.
- Data Analytics and Artificial Intelligence (AI): Advanced analytics and AI algorithms analyse large volumes of patient data to derive insights for personalized treatment plans, predictive modelling, population health management, and clinical decision support. These technologies hold promise for improving healthcare outcomes and optimizing resource allocation.
- Security and Compliance Measures: Given the sensitive nature of patient health information, robust security measures, such as encryption, access controls, and audit trails, are paramount to safeguarding data privacy and complying with regulatory requirements, such as the Health Insurance Portability and Accountability Act (HIPAA).
Overall, the digitalization of healthcare patient reports represents a transformative shift towards a more interconnected, data-driven, and patient-centric healthcare ecosystem, with ongoing advancements continuously shaping the future of healthcare delivery and outcomes
VI. RESULTS AND DISCUSSION
A. Patient Panel
The implementation of the Centralized Health Coordination System (CHCS) has yielded significant benefits for both healthcare providers and patients alike. One of the key outcomes of this technology is the development of a user-friendly application interface that empowers patients to actively engage in their healthcare journey.
Through the CHCS application, patients can easily log in and sign up, gaining immediate access to their medical records and health-related information. This accessibility enhances transparency and promotes patient-centered care, allowing individuals to take ownership of their health data.
Moreover, the CHCS application enables patients to record and monitor various health metrics, including SpO2 levels, number of steps taken, body mass index (BMI), and more. This functionality empowers patients to track their progress, identify trends, and make informed decisions about their lifestyle and healthcare choices.
For example, patients can regularly monitor their SpO2 levels, particularly relevant for individuals with respiratory conditions such as asthma or chronic obstructive pulmonary disease (COPD). By tracking SpO2 levels over time, patients can detect any fluctuations or abnormalities, allowing for early intervention and improved disease management.
Similarly, the ability to monitor the number of steps taken and BMI enables patients to track their physical activity levels and weight management progress. This promotes a proactive approach to health and wellness, encouraging patients to adopt healthier lifestyle habits and prevent chronic diseases associated with sedentary behavior and obesity.
The graphical representations and trend analyses provided by the CHCS application offer valuable insights into patients' health status and progress. Visualizing health data in this manner facilitates better understanding and interpretation, empowering patients to make informed decisions about their healthcare.
Overall, the CHCS application serves as a valuable tool for patient empowerment and engagement, facilitating proactive health monitoring, informed decision-making, and collaboration with healthcare providers. By leveraging technology to empower patients, the CHCS contributes to improved health outcomes and enhanced quality of care in the modern healthcare landscape.
B. Doctor Panel & Pathologist Panel
The Centralized Health Coordination System (CHCS) offers a comprehensive solution not only for patients but also for healthcare providers, particularly doctors. Through the CHCS application, doctors gain access to a range of features and functionalities that enhance clinical efficiency, promote collaborative care management, and support evidence-based decision-making.
One of the primary benefits of the CHCS application for doctors is streamlined access to patient records and medical information. Doctors can log in securely to the system and retrieve patient records with ease, regardless of their location or the healthcare facility where the records are stored. This accessibility facilitates continuity of care, allowing doctors to review patients' medical histories, diagnoses, medications, and treatment plans quickly and efficiently.
Furthermore, the CHCS application enables doctors to add relevant suggestions or recommendations to patient records based on their clinical assessments. This feature supports collaborative care management, as doctors can communicate important insights, instructions, or follow-up recommendations directly within the patient's record. By documenting their suggestions, doctors contribute to comprehensive and accurate medical record-keeping, ensuring continuity of care across healthcare providers.
The ability to review past records and analyze trends within the CHCS application is another valuable feature for doctors. By accessing historical medical records, doctors can gain insights into patients' health histories, treatment trajectories, and disease progression over time. Advanced data visualization tools facilitate trend analysis, enabling doctors to identify longitudinal changes in patients' health status, track the effectiveness of interventions or treatments, and make data-driven clinical decisions.
Moreover, the CHCS application supports seamless collaboration and communication among healthcare providers through secure messaging and information sharing functionalities. Doctors can consult with specialists, refer patients to other healthcare professionals, and coordinate care plans efficiently within the system. This interdisciplinary collaboration enhances patient care outcomes, promotes continuity of care, and reduces the likelihood of medical errors or duplicative tests.
Overall, the CHCS application empowers doctors with the tools and resources necessary to deliver high-quality, patient-centered care in today's digital healthcare landscape. By facilitating efficient access to patient records, promoting collaborative care management, and enabling data-driven decision-making, the CHCS enhances clinical efficiency, improves patient outcomes, and contributes to the advancement of modern medicine.
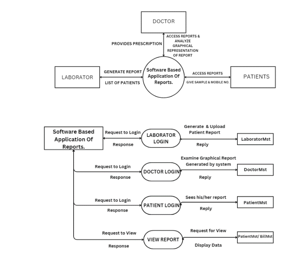
C. O Level DFD of the entire module

D. 1 Level DFD of the entire module
VII. ADVANTAGES OF DIGITAL PATHOLOGY:
- Efficiency: Digital pathology streamlines the workflow by digitizing slide analysis, reducing the time required for processing, reviewing, and sharing results. This expedites diagnosis and subsequent treatment.
- Enhanced Collaboration: It allows pathologists to collaborate remotely, facilitating consultations with specialists worldwide. This improves diagnostic accuracy, encourages second opinions, and aids in complex case discussions.
- Accessibility and Sharing: Digital slides are easily accessible and shareable among multiple professionals simultaneously. This accessibility promotes educational purposes, facilitates consultations, and allows for quicker decision-making for patient care.
- Data Preservation and Retrieval: Digital slides can be stored, indexed, and retrieved more efficiently than physical slides. This facilitates long-term preservation of pathology specimens, supports retrospective analysis, research, and quality assurance initiatives.
- Integration with Technology: Digital pathology integrates seamlessly with artificial intelligence (AI) algorithms and analytics tools. This integration enables faster image analysis, pattern recognition, and potential automation in identifying abnormalities, leading to more accurate diagnoses and predictions
VIII. DISADVANTAGES OF DIGITAL PATHOLOGY
- Cost: Transitioning to digital pathology involves substantial initial investment in equipment, software, and infrastructure. This financial outlay might pose challenges, especially for smaller healthcare facilities or resourcelimited settings.
- Training and Adaptation: Pathologists and lab technicians need training to adapt to digital systems. Resistance to change or lack of expertise in handling digital tools might hinder the smooth adoption of digital pathology, requiring additional resources for training and support.
- Security and Privacy Concerns: Digital pathology introduces concerns about data security and patient privacy. Ensuring compliance with regulations (such as HIPAA) to protect patient information in digital formats is crucial. Securing digital systems against cyber threats becomes paramount.
- Technical Challenges: Quality issues related to digital image acquisition, network connectivity for remote access, and standardization of digital pathology formats might arise. These technical challenges can impact the accuracy of diagnoses and remote consultations.
- Regulatory and Legal Considerations: There might be regulatory hurdles and legal considerations specific to digital pathology. Validating and ensuring the acceptance of digital images for diagnostic purposes within legal frameworks may present challenges
IX. ADVANTAGE OF THE PROPOSED SYSTEM
- Efficiency: The project streamlines the process of delivering and accessing health reports, reducing the time and effort required for both patients and healthcare providers. This efficiency can lead to faster diagnosis and treatment.
- Accessibility: Patients can access their health reports instantly through a digital platform, promoting transparency and patient engagement in their healthcare. This accessibility empowers patients to take control of their health.
- Reduced Paperwork: By eliminating the need for paper-based reports and records, the project significantly reduces the administrative burden on healthcare facilities. This reduction in paperwork can save time and resources.
- Enhanced Data Security: Digital records offer advanced security measures to protect sensitive patient data, reducing the risk of data breaches. This ensures the confidentiality and integrity of patient information.
- Historical Trend Analysis: The digital repository of health records allows for the analysis of historical trends, which can lead to better-informed healthcare decisions and more effective treatments. This data-driven approach can improve patient outcomes and overall healthcare quality.
X. LIMITATION OF PROPOSED SYSTEM
- Technical Challenges: Technical issues such as system outages, software glitches, or data synchronization problems can disrupt the seamless flow of health information.
- Resistance to Change: Healthcare professionals and institutions may resist shifting from traditional paper-based processes to digital solutions due to familiarity with existing practices.
XI. ACKNOWLEDGEMENT
I extend my heartfelt gratitude to Shri Ramswaroop Memorial College of Engineering and Management for their invaluable guidance and unwavering support throughout the duration of this project. Special thanks are due to my guide and project coordinator, Ma’am Sarika, whose consistent support and administrative assistance were instrumental in navigating through the challenges.
I am deeply indebted to my acquaintances whose generous support made this project achievable. Their encouragement and belief in my endeavours spurred me on even in the face of obstacles.
Lastly, I would like to express my sincere appreciation to the study participants whose willingness to share their time and insights enriched this project immeasurably. Their contributions have been integral to its success.
Conclusion
In conclusion, the trajectory of healthcare\'s evolution towards digital integration represents a profound shift that promises substantial benefits while posing a few inevitable challenges. The transition from paper-based systems to comprehensive digital solutions signifies a paradigmatic leap toward efficiency, accessibility, and improved patient engagement. By offering immediate access to records, empowering patients to actively manage their health, and reducing administrative burdens, digital systems hold the potential to revolutionize healthcare delivery. However, navigating technical hurdles and overcoming entrenched resistance within the healthcare community to embrace these digital transformations remain pivotal. Addressing these challenges will be instrumental in harnessing the full potential of digital integration, ensuring enhanced data security, fostering informed decision-making through historical trend analysis, and ultimately, delivering a more interconnected and patient-centric healthcare landscape. The journey towards digital integration in healthcare signifies not just a technological shift but a fundamental reimagining of healthcare delivery, promising a future where efficiency, accessibility, and patient care converge harmoniously for the benefit of all. In this project, we will have the data of a patient\'s previous blood reports and their current report. 1) Using graphical analysis, we will develop a doctor recommendation system so that the patient can seek advice from a doctor in the future. 2) Further an AI Chatbot will also be implemented in future for acting as a help desk for patient. 3) Also, we will add a functionality in which patient can upload his prescription of medicine and can get the information regarding the pros and cons of the medicine which is prescribed to them.
References
[1] Seymour, T., Frantsvog, D., & Graeber, T. (2012). Electronic health records (EHR). American Journal of Health Sciences (AJHS), 3(3), 201-210. [2] Serbanati, L. D. (2020). Health digital state and Smart EHR systems. Informatics in Medicine Unlocked, 21, 100494. [3] Bakker, A. R. (2007). The need to know the history of the use of digital patient data, in particular the EHR. International Journal of Medical Informatics, 76(5-6), 438-441. [4] Hippisley-Cox, J., Pringle, M., Cater, R., Wynn, A., Hammersley, V., Coupland, C., ... & Johnson, C. (2003). The electronic patient record in primary care—regression or progression? A cross sectional study. Bmj, 326(7404), 1439-1443. [5] Shickel, B., Tighe, P. J., Bihorac, A., & Rashidi, P. (2017). Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE journal of biomedical and health informatics, 22(5), 1589-1604. [6] Coughlin, J. W., Martin, L. M., Zhao, D., Goheer, A., Woolf, T. B., Holzhauer, K., ... & Bennett, W. L. (2022). Electronic Health Record–Based Recruitment and Retention and Mobile Health App Usage: Multisite Cohort Study. Journal of medical Internet research, 24(6), e34191. [7] Genes, N., Violante, S., Cetrangol, C., Rogers, L., Schadt, E. E., & Chan, Y. F. Y. (2018). From smartphone to EHR: a case report on integrating patient-generated health data. NPJ digital medicine, 1(1), 23. Mandl, K. D., Gottlieb, D., & Ellis, A. (2019). Beyond one-off integrations: a commercial, substitutable, reusable, standardsbased, electronic health record–connected app. Journal of Medical Internet Research, 21(2), e12902. [8] Ford, E. W., Menachemi, N., & Phillips, M. T. (2006). Predicting the adoption of electronic health records by physicians: when will health care be paperless?. Journal of the American Medical Informatics Association, 13(1), 106-112. [9] Adler-Milstein, J., & Bates, D. W. (2010). Paperless healthcare: Progress and challenges of an IT-enabled healthcare system. Business Horizons, 53(2), 119-130. [10] Niazi, M. K. K., Parwani, A. V., & Gurcan, M. N. (2019). Digital pathology and artificial intelligence. The lancet oncology, 20(5), e253-e261. [11] Jahn, S. W., Plass, M., & Moinfar, F. (2020). Digital pathology: advantages, limitations and emerging perspectives. Journal of clinical medicine, 9(11), 3697. [12] Baidoshvili, A., Bucur, A., van Leeuwen, J., van der Laak, J., Kluin, P., & van Diest, P. J. (2018). Evaluating the benefits of digital pathology implementation: time savings in laboratory logistics. Histopathology, 73(5), 784-794. [13] Holten-Rossing, H. Digitalization in pathology. [14] Hanna, M. G., Ardon, O., Reuter, V. E., Sirintrapun, S. J., England, C., Klimstra, D. S., & Hameed, M. R. (2022). Integrating digital pathology into clinical practice. Modern Pathology, 35(2), 152- 164. [15] Volynskaya, Z., Chow, H., Evans, A., Wolff, A., Lagmay-Traya, C., & Asa, S. L. (2018). Integrated pathology informatics enables high-quality personalized and precision medicine: digital pathology and beyond. Archives of pathology & laboratory medicine, 142(3), 369-382. [16] Hanna, M. G., Reuter, V. E., Ardon, O., Kim, D., Sirintrapun, S. J., Schüffler, P. J., ... & Hameed, M. (2020). Validation of a digital pathology system including remote review during the COVID-19 pandemic. Modern Pathology, 33(11), 2115-2127. [17] Fraggetta, F., L’imperio, V., Ameisen, D., Carvalho, R., Leh, S., Kiehl, T. R., ... & Eloy, C. (2021). Best practice recommendations for the implementation of a digital pathology workflow in the anatomic pathology laboratory by the European Society of Digital and Integrative Pathology (ESDIP). Diagnostics, 11(11), 2167. [18] Kwiatkowska, E. M., & Skórzewska-Amberg, M. (2019). Digitalisation of Healthcare and the Problem of Digital Exclusion. Central European Management Journal, 27, 48-63. [19] Botrugno, C. (2021). Information technologies in healthcare: Enhancing or dehumanising doctor–patient interaction?. Health, 25(4), 475-493. [20] Popov, V. V., Kudryavtseva, E. V., Kumar Katiyar, N., Shishkin, A., Stepanov, S. I., & Goel, S. (2022). Industry 4.0 and digitalisation in healthcare. Materials, 15(6), 2140. [21] Shaharul, N. A., Ahmad Zamzuri, M. A. I., Ariffin, A. A., Azman, A. Z. F., & Mohd Ali, N. K. (2023). Digitalisation Medical Records: Improving Efficiency and Reducing Burnout in Healthcare. International Journal of Environmental Research and Public Health, 20(4), 3441. [22] Veikkolainen, P., Tuovinen, T., Jarva, E., Tuomikoski, A. M., Männistö, M., Pääkkönen, J., ... & Reponen, J. (2023). eHealth competence building for future doctors and nurses–Attitudes and capabilities. International Journal of Medical Informatics, 169, 104912. [23] Tomar, S., Gupta, M., Rani, M., & Shyam, H. S. (2023, March). Healthcare Digitalisation: Understanding Emerging Technological Trends. In 2023 9th International Conference on Advanced Computing and Communication Systems (ICACCS) (Vol. 1, pp. 2459-2463). IEEE. [24] Gy?rffy, Z., Radó, N., & Mesko, B. (2020). Digitally engaged physicians about the digital health transition. PLoS One, 15(9), e0238658. [25] Williams, F., & Boren, S. A. (2008). The role of the electronic medical record (EMR) in care delivery development in developing countries: a systematic review. Informatics in primary care, 16(2). [26] Heart, T., Ben-Assuli, O., & Shabtai, I. (2017). A review of PHR, EMR and EHR integration: A more personalized healthcare and public health policy. Health Policy and Technology, 6(1), 20-25. [27] Belden, J. L., Grayson, R., & Barnes, J. (2009). [27] Defining and testing EMR usability: Principles and proposed methods of EMR usability evaluation and rating. Healthcare Information and Management Systems Society (HIMSS). [28] Bhavnani, S. P., Parakh, K., Atreja, A., Druz, R., Graham, G. N., Hayek, S. S., ... & Shah, B. R. (2017). 2017 Roadmap for innovation—ACC health policy statement on healthcare transformation in the era of digital health, big data, and precision health: a report of the American College of Cardiology Task Force on Health Policy Statements and Systems of Care. Journal of the American College of Cardiology, 70(21), 2696-2718.
Copyright
Copyright © 2024 Ekta Yadav, Er. Sarika Singh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET62687
Publish Date : 2024-05-25
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online