Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Cycloserine-Induced Psychosis in Multidrug-Resistant Tuberculosis (MDR-TB) in Young Male Patient: A Case Report
Authors: Damini Kharb, Shagufta Jawaid , Krishan Kant Kushwaha
DOI Link: https://doi.org/10.22214/ijraset.2024.66083
Certificate: View Certificate
Abstract
The genre of tuberculosis (TB) dubbed multidrug-resistant tuberculosis (MDR-TB) is resistant to at least two of the most potent first-line anti-TB medications, isoniazid (H) and rifampicin (R). Cycloserine is placed by the World Health Organization as a group four second line anti-tubercular medication for the treatment of MDR-TB. Psychosis, depression, and neuropathy have been linked to neuropsychiatric toxicity, which is caused by cycloserine or its structural equivalent terizidone. After receiving an MDR-TB diagnosis, a 32-year-old male patient received customized treatment regimens including bedaquiline, linezolid, levofloxacin, and Cs. The patient experienced psychosis with agitated behaviour, excessive talking, yelling episodes, fearfulness, photophobia, drowsiness, paranoid thoughts, and headaches multiple times after taking anti-TB medications for 54 days. He was prescribed clonazepam, olanzapine, and lorazepam. Over time, the patient recovered progressively. When giving cycloserine, extreme caution should be used along with frequent and close monitoring, as mental adverse medication reactions may increase the risk of poor drug adherence in patients with drug-resistant tuberculosis.
Introduction
I. INTRODUCTION
Mycobacterium tuberculosis is the causative agent of tuberculosis, which is mainly spread by airborne droplets from an infected individual (1). Although extra pulmonary tuberculosis can also damage the spine and brain, tuberculosis primarily affects the lung (2). The cornerstone of tuberculosis treatment is ant tuberculosis medication, specifically isoniazid, rifampicin, ethambutol, and pyrazinamide as first-line therapies (3). Anti-TB medication side effects can be broken down into two different kinds: severe and mild (4). TB that is resistant to at least isoniazid (H) and rifampicin (R), the two most potent medications, is known as multidrug-resistant tuberculosis (MDR-TB) (5). The outcomes of a sensitivity test, which attempts to figure out if Mycobacterium tuberculosis (M. tb) has or has not been resistant to anti-TB medications, are used to confirm the diagnosis of multidrug-resistant tuberculosis (MDR-TB). The course of MDR-TB treatment consists of 18 to 24 months of minimum medication use (6).
For extended multidrug-resistant tuberculosis (MDR-TB) treatment regimens, the World Health Organization (WHO) listed terizidone or cycloserine as a group B medication (WHO, 2019) (7). The compound known as cycloserine, or D-4-amino-3-isoxazolidinone, first emerged and fabricated by Hidy et al. (8)(Hidy et al., 1955). Treatment of tuberculosis-resistant patients: Evidence-based guidelines and international medical societies have considered several treatment alternatives (9), such as the use of robustly effective extended-spectrum antibiotics such cycloserine (10). By competitively inhibiting two crucial enzymes involved in the formation of Mycobacterium tuberculosis's cell wall, CS demonstrates its antibiotic properties (11). But because cycloserine (CS) may cross the blood–brain barrier, inhibit GABA-transferase, and interact with N-methyl-d-aspartate (NMDA) receptors in the central nervous system, it also appears to be correlated with the onset of psychotic symptoms (12).
Cycloserine, or its structural analogue terizidone, has been associated with neuropsychiatric toxicity (psychosis, depression, and neuropathy) (13). Studies reporting the effect of cycloserine concentrations on both microbial kill and resistance suppression have recently been published, including penetration of the drug into TB cavities and resistance arising therein (14, 15)(Deshpande et al., 2018; Dheda et al.,2018). This case report is noteworthy because it illustrates the psychological adverse effects from various anti tuberculosis medications.
II. CASE PRESENTATION
A 32-year-old male patient presented to Pulmonary medicine ward with chief complaints of acute fever for 1 week, patient experienced productive non-blood-stained cough but not able to expectorate for 4 days, vertigo, Psychosis with the symptoms of agitated behaviour, overtalktiveness, shouting spells, fearfulness, photophobia, drowsiness, paranoid ideas and headache.
Patient also experienced shortness of breath for 4 days was admitted in MDR department. Past medical history of patient was diagnosed to have multidrug resistance tuberculosis (MDR-TB), patient resistance too both rifampicin and Isoniazid.
Patient was advised for CX-R, ABG, ECG, CBC, LFT, KFT, PT/INR, D-dimer. Urine analysis R/E Followed by serum sodium, potassium and magnesium levels. Patient was primarily stabilized with antipsychotics, antidepressants and benzodiazepines for psychosis. His blood test at presentation illustrated as:
Table1: Complete blood count and comprehensive metabolic panel.
|
Complete blood count |
Comprehensive metabolic panel |
|||
|
Haemoglobin: 13gm/dl (13-17) |
Sodium: 136mmol/L (137-145) |
|||
|
Platelets: 259000/uL (150000-400000) |
Potassium: 3.9mmol/L (3.5-5.1) |
|||
|
Differential leucocyte count (DLC)
|
Magnesium: 2.0 mmol/L (1.6-2.3) |
|||
|
PCV: 37.7% (40-50) |
Serum Bilirubin direct: 0.5mg/dl (0-0) |
|||
|
|
Serum globulin: 3.70gm/dl (2.30-3.59) |
|||
|
|
Serum Creatinine: 0.5mg/dl (0.8-1.5) |
|||
|
|
Serum Uric acid: 3.2mg/dl (3.5-8.5) |
Anti HCV, HBsAg test was negative, prothrombin time, and international normalized ratio and urine examination(R/E) were normal.
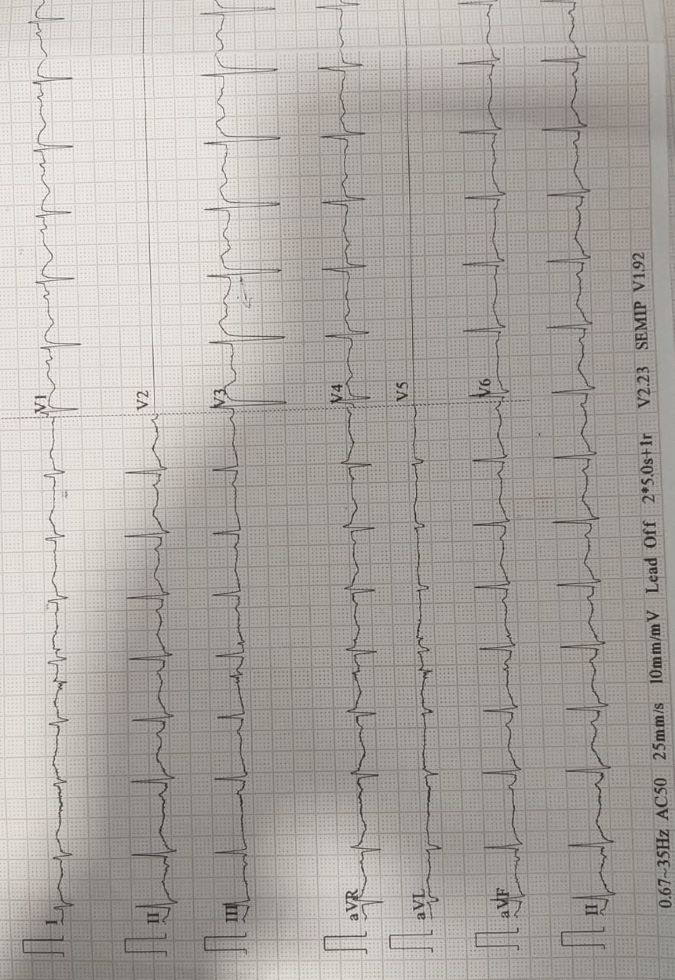
Figure 1: - ECG illustrates prolonged QT Intervals.
Table 2: - Patient Arterial Blood Gas analysis
|
Components |
11/09/2024 |
12/09/2024 |
Normal Range |
|
pH |
7.40 |
7.40 |
7.35-7.45 |
|
PCo2 |
33 |
31 |
35-45 mmHg |
|
PO2 |
88 |
100 |
60-100 mmHg |
|
HCO3- |
20.4 |
20.1 |
22-26 mmol/L |
|
Hct |
41 |
53 |
40-54% |
|
SO2c |
97 |
98 |
95-100% |
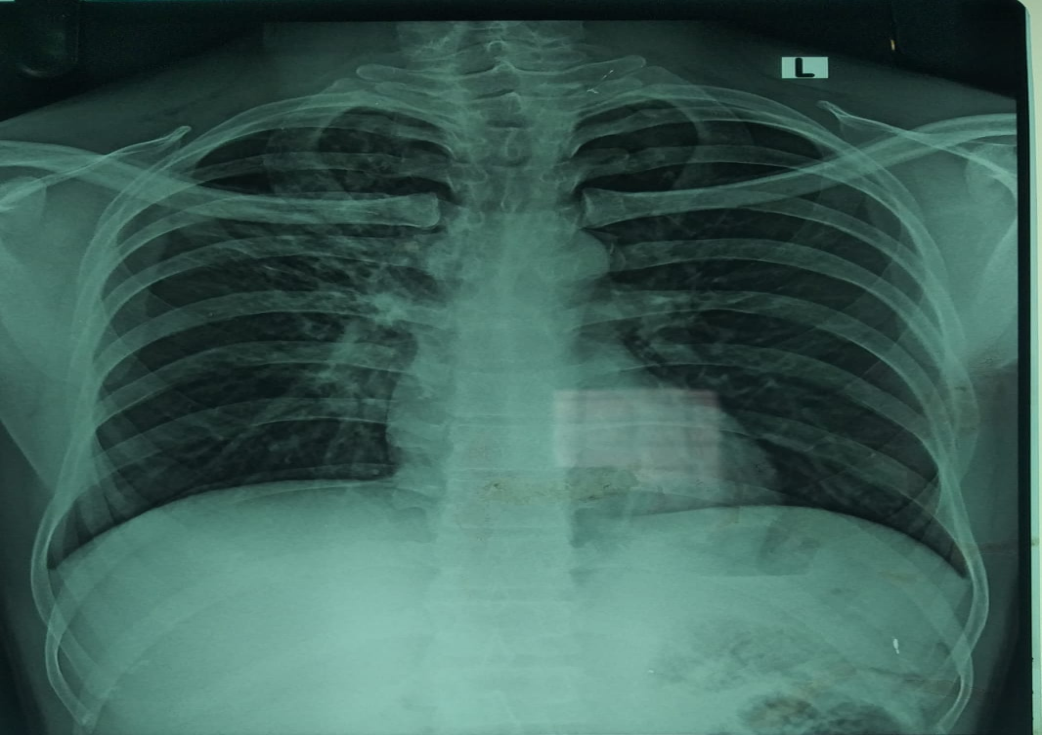
Figure 2: - Chest X-ray of patient (Bilateral prominent markings with hyper inflated lungs)
Patient was treated with suitable medications as mentioned below. The care taker were counselled about the MDR-TB therapy side effects, patient diet and patients was discharge.
Table 3: Medication Treatment Chart
|
Medication |
Dose |
Route |
Frequency |
|
Tab. VMS MAX |
1 tab. |
Oral |
OD |
|
Tab. BEDAQUILLINE |
2x100 MG |
Oral |
On alternate days |
|
Tab. CYCLOSERINE |
3x250 MG |
Oral |
OD |
|
Tab. LINEZOLID |
600 MG |
Oral |
OD |
|
Tab. LCIN |
750 MG |
Oral |
OD |
|
Tab. DELAMANID |
2x500 MG |
Oral |
BD |
|
Tab. PYRIDOXINE |
100 MG |
Oral |
HS |
|
Tab. ACILOC |
300 MG |
Oral |
OD |
|
Ensure protein |
2 TSF |
Oral |
TDS with half glass of water |
|
Tab. OLIMELT |
5 MG |
Oral |
BD |
|
Inj. LOPEZ |
2 MG |
IM |
SOS |
|
Tab. CLONOTRIL |
0.25 MG |
Oral |
BD |
Conclusion
MDR-TB management might occasionally be challenging. While therapy for MDR-TB with an individual regimen requires at least five medications and lasts 18 to 24 months, treatment for sensitive TB only requires four drugs and takes six to nine months. Many medications have serious negative effects when used. Streptococcus orchidaceous produces the broad-spectrum antibiotic cyclorine. In 1995, it was initially extracted from a fermentation brew and then synthesised. Currently, when main medicines fail to cure pulmonary or extra pulmonary TB, cycloserine is used in combination with other tuberclostatic medications. The patient was started on cycloserine due to resistance. Although our patient was on multiple potentially psychotic ant tubercular medications, he had no family or personal history of mental health issues. When antipsychotic medications were stopped and CS was stopped, the majority of documented individuals showed improvement in their ability to treat CS-induced psychosis. This feature varies based on accounts in the literature because a retrospective study demonstrates that most patients\' psychosis improves when the dosage of CS is decreased or temporarily stopped. Nonetheless, the findings of both trials concur that lowering CS exposure and giving antipsychotics lessens the likelihood that CS-induced psychotic symptoms will manifest. Initially, 250mg 12hrly for the first 2 weeks, followed by 500-1000mg daily in equally divided doses. Adjust dose based on blood concentration and response. Max. 1000mg daily. There were some contraindication with CS: Hypersensitivity, Epilepsy, mental depression, severe anxiety, psychosis, alcohol abuse or alcoholism and some sever renal impairment. There was some special precaution taken with CS, patient with porphyria, history of chronic alcoholism, potential vit. B12 or folate deficiency. Patient receiving >500mg daily dose have mild to moderate renal impairment. Monitoring parameters initial to CS therapy: perform culture and susceptibility tests, renal, hepatic and haematological functions periodically. Evaluate neuropsychiatric status every month or more frequently if symptoms occur (Disorientated with loss of memory, paraesthesia, dizziness, coma, personality changes, hyperirritability, aggression).
References
[1] Swalehe H, Obeagu E. Tuberculosis: Current Diagnosis and Management. Elite Journal of Public Health. 2024;2(1):23-33. [2] Mandal S, Biswas P, Ansar W, Mukherjee P, Jawed JJ. Tuberculosis of the central nervous system: Pathogenicity and molecular mechanism. A Review on Diverse Neurological Disorders: Elsevier; 2024. p. 93-102. [3] Jones NT, Abadie R, Keller CL, Jones K, Ledet III LF, Fox JE, et al. Treatment and Toxicity Considerations in Tuberculosis: A Narrative Review. Cureus. 2024;16(6). [4] Mishra AK. Clinical Implications of Adverse Reactions to Anti-Tubercular Drugs in Tuberculous Meningitis: A Literature Review. International Journal. 2024;7(4):342. [5] Maya T, Wilfred A, Lubinza C, Mfaume S, Mafie M, Mtunga D, et al. Diagnostic accuracy of the Xpert® MTB/XDR assay for detection of Isoniazid and second-line antituberculosis drugs resistance at central TB reference laboratory in Tanzania. BMC Infectious Diseases. 2024;24(1):672. [6] Achalu DL, Kiltu AB, Teferi M, Mohammed FG, Workneh BD, Beyene KA, et al. Treatment outcomes of standardized injectable shorter regimen for multi-drugs resistant tuberculosis in Ethiopia: a retrospective cohort study. BMC Infectious Diseases. 2024;24(1):1-9. [7] Haroon OM. CLASSIFYING NEW ANTI-TUBERCULOSIS DRUGS AND MANAGEMENT OF ITS ADR AS PER WHO: A SHORT REVIEW. World Journal of Pharmaceutical Sciences. 2024. [8] Johnson PD. Cycloserine and Terizidone. Kucers\' The Use of Antibiotics: CRC Press; 2017. p. 2520-30. [9] Al-Worafi YM. Handbook of Complementary, Alternative, and Integrative Medicine: Education, Practice, and Research Volume 3: Research Evidence Based Clinical Practice: CRC Press; 2024. [10] Mushtaq A, Buensalido JAL, DeMarco CE, Sohail R, Lerner SA. Mechanisms of action of Antibacterial agents. Practical Handbook of Microbiology: CRC Press; 2021. p. 747-76. [11] Chauhan M, Barot R, Yadav R, Joshi K, Mirza S, Chikhale R, et al. The Mycobacterium tuberculosis Cell Wall: An Alluring Drug Target for Developing Newer Anti?TB Drugs—A Perspective. Chemical Biology & Drug Design. 2024;104(3):e14612. [12] Kuo H-Y, Liu F-C. Molecular pathology and pharmacological treatment of autism spectrum disorder-like phenotypes using rodent models. Frontiers in cellular neuroscience. 2018;12:422. [13] Court R, Centner CM, Chirehwa M, Wiesner L, Denti P, de Vries N, et al. Neuropsychiatric toxicity and cycloserine concentrations during treatment for multidrug-resistant tuberculosis. International Journal of Infectious Diseases. 2021;105:688-94. [14] McMaster EC. Ferrocene-sulfonamide derivatives as antimycobacterials. 2024. [15] Morton AJ, Roddy Mitchell A, Melville RE, Hui L, Tong SY, Dunstan SJ, et al. Mycobacterium tuberculosis infection in pregnancy: a systematic review. medRxiv. 2024:2024.08. 10.24311783.
Copyright
Copyright © 2024 Damini Kharb, Shagufta Jawaid , Krishan Kant Kushwaha . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET66083
Publish Date : 2024-12-23
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

