Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
An Alternative and Complementary Approach to Stress Caused by Sleep Deprivation: A Review
Authors: Anchal Patel, Shajeel Ahmad, Anjali Singh, Vineeta Kumari, Km.Dolly Chaudhary, Shwet Kumar, Dr. Sachin Neekhra, Dr. Alok Kumar Shukla
DOI Link: https://doi.org/10.22214/ijraset.2025.66503
Certificate: View Certificate
Abstract
Lack of sleep is a prevalent issue in contemporary society, often leading to considerable stress that negatively affects physical, emotional, and cognitive health. Traditional treatments, like drug therapies, are effective but often come with side effects, risks of dependency, and limited long-term benefits. Consequently, alternative and complementary methods are becoming more popular as viable, holistic solutions for alleviating stress resulting from sleep deprivation. These techniques encompass mindfulness-based practices, herbal remedies, dietary changes, physical exercise, and mind-body therapies. This paper examines the evidence backing these alternative methods and their mechanisms in reducing stress while improving sleep quality and overall wellness. Moreover, cognitive-behavioral therapy for insomnia (CBT-I) addresses the cognitive misconceptions tied to sleep deprivation, reducing stress while encouraging healthier sleep patterns. Complementary technologies, including biofeedback and wearable sleep monitors, further assist in managing stress by supplying real-time information to enhance interventions.
Introduction
I. INTRODUCTION
A. Definition of Sleep and Its Biological Importance
Sleep is a naturally occurring, reversible state of diminished awareness and sensory function crucial for the physical and mental rejuvenation of the body. It is governed by the circadian rhythm, which aligns the timing of sleeping and waking, and the homeostatic sleep drive, which heightens the requirement for sleep the longer a person stays awake. Sleep facilitates numerous biological functions, such as memory consolidation, immune system performance, and cellular repair..
B. Definition of Stress and Its Psychological and Physiological Component
Stress signifies the physiological and psychological reaction to external or internal pressures (stressors) that jeopardize an individual's homeostasis or well-being. Psychologically, stress encompasses emotions of tension, anxiety, or worry, whereas physiologically, it initiates the activation of the hypothalamic-pituitary-adrenal (HPA) axis, resulting in the release of cortisol and other stress hormones.
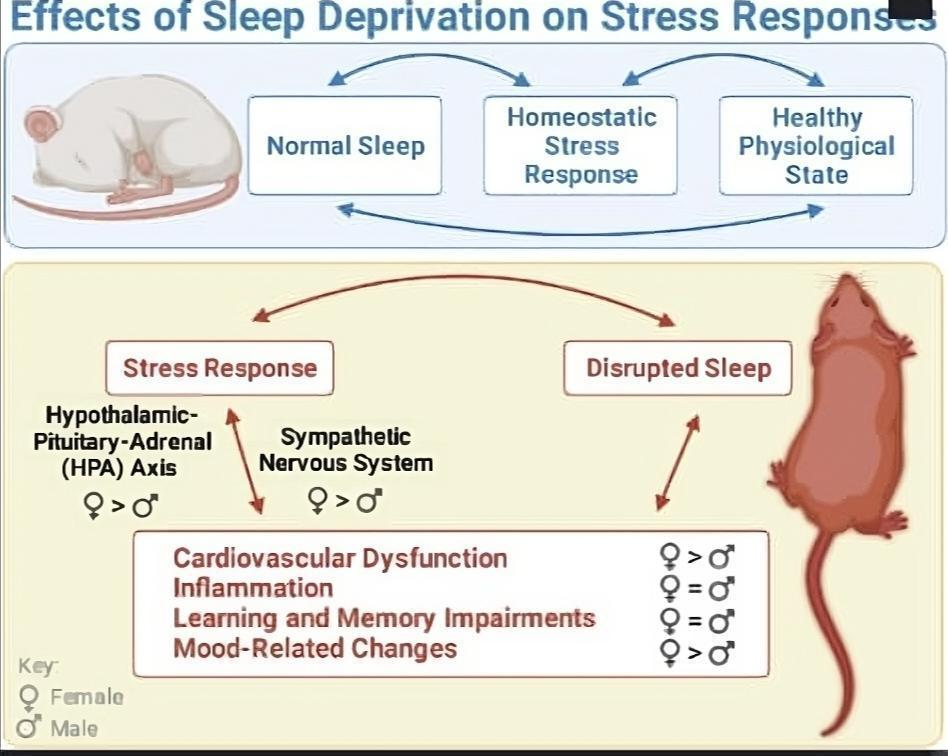
Effect of sleep deprivation on stress response
(Fig.1)
Sleep and stress are closely connected, with insufficient sleep frequently causing stress and ongoing stress detrimentally influencing sleep. Insufficient sleep raises cortisol levels, which can worsen the body's stress response. Sleep deprivation can hinder emotional regulation, resulting in increased stress sensitivity and diminished coping mechanisms (Fernandes et al. , 2020). In contrast, stress can interfere with sleep by stimulating the HPA axis and amplifying sympathetic nervous system activity, hindering the ability to fall asleep or stay asleep.
Table 1.
Medicinal Plants Used for Anxiety, Depression or Stress Treatment
|
S.No. |
PLANTS
|
CONSTITUENTS |
|
1. |
Hops (Humulus lupulus L) |
Hops (Humulus lupulus L) Resins (Alpha-acid and Beta-acid, Polyphenols, Flavonoids, Essential oils, Proteins, lipid, waxes, Humulene, Xantholhumol, cellulose. |
|
2. |
Kava-Kava (Piper methysticum G. Forst) |
Kava-Kava (Piper methysticum G. Forst). Kavalactones (Anxiolytic property), Starch (43%), Fibres (20%), Sugar (3. 2%), Proteins, minerals (3. 2%). |
|
3. |
Lavender (Lavandula angustifolia mill) |
Linalool, Linalyl acetate, 1,8-cineole, Beta-Ocimene, Terpinen-4-ol, Camphor.
|
|
4. |
Lemon Balm (Melissa officinalis L. ) |
Flavonoids (antioxidant property), Terpenes, Vitamin C, Essential oils (0. 25-0. 38%), Phenolic Compounds (caffeic acid, phenolic acid). |
|
5. |
Maypop (Passiflora incarnata) |
Maypop (Passiflora incarnata) Flavonoids, alkaloids, B2F (antianxiety effect), Nitrogen, potassium, phosphorus. Maypop (Passiflora incarnata) Flavonoids, alkaloids, B2F (antianxiety effect), Nitrogen, potassium, phosphorus. |
|
6. |
Peppermint (Mentha piperita L. )
|
Menthol, Menthone, Menthyl acetate, Menthofuran, Terpenoids, Flavonoids. Peppermint (Mentha piperita L. ) Menthol, Menthone, Menthyl acetate, Menthofuran, Terpenoids, Flavonoids. |
|
7. |
Saffron (Crocus Sativus L. ) |
Vitamins, Minerals (calcium, sodium, zinc), Carbohydrates (Starch, gums, pectin, sugar), Proteins (12%), Fat (5%), Crude fibre (5%), Moisture (10%), Secondary metabolites (crocins, Crocetin). Saffron (Crocus Sativus L. ) Vitamins, Minerals (calcium, sodium, zinc), Carbohydrates (Starch, gums, pectin, sugar), Proteins (12%), Fat (5%), Crude fibre (5%), Moisture (10%), Secondary metabolites (crocins, Crocetin). |
|
8. |
Valerian (Valeriana officinalis L. )
|
Flavonoids, Alkaloids, Amino acids, Monoterpenes, and Sesquiterpenes. Valerian (Valeriana officinalis L.) Flavonoids, Alkaloids, Amino acids, Monoterpenes, and Sesquiterpenes. |
II. MECHANISMS OF SLEEP DEPRIVATION-INDUCED STRESS
A. Physiological Mechanisms
a. Disruption of the Hypothalamic-Pituitary-Adrenal (HPA) Axis
The HPA axis serves as a vital part of the body's stress response system, orchestrating the release of cortisol, the main stress hormone. When normal functioning of the HPA axis is disrupted by sleep deprivation, cortisol levels increase, which can intensify stress responses. Long-term sleep deprivation may lead to a dysregulated HPA axis, marked by elevated basal cortisol secretion and an exaggerated cortisol response to stress.
b. Alterations in Cortisol and Other Stress Hormones (e. g. , Adrenaline, Noradrenaline)
While sleep deprivation is associated with heightened cortisol levels, it also affects other hormones related to stress, including adrenaline and noradrenaline. Released by the sympathetic nervous system and adrenal glands, these hormones are crucial for the body's "fight or flight" response to stress. Chronic sleep deprivation results in prolonged activation of these systems, which can cause physiological changes such as an increased heart rate, elevated blood pressure, and heightened arousal states.
c. Impact on Autonomic Nervous System (e. g. , Increased Sympathetic Activity, Reduced Parasympathetic Response)
The autonomic nervous system (ANS) governs involuntary bodily functions like heart rate, digestion, and respiration. Sleep deprivation alters the equilibrium between the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). Normally, the PNS facilitates relaxation and recovery during sleep, while the SNS is stimulated during stress or physical activity. Increased sympathetic activity resulting from sleep deprivation leads to elevated levels of physiological arousal, concurrently diminishing parasympathetic activity, which hinders the body's capability to revert to a state of calm post-stress.
d. Sleep Deprivation and Inflammation (Cytokines, Immune Response)
Sleep is essential for sustaining immune function, and research shows that sleep deprivation elevates levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These cytokines are integral to the body's immune response and play a role in controlling inflammation. Such inflammation aggravates the body's stress response, establishing a feedback loop that exacerbates both sleep deprivation and stress (Reynolds et al. , 2013).
III. MECHANISMS OF SLEEP DEPRIVATION-INDUCED STRESS
A. Physiological Mechanisms
1) Disruption of the Hypothalamic-Pituitary-Adrenal (HPA) Axis
The HPA axis serves as a vital part of the body's stress response system, orchestrating the release of cortisol, the main stress hormone. When normal functioning of the HPA axis is disrupted by sleep deprivation, cortisol levels increase, which can intensify stress responses. Long-term sleep deprivation may lead to a dysregulated HPA axis, marked by elevated basal cortisol secretion and an exaggerated cortisol response to stress.
2) Alterations in Cortisol and Other Stress Hormones (e. g. , Adrenaline, Noradrenaline)
While sleep deprivation is associated with heightened cortisol levels, it also affects other hormones related to stress, including adrenaline and noradrenaline. Released by the sympathetic nervous system and adrenal glands, these hormones are crucial for the body's "fight or flight" response to stress. Chronic sleep deprivation results in prolonged activation of these systems, which can cause physiological changes such as an increased heart rate, elevated blood pressure, and heightened arousal states.
3) Impact on Autonomic Nervous System (e. g. , Increased Sympathetic Activity, Reduced Parasympathetic Response)
The autonomic nervous system (ANS) governs involuntary bodily functions like heart rate, digestion, and respiration. Sleep deprivation alters the equilibrium between the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). Normally, the PNS facilitates relaxation and recovery during sleep, while the SNS is stimulated during stress or physical activity. Increased sympathetic activity resulting from sleep deprivation leads to elevated levels of physiological arousal, concurrently diminishing parasympathetic activity, which hinders the body's capability to revert to a state of calm post-stress.
4) Sleep Deprivation and Inflammation (Cytokines, Immune Response)
Sleep is essential for sustaining immune function, and research shows that sleep deprivation elevates levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). These cytokines are integral to the body's immune response and play a role in controlling inflammation. Such inflammation aggravates the body's stress response, establishing a feedback loop that exacerbates both sleep deprivation and stress (Reynolds et al. , 2013).
B. Neurobiological Mechanisms
1) Changes in Brain Activity and Neural Circuitry (e. g. , Prefrontal Cortex, Amygdala)
Sleep deprivation modifies the activity within crucial brain regions responsible for processing stress, notably the prefrontal cortex (PFC) and the amygdala. The PFC, which oversees higher cognitive abilities like decision-making, emotional regulation, and executive control, shows diminished activity during instances of sleep deprivation. This decline in PFC function hampers the regulation of emotional responses to stress. Concurrently, the amygdala, which is engaged in emotional processing and fear responses, becomes overactive, resulting in heightened emotional reactivity and stress sensitivity. The disparity between the PFC and amygdala is believed to contribute to increased susceptibility to stress and compromised emotional regulation following sleep deprivation.
2) Sleep Deprivation and Its Effect on Emotional Regulation and Decision-Making
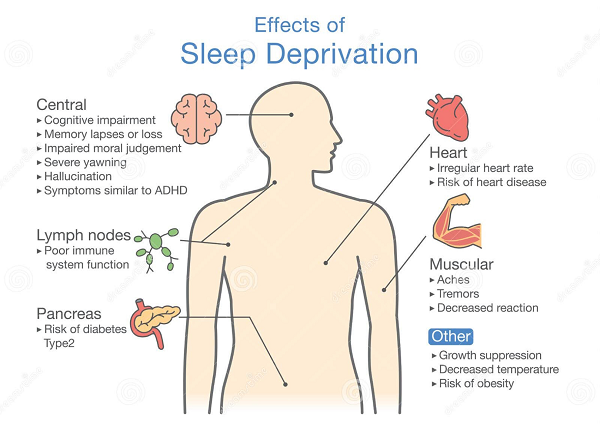
(Fig.2)
Sleep deprivation impairs emotional regulation by reducing the brain's ability to manage negative emotions effectively. A decrease in PFC activity and increased amygdala reactivity leads to heightened emotional responses to stressors, making individuals more prone to anxiety, irritability, and negative mood state. This lack of emotional regulation and poor decision-making further exacerbates stress and can contribute to the development of mental health disorders.
3) Neurotransmitters Involved in Sleep and Stress (e.g., Serotonin, Dopamine, GABA)
Neurotransmitters play a crucial role in both sleep regulation and stress response. For example, serotonin, which is involved in mood regulation and sleep-wake cycles, is often found to be dysregulated during periods of sleep deprivation. Dopamine, a neurotransmitter involved in motivation and reward processing, is also affected by sleep loss, leading to impaired motivation and an increased desire for stimulating, rewarding activities. GABA (gamma-aminobutyric acid), an inhibitory neurotransmitter that helps induce relaxation and sleep, may be reduced during sleep deprivation, impairing the body's ability to relax and manage stress effectively. These neurochemical changes contribute to the heightened stress response and the difficulty in achieving restorative sleep.
C. Psychological Mechanisms
1) Impact on Mood, Cognition, and Emotional Reactivity
Sleep deprivation has significant effects on mood, cognition, and emotional reactivity. Individuals who are sleep-deprived tend to experience more negative moods, greater irritability, and increased emotional volatility. The combination of emotional and cognitive difficulties heightens the perceived stress, leading to a vicious cycle of poor sleep and increased stress levels.
2) Increased Vulnerability to Anxiety, Depression, and Other Stress-Related Disorders
Sleep deprivation has been strongly associated with increased vulnerability to anxiety, depression, and other mood disorders . The dysregulation of neurotransmitter systems (e.g., serotonin, dopamine) and the brain regions involved in emotional regulation (e.g., prefrontal cortex, amygdala) make individuals more susceptible to developing stress-related psychiatric conditions.
3) Impaired Coping Strategies and Diminished Resilience to Stress
Sleep deprivation impairs an individual's ability to cope with stress. When well-rested, individuals can typically employ adaptive coping strategies, such as problem-solving, emotional regulation, and social support. This reduction in coping
ability, combined with heightened stress sensitivity, decreases overall resilience to stress, increasing the likelihood of developing chronic stress and its associated health impacts.
IV. LONG-TERM CONSEQUENCES OF CHRONIC SLEEP DEPRIVATION AND STRESS
A. Physical Health Risks
1) Cardiovascular Disease (Hypertension, Heart Disease)
Chronic sleep deprivation, particularly when accompanied by high levels of stress, is a significant risk factor for cardiovascular disease. Sleep deprivation leads to increased sympathetic nervous system activity and dysregulated cortisol levels, both of which contribute to elevated blood pressure and an increased heart rate. Over time, this prolonged activation of the stress response system can lead to chronic hypertension, a major risk factor for heart disease, stroke, and other cardiovascular conditions.
2) Metabolic Disturbances (e.g., Obesity, Diabetes)
Chronic sleep deprivation and stress are closely associated with metabolic disturbances, including obesity and type 2 diabetes. Sleep loss negatively affects appetite-regulating hormones, such as ghrelin (which stimulates appetite) and leptin (which signals fullness), leading to overeating and poor dietary choices. Studies show that chronic sleep deprivation and stress contribute to abdominal fat accumulation, which is particularly harmful due to its association with cardiovascular and metabolic diseases.
3) Impaired Immune System Functioning
Both sleep deprivation and chronic stress can impair immune function, making individuals more susceptible to infections and illness. Sleep is crucial for maintaining proper immune response, and its disruption weakens the body's ability to fight pathogens. Sleep deprivation leads to a reduction in the production of cytokines, which are essential for initiating an immune response (Irwin, 2015)
B. Mental Health Risks
1) Chronic Anxiety, Depression, and Other Mood Disorders
Long-term sleep deprivation and stress are closely associated with the onset of mood disorders, such as chronic anxiety and depression. The lack of sleep hinders emotional regulation and raises the chance of encountering negative emotional states including irritability, sadness, and anxiety. Frequently, sleep disturbances are reported as a coexisting symptom in those suffering from anxiety and depression, and ongoing sleep loss can heighten the risk of these conditions developing.
2) Increased Risk of Developing Post-Traumatic Stress Disorder (PTSD)
Chronic sleep deprivation, especially when linked with persistent stress, may raise the susceptibility to the development of post-traumatic stress disorder (PTSD) after experiencing traumatic events. Sleep is vital for processing emotional memories and enabling recovery from trauma. However, a lack of adequate sleep disrupts this mechanism and can result in more intrusive and lasting memories of the traumatic incident. Individuals with a history of sleep problems or ongoing stress are at an elevated risk for developing PTSD and suffering from more intense symptoms.
3) Long-Term Cognitive Decline and Potential Neurodegenerative Conditions
Research indicates that chronic sleep deprivation adversely affects brain health, contributing to lasting cognitive decline and increasing the potential for neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease. Sleep is essential for removing waste products from the brain, including beta-amyloid plaques, which are linked to Alzheimer's disease. Insufficient sleep interrupts this cleaning process, causing the buildup of harmful proteins in the brain and raising the chances of neurodegeneration. Altogether, chronic sleep deprivation and stress play a role in the acceleration of cognitive decline and the emergence of neurodegenerative conditions in older adults.
C. Impact on Quality of Life
1) Reduced Overall Well-Being and Life Satisfaction
Chronic sleep deprivation and stress can significantly lower an individual’s overall quality of life. The enduring effects on physical and mental health, alongside cognitive performance, lead to a general decline in well-being. Individuals suffering from sleep deprivation often report a reduced satisfaction with life, as their ability to engage in daily activities is compromised due to fatigue, irritability, and decreased cognitive function.
2) Impaired Relationships, Social Interactions, and Personal Development
The consequences of ongoing sleep deprivation and stress influence an individual's social connections and relationships. People who do not get enough sleep frequently exhibit reduced social participation and are less inclined to engage in social events, which can result in feelings of seclusion. Persistent irritability, emotional instability, and ineffective communication abilities can put a strain on relationships with family, friends, and coworkers, leading to social retreat and discord.
V. STRATEGIES FOR MANAGING SLEEP DEPRIVATION-INDUCED STRESS
A. Sleep Hygiene and Cognitive Behavioural Therapy (CBT)
1) Importance of Maintaining Healthy Sleep Habits
Maintaining good sleep hygiene is crucial for alleviating the consequences of stress linked to sleep deprivation. Healthy sleeping practices encompass keeping a regular sleep timetable (going to bed and rising at the same time each day), enhancing the sleep environment (e. g. , minimizing noise, regulating light and temperature), and steering clear of stimulants (like caffeine or nicotine) near bedtime. A consistent sleeping schedule aids in regulating the body's internal circadian rhythm, enhancing both the amount and quality of sleep.
2) Cognitive Behavioural Therapy for Insomnia (CBT-I)
Cognitive Behavioural Therapy for Insomnia (CBT-I) is a very effective approach for treating sleep-related stress and insomnia. CBT-I focuses on identifying and modifying thoughts and behaviors that interfere with sleep. It incorporates strategies such as stimulus control, sleep restriction, and cognitive restructuring to confront negative thought patterns related to sleep. Research has demonstrated that CBT-I not only enhances sleep quality but also alleviates anxiety and stress by assisting individuals in managing the psychological components that contribute to sleep issues.
B. Stress Management Techniques
1) Mindfulness-Based Stress Reduction (MBSR) and Relaxation Techniques
Mindfulness-Based Stress Reduction (MBSR) is a recognized program that employs mindfulness meditation to decrease stress and enhance psychological well-being. MBSR has proven effective in lowering cortisol levels, fostering emotional regulation, and improving sleep quality in those under stress. These methods stimulate the parasympathetic nervous system, diminishing the fight-or-flight reaction and encouraging relaxation.
2) Time Management Strategies to Reduce Stress Levels
Efficient time management is a potent approach for handling stress and alleviating the effects of sleep deprivation. Chronic stress often stems from a perception of time limitation, excessive workloads, and disorganized daily schedules. Time management strategies, such as task prioritization, dividing larger tasks into smaller, manageable components, and establishing realistic deadlines, can help to lessen the sensation of overwhelm.
C. Pharmacological Interventions
1) Role of Medications (e. g. , Anxiolytics, Antidepressants) in Managing Stress
For those experiencing chronic stress, medications like anxiolytics (e. g. , benzodiazepines) and antidepressants (e. g. , SSRIs, SNRIs) may be recommended to alleviate anxiety and depressive symptoms. Such medications can offer temporary relief from the mental impacts of stress, aiding individuals in regaining emotional balance. Furthermore, medications like benzodiazepines can disrupt the sleep cycle, potentially resulting in dependence and withdrawal symptoms.
2) Sleep Aids and Their Potential Side Effects (e. g. , Benzodiazepines, Melatonin)
Sleep aids, including benzodiazepines (e. g. , lorazepam, diazepam) and over-the-counter supplements such as melatonin, are commonly utilized to address sleep deprivation. While benzodiazepines can effectively induce sleep, their prolonged usage is not recommended due to the potential for dependency, tolerance, and withdrawal symptoms. In contrast, melatonin is a natural hormone that manages the sleep-wake cycle and is regarded as a safer option for enhancing sleep onset in those dealing with circadian rhythm disturbances. Nevertheless, its efficacy might differ based on the individual's specific sleep disorder as well as the dosage administered.
3) Investigating the Use of Newer Pharmacological Agents Targeting Both Sleep and Stress
Recent studies have examined the possibilities of newer pharmacological agents aimed at addressing both sleep regulation and stress relief. For instance, medications like suvorexant, which functions as an orexin receptor antagonist, assist in regulating the sleep-wake cycle by facilitating sleep without the sedative impacts of conventional sleep medications.
D. Lifestyle Modifications
1) Regular Physical Activity and Its Impact on Sleep and Stress Regulation
Regular physical activity is among the most effective methods to enhance both sleep and stress management. Exercise has been demonstrated to elevate the release of endorphins, which are natural mood boosters, and to lower levels of stress hormones such as cortisol. Additionally, exercise is essential in sustaining healthy metabolic operations, which can alleviate the long-term physical consequences of sleep deprivation and stress.
2) The Role of Diet and Nutrition in Sleep Quality and Stress Resilience
Diet is vital in governing sleep and stress levels. A balanced diet abundant in fruits, vegetables, whole grains, and lean proteins delivers the necessary nutrients to support brain functionality and overall health. Specific nutrients, including magnesium, omega-3 fatty acids, and vitamin D, have been found to encourage relaxation and enhance sleep quality. A healthy diet bolsters the body's capacity to manage stress, uphold healthy sleep patterns, and elevate overall wellness.
3) Reducing Screen Time and Technology Use, Especially Before Sleep
The usage of electronic devices, particularly in the time leading up to bedtime, can disrupt sleep quality and heighten stress levels. Exposure to blue light from screens (e. g. , smartphones, tablets, computers) inhibits the synthesis of melatonin, the hormone responsible for regulating sleep. Limiting screen time in the evening, especially at least one hour prior to going to bed, aids in improving melatonin production and supporting natural.
VI. FUTURE DIRECTIONS IN RESEARCH
A. Gaps in Current Literature
1) Need for More Longitudinal Studies on the Long-Term Effects of Sleep Deprivation-Induced Stress
Although a significant portion of the current research regarding sleep deprivation and stress has concentrated on short-term effects, there is an urgent necessity for additional longitudinal studies that monitor the long-term impacts of chronic sleep deprivation and stress. The predominant studies have depended on cross-sectional or experimental frameworks, which restrict our comprehension of the cumulative impacts over multiple years or decades.
2) Exploration of Individual Differences in Susceptibility to Sleep Deprivation and Stress
Not everyone faces the same level of susceptibility to stress caused by sleep deprivation. A significant gap in the literature is the investigation of individual differences that might influence susceptibility. Genetic components, such as variations in genes that manage the sleep-wake cycle or the stress response (e. g. , CLOCK gene, FKBP5), may affect how people respond to sleep deprivation and stress.
B. Advancements in Neuroimaging and Biomarker.
1) Use of Advanced Neuroimaging Techniques to Understand the Brain Mechanisms Underlying Sleep Deprivation and Stress
Recent progress in neuroimaging technologies such as functional MRI (fMRI), positron emission tomography (PET), and magnetoencephalography (MEG) presents an exciting opportunity to enhance our comprehension of the brain mechanisms associated with sleep deprivation and stress. These instruments can assist in recognizing alterations in brain activity, connectivity, and structure in areas like the prefrontal cortex, hippocampus, and amygdala—regions essential for emotional regulation, memory, and the stress response.
2) Development of Biomarkers for Early Identification of Stress-Related Disorders Linked to Sleep Deprivation
Biomarkers are essential for the early detection and prevention of stress-related conditions that stem from chronic sleep deprivation. The existing biomarkers employed to evaluate stress, such as cortisol levels and heart rate variability, possess limitations, indicating a need for more dependable and specific indicators. Investigating genetic, epigenetic, and molecular biomarkers may aid in identifying individuals at a higher risk for developing sleep deprivation-induced stress disorders.
C. Innovative Interventions
1) Exploring New Treatments Targeting Both Sleep Quality and Stress Reduction (e. g. , Digital Health Interventions, Wearable Devices)
Innovative interventions, particularly through digital health technologies and wearable devices, have the capacity to transform the management of stress resulting from sleep deprivation. Wearable devices, such as smartwatches and fitness trackers, can keep track of sleep patterns, heart rate variability, and other physiological metrics, furnishing real-time data on the effects of stress and sleep on both physical and mental well-being. These gadgets could be utilized to monitor the outcomes of interventions and provide tailored recommendations for enhancing sleep and alleviating stress, such as optimizing sleep hygiene, exercising, and practicing relaxation techniques. The incorporation of AI and machine learning into these interventions could further improve their capability to deliver individualized treatment plans based on personal reactions.
2) Investigating the Potential of Personalized Medicine in Addressing Sleep Deprivation and Stress
The future of addressing stress caused by sleep deprivation is rooted in personalized medicine. This method takes into account personal variations in genetics, physiology, and lifestyle to customize interventions for optimal effectiveness. For instance, personalized pharmaceutical therapies might be designed according to genetic and molecular profiles, allowing for more accurate targeting of the neurotransmitter systems that play a role in both sleep and stress management.
Conclusion
1) Recap of the Main Physiological, Cognitive, and Emotional Mechanisms Linking Sleep Deprivation and Stress The connection between sleep deprivation and stress is intricate, encompassing various physiological, cognitive, and emotional mechanisms. Sleep deprivation interferes with the body’s stress response system by stimulating the hypothalamic-pituitary-adrenal (HPA) axis and raising the production of stress hormones like cortisol and adrenaline. This disruption not only intensifies stress reactions but also hinders the capacity to manage emotions and navigate stress effectively. These physiological and cognitive changes lead to emotional outcomes of sleep deprivation, including greater irritability, anxiety, and an increased susceptibility to creating mood disorders such as depression. 2) Overview of the Consequences of Sleep Deprivation-Induced Stress on Physical and Mental Health Chronic sleep deprivation and its associated stress have significant long-term impacts on both physical and mental well-being. The physiological ramifications involve a heightened risk of cardiovascular conditions, metabolic issues like obesity and diabetes, and diminished immune function. Regarding mental health, ongoing sleep deprivation-induced stress is associated with the emergence of mood disorders such as anxiety, depression, and post-traumatic stress disorder (PTSD).
References
[1] Chrousos, G. P. (2009). Stress and disorders of the stress system. Nature Reviews Endocrinology, 5(7), 374-381. [2] Fernandes, C. A., Mello, M. T., & Tufik, S. (2020). Sleep and stress: An overview. Journal of Clinical Sleep Medicine, 16(5), 817-825. [3] Hirshkowitz, M., Whiton, K., Albert, S. M., et al. (2015). National Sleep Foundation\'s sleep time duration recommendations: methodology and results summary. Sleep Health, 1(1), 40-43. [4] Killgore, W. D. S. (2010). Effects of sleep deprivation on cognition. Progress in Brain Research, 185, 105-129. [5] Kuhs, A. E., Wilkins, A. R., & Banks, S. M. (2018). Stress, sleep, and mood: A review of the literature. Sleep Medicine Reviews, 42, 46-54. [6] McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87(3), 873-904. [7] Meerlo, P., Sgoifo, A., & Suchecki, D. (2008). Role of stress in the pathophysiology of sleep disorders. Progress in Brain Research, 169, 55-69. [8] Walker, M. (2017). Why We Sleep: The New Science of Sleep and Dreams. Scribner [9] Baglioni, C., et al. (2011). Insomnia as a predictor of depression and anxiety: A meta-analytic review of longitudinal studies. Journal of Affective Disorders, 135(1-3), 10-19. [10] Buckley, T. M., & Schatzberg, A. F. (2005). On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep. Journal of Clinical Endocrinology & Metabolism, 90(5), 3106-3115. [11] Burgess, H. J., et al. (2003). The effects of sleep deprivation and low sleep quality on the autonomic nervous system. Journal of Sleep Research, 12(1), 31-40. [12] Goldstein, A. N., & Walker, M. P. (2014). The role of sleep in emotional brain function. Annual Review of Clinical Psychology, 10, 679-708. [13] Irwin, M. (2015). Sleep and inflammation: Partners in sickness and in health. Nature Reviews Immunology, 15(8), 577-588. [14] Kahn, G. L., et al. (2013). The role of sleep in emotional regulation. Sleep Medicine Clinics, 8(1), 29-36. [15] Killgore, W. D. S. (2010). Sleep deprivation and cognitive performance. Progress in Brain Research, 185, 105-129. [16] Kredlow, M. A., et al. (2015). The effects of sleep deprivation on emotion regulation: A meta-analytic review. Sleep Medicine Reviews, 22, 67-87. [17] Minkel, J. D., et al. (2014). Sleep deprivation and serotonin function in humans. Journal of Neuroscience, 34(1 [18] Baglioni, C., et al. (2011). Insomnia as a predictor of depression and anxiety: A meta-analytic review of longitudinal studies. Journal of Affective Disorders, 135(1-3), 10-19. [19] Bowers, A., & Moyer, A. (2017). Effects of sleep deprivation on interpersonal relationships: A review. Journal of Sleep Research, 26(2), 238-244. [20] Dinges, D. F. (2004). The need for sleep: Implications for cognitive performance and stress. Handbook of Stress, 593-613. [21] Durmer, J. S., & Dinges, D. F. (2005). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 25(1), 117-129. [22] Harrison, Y., & Horne, J. A. (2000). The impact of sleep deprivation on decision making: A review. Journal of Experimental Psychology: Applied, 6(3), 236-249. [23] Hirshkowitz, M., et al. (2015). National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health, 1(1), 40-43. [24] Killgore, W. D. S. (2010). Effects of sleep deprivation on cognition. Progress in Brain Research, 185, 105-129. [25] Kessler, R. C., et al. (2011). The prevalence and effects of sleep problems in the workforce. Journal of Occupational and Environmental Medicine, 53(4), 383-389. [26] Killgore, W. D. S., et al. (2006). Sleep deprivation and cognitive performance. Sleep Medicine Reviews, 10(1), 29-37. [27] Minges, K. A., & Redeker, N. S. (2011). The relationship between sleep and mental health in individuals with chronic illness. Journal of Clinical Sleep Medicine, 7(3), 299-310. [28] Rosekind, M. R., et al. (2010). The impact of sleep deprivation on performance and safety in industrial settings. Industrial Health, 48(1), 56-67. [29] Tassi, P., & Muzet, A. (2000). Sleep inertia. Sleep Medicine Reviews, 4(4), 341-353. [30] Walker, M. (2017). Why We Sleep: The New Science of Sleep and Dreams. Scribner. [31] Yoo, S. S., et al. (2007). The human emotional brain without sleep – a prefrontal amygdala disconnect. Current Biology, 17(20), R877-R878. [32] Baglioni, C., et al. (2011). Insomnia as a predictor of depression and anxiety: A meta-analytic review of longitudinal studies. Journal of Affective Disorders, 135(1-3), 10-19. [33] Cappuccio, F. P., et al. (2011). Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep, 34(5), 565-574. [34] Dinges, D. F. (2004). The need for sleep: Implications for cognitive performance and stress. Handbook of Stress, 593-613. [35] Goldstein, A. N., & Walker, M. P. (2014). The role of sleep in emotional brain function. Annual Review of Clinical Psychology, 10, 679-708. [36] Irwin, M. (2015). Sleep and inflammation: Partners in sickness and in health. Nature Reviews Immunology, 15(8), 577-588. [37] Kessler, R. C., et al. (2011). The prevalence and effects of sleep problems in the workforce. Journal of Occupational and Environmental Medicine, 53(4), 383-389. [38] McEwen, B. S. (2007). Physiology and neurobiology of stress and adaptation: Central role of the brain. Physiological Reviews, 87(3), 873-904. [39] Muller, C. P., et al. (2016). Sleep, stress, and inflammation: The role of cytokines in sleep disturbance. Psychoneuroendocrinology, 63, 33-42. [40] Roth, T., et al. (2006). Sleep and post-traumatic stress disorder. Sleep Medicine Reviews, 10(4), 237-244. [41] Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: A meta-analytic study of 30 years of research. Psychological Bulletin, 130(4), 601-630. [42] Stranges, S., et al. (2008). Sleep duration and risk of hypertension in women: The effects of short and long sleep. Hypertension, 51(4), 1095-1101. [43] Taheri, S., et al. (2004). Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Medicine, 1(3), e62. [44] Tasali, E., et al. (2008). Sleep restriction and insulin sensitivity: The role of the autonomic nervous system. Sleep, 31(9), 1061-1068. [45] Van Cauter, E., et al. (1996). Sleep and the regulation of stress hormones. Endocrine Reviews, 17(6), 724-738. [46] Van der Helm, E., et al. (2011). Sleep and emotional memory processing. Sleep Medicine Reviews, 15(3), [47] Bandelow, B., et al. (2015). The Efficacy of Antidepressants and Anxiolytics in the Treatment of Anxiety and Depression. European Neuropsychopharmacology, 25(5), 736-746. [48] Edinger, J. D., & Means, M. K. (2005). Cognitive behavioral therapy for primary insomnia. Clinical Psychology Review, 25(5), 539-558. [49] Hoffman, B. M., et al. (2008). The effects of exercise on anxiety and depression. Psychiatric Clinics of North America, 31(2), 329-343. [50] Hirshkowitz, M., et al. (2015). National Sleep Foundation\'s sleep time duration recommendations: Methodology and results summary. Sleep Health, 1(1), 40-43. [51] Kabat-Zinn, J. (1990). Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Delacorte Press. [52] Kales, A., et al. (1984). Benzodiazepines and the sleep cycle. Archives of General Psychiatry, 41(2), 170-173. [53] Kubera, M., et al. (2012). Exercise and the regulation of sleep. Journal of Psychiatric Research, 46(11), 1516-1525. [54] Lader, M. (2011). Benzodiazepine harm: How the treatment of anxiety and insomnia causes harm. World Psychiatry, 10(3), 172-176. [55] Morin, C. M., et al. (2006). Cognitive behavioral therapy for insomnia: A review of the evidence. Journal of Clinical Psychology, 62(4), 453-467. [56] Roth, T., [57] Alaedini, F., et al. (2020). Wearable technologies in stress and sleep monitoring: Current developments and future prospects. Journal of Sleep Research, 29(6), e13024. [58] Alvaro, P. K., et al. (2013). Genetic influences on the interaction between sleep and stress: A systematic review. Sleep Medicine Reviews, 17(1), 5-14. [59] Finkelmeyer, A., et al. (2020). Digital interventions for stress management: A systematic review of mobile apps. BMC Psychology, 8(1), 12. [60] Fox, K. C. R., et al. (2018). Brain activity during mindfulness meditation and its effect on emotional regulation. Frontiers in Psychology, 9, 1770. [61] Gustin, L. A., et al. (2020). Individual differences in vulnerability to stress and sleep disturbances: Implications for research and treatment. Sleep Health, 6(3), 295-300. [62] Klein, L. A., et al. (2020). Biomarkers of stress-related disorders: Identifying new avenues for research and intervention. Biological Psychology, 158, 107977. [63] Killgore, W. D. S., et al. (2008). Sleep deprivation and emotional regulation: A functional MRI study. Journal of Sleep Research, 17(3), 354-362. [64] Leproult, R., & Van Cauter, E. (2010). Role of sleep and sleep loss in hormone release and metabolism. Current Opinion in Endocrinology, Diabetes, and Obesity, 17(6), 451-457.
Copyright
Copyright © 2025 Anchal Patel, Shajeel Ahmad, Anjali Singh, Vineeta Kumari, Km.Dolly Chaudhary, Shwet Kumar, Dr. Sachin Neekhra, Dr. Alok Kumar Shukla. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET66503
Publish Date : 2025-01-12
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

