Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- References
- Copyright
Evaluating the Anti-Cancer Effects of Thymoquinone in Treating Colorectal Cancer In Vitro
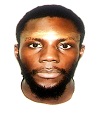
Authors: Beshikwashi Peter Ugbe, Roopika Chandran
DOI Link: https://doi.org/10.22214/ijraset.2023.56786
Certificate: View Certificate
Abstract
Colorectal cancer (CRC) remains a significant health concern worldwide. The toxicities associated with the current treatment modalities for CRC and the growing emergence of chemotherapeutic resistance underscores the need for the discovery of novel anti-cancer agents that offer benefits in tackling these issues. Thymoquinone (TQ), a compound derived from Nigella sativa, has shown promising anticancer effects. This study aimed to investigate the anticancer properties of TQ against colorectal cancer (HCT-116) cells in vitro. The anti-cancer potential of TQ was evaluated using immunocytochemistry, cell cycle analysis, and Annexin V/PI apoptotic assay after 48 hours of treatment with TQ, 5-fluorouracil (5-FU) (positive control), and TQ + 5-FU. The results indicated a substantial reduction in (Epidermal growth factor receptor) EGFR expression post-TQ treatment (P ? 0.001). Similarly, increased expression of the apoptotic marker Caspase-3 was observed in cells treated with TQ (P ? 0.001), 5-FU (P ? 0.001), and their combination (P ? 0.001). Cell cycle analysis showed increased pre-G1 cell events in 5-FU (7.4%, P ? 0.05) and 5-FU + TQ (6.6%, P ? 0.05) with a slight elevation seen with TQ (1.7 %, P ?0.05). Annexin V/PI apoptosis analysis further indicated that TQ-induced early apoptosis (9.15%) and late apoptosis (48.2%) and 5-FU + TQ had 14.5% and 24.8% respectively. In conclusion, Thymoquinone shows anticancer effects against colorectal cancer cells (HCT-116), decreasing EGFR expression and inducing apoptosis as evidenced by pre-G1 cell accumulation and elevated caspase-3 expression. While combined TQ and 5-FU treatment showed certain effects, it did not appear to enhance the anti-cancer activity of TQ or 5-FU, warranting further exploration.
Introduction
I. INTRODUCTION
A. Background
Colorectal cancer (CRC) is the third most common cause of cancer-related death worldwide with an estimated 1.93 million new cases and 830,000 deaths annually. Its global incidence in both genders is projected to increase to 3.2 million by the year 2040[1]. With its high incidence rates and significant mortality burden, CRC poses substantial challenges to healthcare systems worldwide. The most well-established risk factors are male sex, increasing age, and a hereditary predisposition, but associations have been made with modifiable factors such as Western diet, smoking, excessive alcohol, and obesity[2]. These alarming figures underscore the urgency and importance of comprehensive investigations into the aetiology, pathogenesis, and therapeutic strategies for CRC. Significant advancements in diagnostic and therapeutic measures have been developed for the treatment of CRC with the development of targeted therapies for metastatic disease. Despite this progress, the prognosis for patients with advanced stages of CRC remains poor.[3]
Current treatment modalities for CRC include surgical resection, chemotherapy, radiation therapy, and targeted therapies. While these approaches have shown some success, they are not without limitations. Surgical resection may be limited by inoperable tumours, surgical risks, and functional complications[4]. Chemotherapy is associated with toxicity, drug resistance, and limited response rates. Radiation therapy has limitations in tumour specificity, radioresistance, and side effects [5]. Targeted therapies have shown promise, but face challenges related to tumour heterogeneity and the development of resistance.
One of the primary treatments for advanced or metastatic disease involves utilizing chemotherapeutic agents such as 5-fluorouracil(5-FU), capecitabine, and Oxaliplatin. While these agents remain in usage because of their well-established efficacies and accessibility, their compliance is still marred with problems related to their toxicity and the emergence of drug resistance [6].Thus, there is a growing need for novel therapies for CRC treatment that are effective, have low toxicity profiles, and can help combat the growing drug resistance seen with traditional therapeutic agents.
In light of these challenges, researchers have turned their attention to investigating novel therapeutic approaches and an intriguing avenue of research involves the exploration of natural compounds with potential anti-cancer properties. One such compound of interest is thymoquinone (TQ), a bioactive constituent extracted from Nigella sativa, commonly known as black seed or black cumin. TQ has garnered considerable attention due to its diverse pharmacological activities, including anti-inflammatory, antioxidant, and anti-cancer effects.[7] .
While research on TQ's potential anti-cancer properties has been conducted in various cancer types, the investigation of its efficacy specifically in CRC remains relatively limited. Nonetheless, promising findings have emerged from in vitro studies, highlighting TQ's ability to inhibit cancer cell proliferation, induce apoptosis, and suppress tumour growth in CRC models[8, 9].These preliminary studies underscore the need for further research to elucidate the underlying mechanisms and evaluate the therapeutic potential of TQ in CRC treatment.
Previous studies have shown that TQ inhibits the growth of various cancer cell lines, including CRC cells when used singly or as complementary therapy to other chemotherapeutic agents[9, 10]. It has been proposed that TQ exerts its anti-carcinogenic effect by multi-level and multi-pathway involvement primarily in those associated with cell cycle arrest and apoptosis. Multiple studies have indicated that TQ can modulate Epidermal growth factor receptor (EGFR) signalling and caspase-3 activation in various cancer types. TQ has been shown to inhibit EGFR activation, leading to the suppression of downstream signalling pathways involved in cell proliferation and survival[11]. Additionally, TQ has been found to promote caspase-3 activation, which is a key mediator of apoptosis, leading to programmed cell death[12]. However, the specific effects of TQ on EGFR and caspase-3 in CRC cells remain to be fully elucidated.
Understanding the impact of TQ on EGFR and caspase 3 in CRC is of significant importance for several reasons. Firstly, the inhibition of EGFR signalling by TQ may provide a targeted approach to disrupt the growth and survival of CRC cells, potentially overcoming resistance to conventional therapies [13]. Secondly, the activation of caspase-3 by TQ may induce apoptotic cell death, offering a promising avenue for suppressing tumour growth and improving treatment outcomes[14]. By investigating the effects of TQ on these molecular targets, this study aims to contribute to the knowledge base surrounding TQ's potential as an alternative treatment option for CRC, offering insights into its mechanisms of action and therapeutic applications.
B. Global Burden of Colorectal Cancer
The global burden of CRC is significant, with millions of new cases and deaths reported annually. According to recent estimates, there were approximately 1.9 million new CRC cases and 935,000 deaths in 2020[1]. This disease places a significant strain on healthcare systems, economies, and individuals. The economic burden of CRC is considerable, encompassing direct healthcare costs, indirect costs related to productivity loss, and the social impact on patients and their families. A report from the United States estimates that about 12.6% of the total cancer related costs of the healthcare system can be attributed to colorectal cancer[15].There are notable variations observed in the incidence and prevalence of CRC across different regions. In developed countries, CRC incidence rates tend to be higher, while developing countries are experiencing an increasing burden due to instance, studies have reported rising CRC incidence rates in countries like China and India, highlighting the emerging epidemic[16, 17]. Multiple factors contribute to CRC development, including age, family history, lifestyle choices, diet, and genetic predisposition. Lifestyle changes, such as the adoption of Westernized diets and sedentary behaviors, have been associated with an increased risk of CRC[18]. To address the growing burden of CRC, understanding its epidemiology is crucial.
C. Pathogenesis and Disease Progression.
Colorectal cancer (CRC) is a complex and multifactorial disease, and understanding its pathogenesis is crucial for developing effective treatment strategies. It typically arises from a series of genetic and epigenetic alterations that induce malignant transformational changes in normal colonic epithelial cells. The initiation and progression of CRC often involve genetic mutations that disrupt critical cellular pathways. The adenomatous polyposis coli (APC) gene, a tumour suppressor, plays a pivotal role in CRC development[19]. Mutations in APC lead to the dysregulation of the Wnt signalling pathway, promoting uncontrolled cell proliferation and the formation of adenomatous polyps[20].The Kirsten rat sarcoma viral oncogene homolog (KRAS) is another key player in CRC pathogenesis. Mutations in KRAS result in constitutive activation of downstream signalling pathways, leading to enhanced cell survival and proliferation[21]. Epigenetic alterations, such as DNA methylation and histone modifications, also contribute significantly to CRC pathogenesis. Promoter hypermethylation of tumour suppressor genes(Figure 1), such as MLH1 and CDKN2A, can silence their expression, promoting genomic instability and tumorigenesis[22]. Chronic inflammation is another hallmark of CRC pathogenesis.
Inflammatory bowel diseases, such as Crohn's disease and ulcerative colitis, increase the risk of CRC due to persistent inflammation of the colonic mucosa[23]. Inflammatory mediators, including tumour necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), create a microenvironment conducive to tumour growth and progression[24]. Environmental factors, particularly diet and lifestyle, also play a role in CRC pathogenesis. A high intake of red and processed meats, low fibre consumption, and sedentary behaviour are associated with an increased risk of CRC[25].These factors can influence the gut microbiota, leading to chronic inflammation and the production of pro-carcinogenic metabolites[26]. Understanding the intricate pathogenesis of CRC is pivotal for developing targeted therapies and preventive measures.

D. Current Treatment Options for Colorectal Cancer
- Surgery
Surgery remains the mainstay of treatment for colorectal cancer (CRC), aiming to achieve complete tumour resection and regional lymph node removal[4]. Various surgical procedures, such as colectomy, proctectomy, and the creation of ostomies, are employed depending on the tumor location and stage. The main goals of CRC surgical treatment include preventing recurrence and metastasis, addressing complications, and maintaining quality of life[28]. Traditional open surgery has been the gold standard, but advancements in minimally invasive techniques, including laparoscopic and robotic-assisted surgery, have gained popularity due to their benefits, such as reduced blood loss, shorter hospital stays, and faster recovery[4]. However, these surgical options have a limited role to play in advanced CRC warranting the need for further research into non-surgical therapeutic measures to improve morbidity and mortality rates in this sub-group of patients.
2. Chemotherapy
Chemotherapy plays a pivotal role in both adjuvant and palliative settings for CRC treatment. The combination of fluorouracil (5-FU) and leucovorin has been a standard adjuvant chemotherapy regimen for CRC, significantly improving survival outcomes[29]. Oxaliplatin and irinotecan, in combination with 5-FU or its oral prodrug capecitabine, have demonstrated efficacy in metastatic CRC[30]. Advancements in molecular techniques have led to the identification of specific molecular alterations, such as mutations in the KRAS or BRAF genes, which have heralded the development of targeted therapies in CRC[21]. Anti-EGFR monoclonal antibodies, including cetuximab and panitumumab, have shown efficacy in KRAS wild-type metastatic CRC[31]. Additionally, anti-angiogenic agents, such as bevacizumab and aflibercept, have been approved for use in combination with chemotherapy in advanced CRC[32].
3. Radiotherapy
Radiotherapy plays a significant role in the management of locally advanced rectal cancer, aiming to reduce tumour size and improve surgical outcomes. Both external beam radiation therapy (EBRT) and brachytherapy can be employed, either as part of neoadjuvant therapy or as adjuvant treatment following surgery[33]. EBRT techniques, such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT), offer precise dose delivery and minimize radiation exposure to healthy tissues[34] .
However, it is not without its limitations. The proximity of the colon and rectum to critical structures, such as the bladder and small intestine, poses challenges in achieving an optimal balance between delivering effective radiation doses and minimizing damage to healthy tissues[5] . Additionally, inherent tumour resistance to radiation further hampers the therapeutic efficacy of radiotherapy in CRC[35].
E. Introduction to Thymoquinone and its Sources
Nigella sativa, commonly known as black seed or black cumin, has a rich history of traditional medicinal use spanning several centuries. The seeds of this plant contain. constituents responsible for its pharmacological effects. Notably, TQ possesses a distinctive chemical structure characterized by a benzene ring with a quinone moiety, which contributes to its diverse biological activities[36]. The use of Nigella sativa seeds and its derivatives in traditional medicine has provided a strong foundation for exploring their therapeutic potential. TQ has demonstrated intriguing pharmacological properties, including anti-inflammatory, antioxidant, antimicrobial, and immunomodulatory effects[9, 10].
F. Chemical properties and bioavailability of TQ
TQ has a relatively low molecular weight, making it easily soluble in organic solvents such as ethanol, methanol, and dimethyl sulfoxide (DMSO). This solubility profile has facilitated its use in various in vitro studies[37].Studies have suggested that TQ’s moderate to low bioavailability is due to factors such as poor aqueous solubility, rapid metabolism, and limited gastrointestinal absorption[38]. Strategies to enhance the bioavailability of TQ have been explored, including the development of novel formulations, such as nanostructured lipid carriers or encapsulation in liposomes, to improve its stability and absorption[39].
G. Pharmacological properties and potential therapeutic applications of TQ
TQ has been shown to exert anti-inflammatory effects by modulating various inflammatory pathways, including the nuclear factor-kappa B (NF-κB) signalling pathway.[39]. Its antioxidant properties involve scavenging free radicals and enhancing the antioxidant defence system in cells, which may contribute to its protective effects against oxidative stress-related damage[40].
In addition to its anti-inflammatory and antioxidant effects, TQ has demonstrated promising anticancer potential. Several studies have reported its ability to inhibit cell proliferation, induce apoptosis, and suppress tumour growth in various cancer types, including colorectal cancer[8].TQ's anticancer properties are thought to be mediated through multiple mechanisms, such as targeting signalling pathways involved in cell survival and apoptosis, including the epidermal growth factor receptor (EGFR) pathway[12].Furthermore, TQ has shown synergistic effects with conventional chemotherapy agents, enhancing their anticancer efficacy while reducing their toxicity[9].
H. Molecular mechanisms of action of TQ in cancer cells
TQ has been shown to inhibit the activation of nuclear factor-kappa B (NF-κB), a transcription factor involved in the regulation of inflammation, cell survival, and proliferation[41]. By suppressing NF-κB activation, TQ can interfere with the expression of genes associated with tumour growth and survival, thereby inhibiting cancer cell proliferation and promoting apoptosis. TQ has also been found to induce apoptosis.
It can upregulate pro-apoptotic factors such as Bax and downregulate anti-apoptotic factors like Bcl-2, thereby shifting the balance towards apoptosis[42]. TQ has also been shown to activate caspases, a family of proteases involved in the execution of apoptotic cell death. Specifically, TQ has been found to activate caspase 3, a key effector caspase responsible for the cleavage of various cellular substrates during apoptosis[43].

I. In Vitro Studies on Thymoquinone in Colorectal Cancer
A growing number of in vitro studies have investigated the effects of thymoquinone (TQ) in colorectal cancer (CRC) cell lines, providing valuable insights into its potential as a therapeutic agent. These studies have explored various aspects of TQ's anti-cancer effects, including its impact on cell viability, proliferation and intracellular signalling. For instance, it has been found that TQ treatment significantly reduced cell viability and inhibited cell proliferation in HCT116 and SW480 CRC cell lines[44]. Similarly inhibited cell growth and induced cell cycle arrest in HCT116 CRC cell lines[45].
TQ has also been shown to induce apoptosis in CRC cell lines. Studies by [46]. demonstrated that by inhibiting the JAK2- and Src-mediated phosphorylation of EGFR tyrosine kinase, thymoquinone (TQ) effectively blocked STAT3 signalling and induced apoptosis in HCT116 cells. These findings highlight the ability of TQ to induce programmed cell death in CRC cells, offering a potential therapeutic avenue for combating CRC[45].
J. Rationale and Hypothesis
Given the promising anti-cancer effects of Thymoquinone in treating colorectal cancer there is a need to further investigate the mechanism of action and potential therapeutic benefits of this natural compound. As the global incidence of colorectal cancer (CRC) is anticipated to rise, combating drug resistance has become a pressing challenge that necessitates the development of effective, cost-efficient, and safe treatments. The study hypothesizes that Thymoquinone (TQ) will exhibit anti-cancer properties in colorectal cancer cells through the modulation of EGFR expression, activation of caspase-3, and the induction of apoptosis and cell cycle arrest.
K. General aim
To investigate the potential anticancer effects of thymoquinone in colorectal cancer using an in vitro approach.
L. Objectives
- To investigate the effect of thymoquinone on apoptosis in colorectal cancer cells.
- To assess the impact of TQ treatment on cell cycle arrest and distribution in different phases of the cell cycle.
- To assess the effect of thymoquinone on the expression of EGFR and Caspase-3 in colorectal cancer cells.
- To evaluate the potential synergistic anti-cancer effects of TQ in combination with 5-FU in colorectal cancer cells.
II. MATERIALS AND METHODS
A. Materials
The cell line HCT116(ATCC CCL-247) was procured from the American Type Culture Collection (ATCC) and was grown and maintained in Dulbecco's Modified Eagle Medium (DMEM). The DMEM media, FxCycle PI/RNase Staining Solution (Cell Cycle Kit), and eBioscience Annexin V-FITC Apop Kit (Apoptosis Kit) were acquired from Thermo Fisher Scientific (USA). Purified Thymoquinone (Figure 3) and 5 Fluorouracil (5-FU) were obtained from Sigma-Aldrich (USA). Proteintech supplied the EGFR and Caspase-3 antibodies, and Vector laboratories provided the Vectastain Elite ABC Universal kit. Trypan Blue was purchased from HyClone®, South Logan, UT. All chemicals were handled and used in accordance with the manufacturer's instructions and appropriate safety measures. All remaining chemicals used in the study were of the highest available purity grade for analytical purposes and sourced from reputable suppliers.

B. Cell culture
Cells were maintained in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% foetal bovine serum (FBS) and 1% penicillin-streptomycin antibiotic in a humidified incubator at 37°C and 5% CO?. The culture medium was replenished at regular intervals of 48-72 hours using a cell pelleting technique achieved through centrifugation. Prior to experimental treatments, cells were seeded in appropriate culture dishes, and allowed to adhere and grow to approximately 80-90% confluence. Prior to use, the complete cell culture medium and serum-free medium were warmed in a water bath. The cell culture medium was removed, and cells were washed twice with phosphate-buffered saline (PBS) or serum-free media to eliminate serum traces that could interfere with trypsin activity. Subsequently, 5 ml of trypsin was added to detach the cells, and the flask was returned to the incubator for 2 to 5 minutes. Microscopic examination confirmed cell detachment, with gentle tapping applied if some cells remained attached. Following this, 5 ml of complete medium was added to wash the flask walls and deactivate the trypsin. The cell suspension was transferred to a centrifuge tube, centrifuged, and the supernatant discarded. Trypan blue dye assay was used to check for cell density and count using the cell counter, where live cell concentration was recorded for subsequent calculations.
C. Drug and Treatment Concentrations
For the experiments, cells were divided into five distinct treatment groups: control (untreated) group, vehicle control (DMSO) group, Thymoquinone (TQ) group, 5-Fluorouracil(5-FU) group, and a combination of TQ and 5-FU. The utilized concentrations of TQ and 5-FU were 25 μM and 20 μM, respectively. These concentrations were predicated upon prior in vitro investigations which ascertained their non-toxicity to mammalian cells, whilst preserving significant efficacy[47].
D. Immunocytochemistry
Cells were seeded at a density of 7x10^4/ml onto sterilized coverslips and placed in 6-well plates, allowing them to adhere overnight. The adhered cells were then treated with TQ and 5-FU for a duration of 48 hours.
Post-treatment, cells were washed with phosphate-buffered saline (PBS) and fixed in 4% paraformaldehyde for 8 minutes at room temperature. Subsequently, they were permeabilized using 0.1% Triton in PBS for 7 minutes. The fixed cells were blocked using 100 µL of blocking serum (normal serum from the Vectastain Elite ABC Kit) for another 8 minutes.
The cells were then incubated at room temperature for 1 hour and 30 minutes with the primary antibodies EGFR and Caspase-3, using the concentrations recommended by the manufacturers. After washing the cells three times with PBS, they were treated with a secondary antibody (Biotinylated universal antibody from the Vectastain Elite ABC kit) for 30 minutes at room temperature.
Following two 1-minute PBS washes, the tertiary antibody (Vectastain Elite ABC Reagent, 100µL) was added to the coverslips and incubated for 20 minutes. In the dark and at room temperature, 100 µL of TSA-CY5 reagent was added to each well and left for 5 minutes. Lastly, cells were washed and counterstained with DAPI (4',6-diamidino-2-phenylindole) to visualize the nuclei. Images were captured using a Nikon fluorescent microscope. Using the ImageJ software, the mean fluorescent intensity (MFI) of EGFR and Caspase-3 staining was quantified. To account for cell number and variability in staining, the MFI was normalized to the DAPI fluorescence signal, yielding the normalized mean fluorescent intensity (MFI). Regions of interest (ROIs) were defined to exclude areas without cells or with excessive background staining.
E. Apoptosis Assay
HCT-116 cells were seeded in 6 well plates and treated based on the treatment groups and drug concentrations outlined earlier. After 48 hours of treatment, the culture media was removed, and cells were washed twice with PBS to eliminate any residual media. Supernatants from both media and PBS washes were collected in 15ml Falcon tubes for further analysis.
To facilitate cell detachment, 1 ml of Tryple E was added to each well and left for a few minutes in the incubator. The Tryple E was subsequently inactivated by adding 1 ml of media, and the cell suspension was transferred to labelled tubes. After centrifugation (3 minutes at 1500 rpm), the supernatant was discarded, and the cells were washed with cold PBS to remove excess media and FBS. The cells were resuspended in 1x Annexin V Binding Solution (100 μL), and Annexin V FITC Conjugate (5 μL) and PI Solution (5 μL) were added to assess apoptosis.
The cell suspension was incubated for 15 minutes at room temperature, protected from light, followed by the addition of 400 μL of 1x Annexin V Binding Solution.
The samples were mixed well and transferred through a cell strainer cap into FACS tubes with proper labelling. Acquisition and analysis of dual stained cells was done using flow cytometry. Early apoptotic cells (Annexin V+ PI-) and late apoptotic/necrotic cells (Annexin V+ PI+) were differentiated. Data was evaluated with BD Accuri C6 + software (version 1.0.23.1).
F. Cell Cycle Assay
Initially, cells were cultured in 6 well plates and subjected to treatments (as outlined earlier) after 24 hours. Following a 48-hour incubation period, the cells were harvested and processed for analysis. Harvested cells were washed thoroughly with PBS to remove any residues of culture media and foetal bovine serum (FBS).
Subsequently, the cell suspension was subjected to centrifugation (3 minutes at 1500 rpm), and the pellet was washed again with cold PBS to remove any excess media and FBS. To facilitate proper fixation and permeabilization for subsequent staining, the pellet was treated with 70% ethanol and was allowed to fix for 30 minutes on ice.
After the fixation process, the cells were centrifuged (5 minutes at 1500 rpm) again, and the supernatant was carefully aspirated. The cells were washed twice with PBS and incubated with 0.5 mL FxCycle™ PI/RNase Staining Solution. Following an incubation period at room temperature for 30 minutes, protected from light. The stained samples were analysed without further washing using a BD Accuri C6 plus flow cytometer (BD Biosciences, San Diego, CA, USA). Data analysis was carried out using BD Accuri C6 plus software (version 1.0. 23..1).
G. Statistical Analysis
For each experiment, data were collected in duplicate samples to ensure reproducibility. Quantitative data was analysed using Minitab 20® Software (State College, PA, USA).
Statistical analysis was performed using one-way analysis of variance (ANOVA) followed by post hoc tests, with two-sample T-test used to compare some treatments as applicable. Results were considered statistically significant at P < 0.05. Graphs and figures were generated to visually represent the data. Representative images and histograms were selected for inclusion in the results section.
H. Ethical Considerations
Ethical approval for this study was obtained from the Middlesex University Ethics review board. The study adhered to the ethical guidelines and regulations for the use of laboratory facilities and experimental procedures involving human cell lines. All necessary precautions were taken to ensure the safety and welfare of researchers involved in the study. A copy of the ethical approval letter is provided in the appendices for reference.
III. RESULTS
A. Immunocytochemical analysis of EGFR expression in colorectal cancer (HCT-116) cells post-treatment.
To determine the effect of Thymoquinone on the expression of EGFR, HCT-116 cells were treated with Thymoquinone and 5-fluorouracil, singly and in combination, and subjected to immunocytochemistry analysis. Fluorescence microscopy images (Figure 4a) illustrates the cytochemical changes observed post-treatment. There is a visible reduction in EGFR-stained cells(pink) between the control(I) and the TQ(III), 5FU(IV) and TQ + 5-FU group(V). A similar difference is not seen when comparing DMSO(II) and Control(I). This is further demonstrated with quantitative analysis of the mean fluorescent intensity (MFI) (Figure 4b). Notably, there was no significant difference in MFI (p ≥ 0.05) observed between untreated cells and Vehicle control (DMSO). In contrast, cells treated with TQ, and 5-FU showed a pronounced reduction in MFI (p ≤ 0.001) compared to the untreated cells, with TQ demonstrating the most substantial decrease. (Figure 4b). Interestingly the combined drug treatment (TQ + 5-FU) resulted in only a moderate MFI decline (p ≤ 0.05).

Fig 4.Representative immunofluorescence images and quantitative analysis of immunofluorescence intensity for EGFR. (a) Cells were stained directly using EGFR primary antibodies to visualize EGFR protein (shown in pink) and counterstained with DAPI to stain the nucleus (shown in blue). Cells were captured using Fluorescence microscopy at 400X magnification with representative images obtained from two replicates. Scale bar 50 µm (b) Graph illustrates the mean florescence intensity (MFI) across experimental groups. Values are expressed as means ± standard error. Differences in significance between each group and the control (untreated cells) are denoted in the figure. (* P ≤ 0.05, ** P ≤ 0.01, *** P ≤ 0.001 NSD= No significant difference).
B. Immunocytochemical analysis of Caspase-3 expression in colorectal cancer (HCT-116) cells post-treatment.
To investigate the potential pro-apoptotic effects of Thymoquinone on HCT-116 cells, we investigated its effects on the expression of the apoptotic marker, Caspase-3. Fluorescence microscopy images (Figure 5a) captures the cytochemical changes that occurred post-treatment. There is an observable increased expression of Caspase-3(Pink) in the TQ(III), 5-FU(IV) and TQ + 5-FU(V) cells as compared with the untreated cells(I) and vehicle control (III). The quantified mean fluorescent intensity (MFI) (Figure 5b) further demonstrates these differences. Notably, there was no significant difference in MFI (P ≥ 0.05) observed between untreated cells and Vehicle control (DMSO). On the other hand, cells treated with TQ, 5-FU and the combined drug treatment (TQ + 5-FU) showed a highly significant increase in MFI (P ≤ 0.001) compared to the untreated cells.

Fig 5. Representative immunofluorescence images showing the expression of Caspase-3 in HCT-116 cells (a) Cells were stained directly using Caspase-3 primary antibodies to visualize Caspase-3 protein (shown in pink) and counterstained with DAPI to stain the nucleus (shown in blue). Cells were captured using Fluorescence microscopy at 400X magnification with representative images obtained from two replicates. Scale bar 50 µm. b) Graph illustrates the mean florescence intensity (MFI) across experimental groups. Values are expressed as means ± standard error. Differences in significance between each group and the control (untreated cells) are denoted in the figure. (* P ≤ 0.05, ** P ≤ 0.01, *** P ≤ 0.001 NSD= No significant difference).
C. Cell Cyle Analysis Showing the effects of Thymoquinone and 5-FU on HCT-116 cells.
Cell cycle analysis revealed four distinct cell populations in HCT-116 cells which were indicative of cells in the pre-G1, G1, S and G2/M phases of the cell cycle (Figure 6a). Notably, distinctions in the pre-G1 phase of the cell cycle emerged across the treatment groups. comparative analysis revealed that the treatment with 5-FU led to the highest increase in cells in the pre-G1 phase (7.4% ± 0.1%) which was significantly higher than untreated cells (1.1% ± 0.2%, P ≤ 0.05), DMSO (1.3% ± 0.05%, P ≤ 0.05), and the Thymoquinone group (1.7% ±0.4%, P ≤ 0.05). A similar increase was observed in cells treated with a combination of 5FU and TQ (6.6% ± 0.3%) although the difference between this group and 5-FU alone wasn’t statistically significant (Figure 6b). The control, DMSO and TQ cell groups exhibited no significant statistical difference (P ≥ 0.05) in their measurements.
In the G1 phase, the untreated cells recorded an average of 6.1% (± 1.85%). In comparison, the DMSO-treated cells indicated a value of 5.7% (± 0.3%). The cells treated with TQ presented 3.9% (± 1.2%) in the G1 phase. Meanwhile, cells under 5-FU treatment showed 4.1% (± 0.85%), and those receiving the combination treatment of 5-FU and TQ had 3.3% (± 0.25%).
For the S phase, the untreated cells had a mean value of 2.0% (± 0.6%)., marking them highest among all groups. The 5-FU treated cells followed closely with 1.5% (± 0.5%)., whereas both DMSO and the combination of 5FU and TQ treatments had identical means of 1.4% (±0.2%). The Thymoquinone (TQ) treatment group presented the lowest mean for this phase at 1.3% (± 0.4%). As observed In the G2 phase, the control group displayed 5.8% (±1.5%). of cells, while the DMSO group showed a decrease to 5.0% (±0.4%). TQ treatment led to 3.8% (±0.1.2%) of cells in G2. Notably, the 5-FU group had the highest increase in the G2 phase population at 6.4% (±2.5%). The combination of TQ and 5-FU resulted in 4.1% (±0.6%). of cells in this phase which may suggest no possible additive effect with TQ.
Statistical analysis of difference in the G1, S and G2/M phases showed no significant difference (P ≥ 0.05) among the different treatment groups in each phase (Figure 6b).

Fig 6. Effects of Thymoquinone and 5-FU on cell cycle progression of human colorectal cancer cells (HCT-116). A) Representative histograms after 48-hour incubation with drug treatments. The distribution of cells in the different phases of the cell cycle was determined using flow cytometry with analysis done using the BD Accuri C6 pus software. The histograms shown here represent a typical result of a duplicate sample. B) Graphical representation of the histogram results. Data are expressed as the mean ± standard error of mean (SEM) of two replicates. One-way ANOVA was done for statistical analysis to compare each group against the control (untreated cells). (* P ≤ 0.05, ** P ≤ 0.01, *** P ≤ 0.001 NSD= No significant difference
D. Differential Apoptotic Responses of HCT-116 cells to Thymoquinone, 5-FU, and Their Combination
Using the Annexin V/PI apoptosis analysis, we observed the vitality and varied apoptotic responses of human colorectal cancer cells to drug-induced cell death by observing the proportion of cells in different phases of the graph (figure 7a). Overall, there was significant reduction in cell viability observed in all groups with untreated cells displaying a viability of 35.9% (± 8.3%). Cells treated with DMSO had a viability of 42% (±2.1 %). TQ-treated cells showed a viability of 42% (± 1.41 %), whereas 5-FU and TQ + 5-FU treated cells recorded 26.1% (±1.4 %) and 38.6 % (±9.1 %) viability respectively.
Furthermore, Control cells showed an early apoptosis rate of 5.25% (±0.3 %). With DMSO, this rate slightly increased to 6.4% (±0.1%). TQ induced early apoptosis in 9.15% (±1.8 %) of cells, while 5-FU led to a substantial increase, with 21.75% (± 5.9 %) of cells in early apoptosis. The combination of TQ + 5-FU showed an early apoptosis rate of 14.5% (± 8.7%) which may point towards the absence of an additive effect.
Control cells in late apoptosis were 58.45% (± 8.4%). With DMSO, TQ, and 5-FU treatments, the rates were 51.15% (±12.6 SE), 48.2% (±3.1%), and 51.7% (± 4.6%), respectively. Notably, the TQ and 5-FU combination induced a prominent necrotic response of 22.15% (± 15%), a contrast to other treatments which ranged between 0.4% (±0.2 %) to 0.45% (±0.2 %) in necrosis.
Overall, while there appeared to be noted variations in cell viability across the groups, these differences were not statistically significant (p ≥ 0.05) when assessed with one-way ANOVA and further paired t-test comparisons.

Fig 7. The apoptotic activity of HCT116 cells after treatment with TQ and 5-FU. Cells were stained with FITC and PI and analysed by Flow Cytometry. A) Representative Flow cytometry plots. Experiments were performed in duplicates with data shown as mean ± standard error of mean (SEM). B) A graphical comparison of apoptotic cell percentages between treated and untreated cells. Data was analysed using one-way ANOVA with Tukey post-hoc test. Single Thymoquinone, 5-Flourouracil and their combination were further compared by two-sample t-test.
IV. DISCUSSION
In recent years, there has been a growing interest in exploring Thymoquinone's anti-cancer effects and its potential synergistic effects with other chemotherapeutic agents in the treatment of various cancers.[13].This study was designed to assess the anti-cancer effects of thymoquinone (TQ) on colorectal cancer, employing various techniques to investigate TQ's effect on EGFR expression, its pro-apoptotic effects through Caspase-3 expression and flow cytometry, and its effects on cell cycle progression. The results revealed that TQ significantly reduced the expression of EGFR, increased the expression of Caspase-3 and induced apoptosis, increased the pre-G1 phase of the cell cycle, and showed synergistic apoptotic effects when combined with 5-FU.
In many malignancies, including colorectal cancer, the epidermal growth factor receptor (EGFR) – a transmembrane receptor tyrosine kinase – is widely overexpressed and is often associated with poorer clinical outcomes[48]. One of the paramount findings of the study was the pronounced reduction of EGFR expression in cells treated with TQ compared to untreated cells (Figure 4b). Previous studies have shown possible molecular mechanisms for this observation, with findings that suggest that TQ exerts an inhibitory effect on several upstream kinases and attenuates JAK-2 and src-mediated EGFR phosphorylation[11]. Furthermore, the 5-FU-treated cells also showed a notable decline in EGFR expression, though not as pronounced as the TQ group. 5-FU being a fluorinated analogue of uracil, exerts its cytotoxic effects by inhibiting thymidylate synthase (TYMS) enzyme leading to impairment in cellular DNA synthesis in malignant cells[49]. However, its impact on molecular signalling pathways involved in cellular apoptosis and autophagy is increasingly recognized[50]. EGFR activates several intracellular cascades, including the PI3K/AKT-mTOR and the RAS/RAF/MEK/ERK pathways[51]. A study by Xiong et al. found that 5-FU treatment resulted in reduced mTOR activity in Bax/PUMA deficient CRC cells[24]. By influencing these pathways, 5-FU could indirectly modulate the overall EGFR signalling in cancer cells thereby reducing the receptor's activation or expression.
Interestingly, the combination of TQ and 5-FU resulted in a moderate decline in EGFR expression. While the reduction was less than that observed with TQ alone, it was significant compared to untreated cells. This combined effect implies that while both agents might independently target EGFR, their combined action might involve different or overlapping mechanisms. The synergistic or antagonistic nature of their relationship in the context of EGFR is an area of further research.
The results further indicated that the pro-apoptotic effects of TQ were evident through the increased expression of Caspase-3. Although the exact nature of their function is unknown, the activation of caspase proteases is essential for apoptotic cell death. Caspases that are activated, particularly caspase-3, control nuclear condensation, membrane blebbing, and DNA fragmentation[52]. The augmented expression of Caspase-3 upon TQ treatment indicates that TQ prompts apoptotic cell death in CRC(HCT-116) cells. These findings are similar with research by Kundu et al., who found that TQ treatment increased apoptosis and decreased HCT-116 cancer cell viability in a dose- and time-dependent way associated with elevated levels of the pro-apoptotic Bax (BCL-2 associated X) and downregulation of the anti-apoptotic Bcl-2 (B-cell lymphoma-2) and Bcl-xL protein was downregulated[11].Treatment with 5-FU induced the highest expression levels of Caspase-3, and this is in keeping with previous studies that have confirmed increased activity of Caspase-3 and Caspase-8 in 5-FU treated human colorectal cancer cells [53].The combined effect of TQ and 5-FU on caspase-3 expression was notably less pronounced compared to their individual impacts. This phenomenon, interestingly, mirrors the observations made regarding EGFR expression in this study. Such an interaction suggests a potential modulatory or non-synergistic relationship between TQ and 5-FU. Prior research on combined drug therapies in CRC has underscored the complexity of their pharmacodynamic interactions[54].For instance, studies on other drug combinations have occasionally noted diminished efficacy when certain agents are combined, due to potential interferences in their modes of action[47]. Similarly, the observed subdued effect in our study, when TQ and 5-FU are combined, raises questions about optimal dosing or sequence of administration to harness their full therapeutic potential. Moreover, potential interactions between TQ and 5-FU at a molecular level, when combined, could lead to structural changes that make either less available or less active. Such interactions could be a result of binding affinities or competition for the same cellular targets, as highlighted in some combined therapeutic studies[55].
Previous studies have shown that TQ affects cell cycle progression at different phases of the cycle[56].An in vitro study by Wirries et al., (2010) reported G2/M arrest in p53-competent HCT116 cells at lower concentrations (10 μM) of TQ that had been modified with an unsaturated fatty acid to amplify its effect[57]. Other researchers found that G0/G1 arrest was seen at a TQ concentration of 60 μM after 24 hours of incubation. Following 48 hours of incubation, there was also pre-G1 accumulation of cells which was drastically increased at higher concentrations of TQ (100 μM) [58]. Similarly, the present study found a moderate increase in pre-G1 cell accumulation in cells treated with TQ, with associated reductions in the G0/G1, S and G2/M. This indicates apoptosis induction by TQ that resulted in concomitant shifts in the % of cells in other phases. An increase in the pre-G1 cell population in HCT-116 cells with similar accompanying phase reductions has also been found in a study that aimed to assess TQ’s ability to induce apoptosis and inhibit tumour growth in carcinoma cells(breast MDA-MB-468, T-47DMDA-MB-468, MCF-7, and colon HCT-116) with different known sensitivities[59].
The anticipated G1 or G2/M cell cycle arrest, typically associated with TQ treatment, was not observed. One possible explanation might centre on the concentration and duration of TQ exposure. While a few studies have observed cell cycle arrest at lower concentrations of TQ (< 30 μM)[60], typical findings were seen at higher concentrations in a time and dose-dependent manner[13, 57].Molecular studies investigating cell cycle regulating factors influenced by TQ have found that its effects are associated with an up-regulation of p53 and p21cip1/waf1, and a down-regulation of Bcl-2 protein and cyclin E which is essential for progression from the G1 to the S phase[61].
It is well established that both the intrinsic and extrinsic apoptotic pathways are dysregulated in colorectal cancer and this has increased research interest in developing specific apoptotic chemotherapeutic targets[55]. In this work, TQ induced a moderate rise in the early apoptotic population with a more significant increase seen in the late apoptotic population. These correlates with our other findings of an increase in casase-3 expression and pre-G1 cell cycle accumulation. According to studies that had similar findings, TQ’s apoptotic effects can be linked to an increase in the expression of the proapoptotic protein Bax, and decreased expression of anti-apoptotic proteins Bcl-cl and Bcl-2. They also found that when cells are pre-treated with pan-caspase inhibitors, these changes were not replicated hinting that by inducing caspase-3 activity, TQ primarily acts at the intrinsic apoptotic pathway[11, 52, 58].There were also significant late apoptotic cells seen in the untreated cell and vehicle control group. This likely may have developed as a result of technical and environmental factors with the experiment. While attempts were made to standardize steps for each plate, pipetting errors during collection/transfer, as well as possible bacterial contamination could have occurred. Further repeats with a different cell batch may be beneficial in confirming the reproducibility of this result. The overall reliability of the Annexin V/PI apoptosis assay results was taken into consideration in light of this and other indicators of apoptosis (increased caspase-3 expression and raised pre-G1 cell events) supports TQ’s pro-apoptotic effects.
5-Flourouracil and phytochemical drug combinations have been extensively studied for a wide range of carcinomas. In a study of colon cancer, simultaneous apoptosis and autophagic cell death were seen[62]. This may be seen as an antagonistic relationship brought on by the cytoprotective nature of autophagy[63](Dey et al., 2020).
When combined with TQ, some studies in triple-negative breast cancer, pancreatic cancer and osteosarcomas have found a synergistic effect[54, 64]. In this study, we found that TQ + 5-FU combination showed varied responses when compared with their individual treatments with no conclusive synergistic action observed. While it induced late apoptosis, increased caspase-3 expression and caused a moderate reduction in EGFR-expression, there was no significant difference shown when compared with the effects of TQ or 5-FU alone. Further studies using measures such as the ccombination Index (CI) and Dose-Reduction Index (DRI), could help properly delineate this interaction.
This study has some major limitations. While it provides valuable insights into the anti-cancer effects of thymoquinone on human colorectal cancer cells in vitro, One notable limitation is the absence of a non-cancerous control cell line to serve as a comparative baseline. Using a control cell line, particularly one that is of similar tissue origin but non-transformed, offers valuable insights into the specificity of the anti-cancer effects of thymoquinone. Such comparisons can help ascertain whether the observed effects are exclusive to cancerous cells or if they also manifest in normal cells. In the context of potential therapeutics, understanding this distinction is crucial to predict potential side effects or toxicities in normal tissues. Additionally, control cell lines help in eliminating or accounting for any non-specific effects that may arise during treatment, ensuring the observed results truly reflect the effects on the cancerous cells and not some general cellular response to treatment. Future studies should consider incorporating control cell lines to elucidate the specific effects of thymoquinone on colorectal cancer cells vis-à-vis normal cells. Furthermore, it's essential to note that using a singular cell line, such as HCT-116, might not capture the complete heterogeneity of colorectal cancer. Different colorectal cancer cell lines or primary cells from patient tumours may respond differently to TQ treatment. In addition, while the effects of TQ on EGFR signalling and caspase-3 activation were observed, the downstream consequences on cell signalling pathways and other cellular functions were not extensively explored. Assays to assess migration, invasion, and other functional aspects could provide a more comprehensive picture of TQ's anti-cancer properties. Lastly, it's essential to recognize that in vitro studies, while offering controlled conditions, do not always translate directly to in vivo scenarios. Factors like drug metabolism, systemic immune responses, and tumour-stroma interactions can significantly influence drug efficacy in a living organism. Future studies employing animal models or patient-derived xenografts could validate and expand upon these findings. Probably the most significant limitation is in the methodology. Due to delays in the arrival of some procured reagents, and the time constraints for the experiment, independent experiments could not be repeated for the flow cytometry (cell cycle analysis and apoptosis).
A. Perspectives and Future Prospects
This study adds to an extensive pool of in vitro research on thymoquinone that has brought to light its multifaceted mechanisms of action, its efficacy even in small dosages, and its potential in combination therapies in the treatment of various malignancies, including colorectal cancer[7]. Future in vitro studies could explore more accurate techniques such as growth kinetics and whole genome sequencing/transcriptomics, to assess the synergistic effects of Thymoquinone and 5-FU. In addition, further biochemical and molecular biological explorations are essential to unearth the specific signalling pathways that are modulated by TQ. Advanced techniques like single-cell RNA sequencing or CRISPR-based functional screens could help in pinpointing the precise pathways and molecules influenced by thymoquinone leading to more specific targets in drug development and guiding possible combinatorial treatments. Considering that a major limitation of TQ’s use is its poor solubility and bioavailability in aqueous solutions[65], the development of novel drug delivery systems could be pivotal in accelerating its clinical applications. Several Thymoquinone nanoparticles are in development that not only improve its pharmacokinetics, but have been found to increase both non-enzymatic and enzymatic antioxidant levels and mitigate against chemotherapeutic induce inflammation by decreasing levels of TNF-α, IL-1β, and NF-kB[66, 67]. While in vitro findings offer valuable insights, the real testament of any therapeutic agent lies in its in vivo efficacy. More Anima models, particularly murine models would not only offer deeper insights into thymoquinone's bioavailability and potential side effects but also its interaction with the tumour microenvironment. Furthermore, with current success in in vivo experiments[58] and advancements in improving its bioavailability [68] transition to more clinical trials will then be the next natural area of focus with better evaluation of its therapeutic window, potential side effects, and optimal administration routes in a clinical setting.
B. Conclusions
In conclusion, the present study demonstrates that Thymoquinone exerts its anti-cancer effects by inducing apoptosis with associated increased caspase-3 expression and pre-G1 cell population, and decreased expression of EGFR in human colorectal cancer (HCT-116) cell lines.
Because there are multiple molecular signalling pathways that may be linked to TQ’s mediation of these changes, there is a need for further studies to explore these effects and offer new insights. On the basis of this, it has been shown that TQ is a promising chemotherapeutic agent in the treatment of colorectal cancer, and there is a role for its future use with current established therapies.
References
[1] Xi Y and Xu P 2021 Global colorectal cancer burden in 2020 and projections to 2040 Transl Oncol 14 101174 [2] Dekker E, Tanis P J, Vleugels J L A, Kasi P M and Wallace M B 2019 Colorectal cancer Lancet 394 1467-80 [3] Baidoun F, Elshiwy K, Elkeraie Y, Merjaneh Z, Khoudari G, Sarmini M T, Gad M, Al-Husseini M and Saad A 2021 Colorectal Cancer Epidemiology: Recent Trends and Impact on Outcomes Curr Drug Targets 22 998-1009 [4] Matsuda T, Yamashita K, Hasegawa H, Oshikiri T, Hosono M, Higashino N, Yamamoto M, Matsuda Y, Kanaji S, Nakamura T, Suzuki S, Sumi Y and Kakeji Y 2018 Recent updates in the surgical treatment of colorectal cancer Ann Gastroenterol Surg 2 129-36 [5] Häfner M F and Debus J 2016 Radiotherapy for Colorectal Cancer: Current Standards and Future Perspectives Visc Med 32 172-7 [6] Fujita S and Kotake K 2014 [Chemotherapy] Nihon Rinsho 72 102-7 [7] Asaduzzaman Khan M, Tania M, Fu S and Fu J 2017 Thymoquinone, as an anticancer molecule: from basic research to clinical investigation Oncotarget 8 51907-19 [8] Edris A E 2009 Anti-cancer properties of Nigella spp. essential oils and their major constituents, thymoquinone and beta-elemene Curr Clin Pharmacol 4 43-6 [9] Khan M A, Chen H C, Tania M and Zhang D Z 2011 Anticancer activities of Nigella sativa (black cumin) Afr J Tradit Complement Altern Med 8 226-32 [10] Tabassum H, Ahmad A and Ahmad I Z 2018 Nigella sativa L. and Its Bioactive Constituents as Hepatoprotectant: A Review Curr Pharm Biotechnol 19 43-67 [11] Kundu J, Choi B Y, Jeong C H, Kundu J K and Chun K S 2014 Thymoquinone induces apoptosis in human colon cancer HCT116 cells through inactivation of STAT3 by blocking JAK2- and Src?mediated phosphorylation of EGF receptor tyrosine kinase Oncol Rep 32 821-8 [12] Shahin Y R, Elguindy N M, Abdel Bary A and Balbaa M 2018 The protective mechanism of Nigella sativa against diethylnitrosamine-induced hepatocellular carcinoma through its antioxidant effect and EGFR/ERK1/2 signaling Environ Toxicol [13] Almajali B, Al-Jamal H A N, Taib W R W, Ismail I, Johan M F, Doolaanea A A and Ibrahim W N 2021 Thymoquinone, as a Novel Therapeutic Candidate of Cancers Pharmaceuticals (Basel) 14 [14] Imran M, Rauf A, Khan I A, Shahbaz M, Qaisrani T B, Fatmawati S, Abu-Izneid T, Imran A, Rahman K U and Gondal T A 2018 Thymoquinone: A novel strategy to combat cancer: A review Biomedicine & Pharmacotherapy 106 390-402 [15] Mariotto A B, Yabroff K R, Shao Y, Feuer E J and Brown M L 2011 Projections of the cost of cancer care in the United States: 2010-2020 J Natl Cancer Inst 103 117-28 [16] Pathy S, Lambert R, Sauvaget C and Sankaranarayanan R 2012 The incidence and survival rates of colorectal cancer in India remain low compared with rising rates in East Asia Dis Colon Rectum 55 900-6 [17] Yang Y, Han Z, Li X, Huang A, Shi J and Gu J 2020 Epidemiology and risk factors of colorectal cancer in China Chin J Cancer Res 32 729-41 [18] Center M M, Jemal A, Smith R A and Ward E 2009 Worldwide variations in colorectal cancer CA Cancer J Clin 59 366-78 [19] Hankey W, Frankel W L and Groden J 2018 Functions of the APC tumor suppressor protein dependent and independent of canonical WNT signaling: implications for therapeutic targeting Cancer Metastasis Rev 37 159-72 [20] Disoma C, Zhou Y, Li S, Peng J and Xia Z 2022 Wnt/?-catenin signaling in colorectal cancer: Is therapeutic targeting even possible? Biochimie 195 39-53 [21] Midthun L, Shaheen S, Deisch J, Senthil M, Tsai J and Hsueh C T 2019 Concomitant KRAS and BRAF mutations in colorectal cancer J Gastrointest Oncol 10 577-81 [22] Petko Z, Ghiassi M, Shuber A, Gorham J, Smalley W, Washington M K, Schultenover S, Gautam S, Markowitz S D and Grady W M 2005 Aberrantly methylated CDKN2A, MGMT, and MLH1 in colon polyps and in fecal DNA from patients with colorectal polyps Clin Cancer Res 11 1203-9 [23] Stidham R W and Higgins P D R 2018 Colorectal Cancer in Inflammatory Bowel Disease Clin Colon Rectal Surg 31 168-78 [24] Xiong H Y, Guo X L, Bu X X, Zhang S S, Ma N N, Song J R, Hu F, Tao S F, Sun K, Li R, Wu M C and Wei L X 2010 Autophagic cell death induced by 5-FU in Bax or PUMA deficient human colon cancer cell Cancer Lett 288 68-74 [25] Amersi F, Agustin M and Ko C Y 2005 Colorectal cancer: epidemiology, risk factors, and health services Clin Colon Rectal Surg 18 133-40 [26] Ocalewski J, Jankowski M, Zegarski W, Migdalski A and Buczkowski K 2023 The Role of Health Behaviors in Quality of Life: A Longitudinal Study of Patients with Colorectal Cancer Int J Environ Res Public Health 20 [27] Hagland H R, Berg M, Jolma I W, Carlsen A and Søreide K 2013 Molecular pathways and cellular metabolism in colorectal cancer Dig Surg 30 12-25 [28] Rentsch M, Schiergens T, Khandoga A and Werner J 2016 Surgery for Colorectal Cancer - Trends, Developments, and Future Perspectives Visc Med 32 184-91 [29] Pardini B, Kumar R, Naccarati A, Novotny J, Prasad R B, Forsti A, Hemminki K, Vodicka P and Lorenzo Bermejo J 2011 5-Fluorouracil-based chemotherapy for colorectal cancer and MTHFR/MTRR genotypes Br J Clin Pharmacol 72 162-3 [30] Bastos D A, Ribeiro S C, de Freitas D and Hoff P M 2010 Combination therapy in high-risk stage II or stage III colon cancer: current practice and future prospects Ther Adv Med Oncol 2 261-72 [31] Fakih M and Wong R 2010 Efficacy of the monoclonal antibody EGFR inhibitors for the treatment of metastatic colorectal cancer Curr Oncol 17 Suppl 1 S3-17 [32] Ansari M J, Bokov D, Markov A, Jalil A T, Shalaby M N, Suksatan W, Chupradit S, Al-Ghamdi H S, Shomali N, Zamani A, Mohammadi A and Dadashpour M 2022 Cancer combination therapies by angiogenesis inhibitors; a comprehensive review Cell Commun Signal 20 49 [33] Tam S Y and Wu V W C 2019 A Review on the Special Radiotherapy Techniques of Colorectal Cancer Front Oncol 9 208 [34] Myint A S and Gérard J P 2020 Role of radiotherapy in the treatment of rectal cancer in older patients European Journal of Surgical Oncology 46 349-57 [35] Marijnen C A and Glimelius B 2002 The role of radiotherapy in rectal cancer Eur J Cancer 38 943-52 [36] Ansary J, Giampieri F, Forbes-Hernandez T Y, Regolo L, Quinzi D, Gracia Villar S, Garcia Villena E, Tutusaus Pifarre K, Alvarez-Suarez J M, Battino M and Cianciosi D 2021 Nutritional Value and Preventive Role of Nigella sativa L. and Its Main Component Thymoquinone in Cancer: An Evidenced-Based Review of Preclinical and Clinical Studies Molecules 26 [37] Homayoonfal M, Asemi Z and Yousefi B 2022 Potential anticancer properties and mechanisms of thymoquinone in osteosarcoma and bone metastasis Cell Mol Biol Lett 27 21 [38] Hajhashemi V, Ghannadi A and Jafarabadi H 2004 Black cumin seed essential oil, as a potent analgesic and antiinflammatory drug Phytother Res 18 195-9 [39] Kohandel Z, Farkhondeh T, Aschner M and Samarghandian S 2021 Anti-inflammatory effects of thymoquinone and its protective effects against several diseases Biomedicine & Pharmacotherapy 138 111492 [40] Sakib R, Caruso F, Aktar S, Belli S, Kaur S, Hernandez M and Rossi M 2023 Antioxidant Properties of Thymoquinone, Thymohydroquinone and Black Cumin (Nigella sativa L.) Seed Oil: Scavenging of Superoxide Radical Studied Using Cyclic Voltammetry, DFT and Single Crystal X-ray Diffraction Antioxidants (Basel) 12 [41] Liu T, Zhang L, Joo D and Sun S C 2017 NF-?B signaling in inflammation Signal Transduct Target Ther 2 17023- [42] Samarghandian S, Azimi-Nezhad M and Farkhondeh T 2019 Thymoquinone-induced antitumor and apoptosis in human lung adenocarcinoma cells J Cell Physiol 234 10421-31 [43] Paramasivam A, Sambantham S, Shabnam J, Raghunandhakumar S, Anandan B, Rajiv R, Vijayashree Priyadharsini J and Jayaraman G 2012 Anti-cancer effects of thymoquinone in mouse neuroblastoma (Neuro-2a) cells through caspase-3 activation with down-regulation of XIAP Toxicol Lett 213 151-9 [44] Karim S, Burzangi A S, Ahmad A, Siddiqui N A, Ibrahim I M, Sharma P, Abualsunun W A and Gabr G A 2022 PI3K-AKT Pathway Modulation by Thymoquinone Limits Tumor Growth and Glycolytic Metabolism in Colorectal Cancer Int J Mol Sci 23 [45] Aumeeruddy M Z, Zengin G and Mahomoodally M F 2018 A review of the traditional and modern uses of Salvadora persica L. (Miswak): Toothbrush tree of Prophet Muhammad J Ethnopharmacol 213 409-44 [46] Kundu J, Choi B Y, Jeong C-H, Kundu J K and Chun K-S 2014 Thymoquinone induces apoptosis in human colon cancer HCT116 cells through inactivation of STAT3 by blocking JAK2- and Src?mediated phosphorylation of EGF receptor tyrosine kinase Oncol Rep 32 821-8 [47] Roepke M, Diestel A, Bajbouj K, Walluscheck D, Schonfeld P, Roessner A, Schneider-Stock R and Gali-Muhtasib H 2007 Lack of p53 augments thymoquinone-induced apoptosis and caspase activation in human osteosarcoma cells Cancer Biol Ther 6 160-9 [48] Lo Nigro C, Ricci V, Vivenza D, Granetto C, Fabozzi T, Miraglio E and Merlano M C 2016 Prognostic and predictive biomarkers in metastatic colorectal cancer anti-EGFR therapy World J Gastroenterol 22 6944-54 [49] Longley D B, Harkin D P and Johnston P G 2003 5-fluorouracil: mechanisms of action and clinical strategies Nat Rev Cancer 3 330-8 [50] Ghafouri-Fard S, Abak A, Tondro Anamag F, Shoorei H, Fattahi F, Javadinia S A, Basiri A and Taheri M 2021 5-Fluorouracil: A Narrative Review on the Role of Regulatory Mechanisms in Driving Resistance to This Chemotherapeutic Agent Front Oncol 11 658636 [51] Seshacharyulu P, Ponnusamy M P, Haridas D, Jain M, Ganti A K and Batra S K 2012 Targeting the EGFR signaling pathway in cancer therapy Expert Opin Ther Targets 16 15-31 [52] El-Mahdy M A, Zhu Q, Wang Q E, Wani G and Wani A A 2005 Thymoquinone induces apoptosis through activation of caspase-8 and mitochondrial events in p53-null myeloblastic leukemia HL-60 cells Int J Cancer 117 409-17 [53] Violette S, Poulain L, Dussaulx E, Pepin D, Faussat A M, Chambaz J, Lacorte J M, Staedel C and Lesuffleur T 2002 Resistance of colon cancer cells to long-term 5-fluorouracil exposure is correlated to the relative level of Bcl-2 and Bcl-X(L) in addition to Bax and p53 status Int J Cancer 98 498-504 [54] Milczarek M, Pogorzelska A and Wiktorska K 2021 Synergistic Interaction between 5-FU and an Analog of Sulforaphane-2-Oxohexyl Isothiocyanate-In an In Vitro Colon Cancer Model Molecules 26 [55] Abraha A M and Ketema E B 2016 Apoptotic pathways as a therapeutic target for colorectal cancer treatment World J Gastrointest Oncol 8 583-91 [56] Almajali B, Al-Jamal H A N, Wan Taib W R, Ismail I, Johan M F, Doolaanea A A, Ibrahim W N and Tajudin S A 2021 Thymoquinone Suppresses Cell Proliferation and Enhances Apoptosis of HL60 Leukemia Cells through Re-Expression of JAK/STAT Negative Regulators Asian Pac J Cancer Prev 22 879-85 [57] Wirries A, Breyer S, Quint K, Schobert R and Ocker M 2010 Thymoquinone hydrazone derivatives cause cell cycle arrest in p53-competent colorectal cancer cells Exp Ther Med 1 369-75 [58] Gali-Muhtasib H, Diab-Assaf M, Boltze C, Al-Hmaira J, Hartig R, Roessner A and Schneider-Stock R 2004 Thymoquinone extracted from black seed triggers apoptotic cell death in human colorectal cancer cells via a p53-dependent mechanism Int J Oncol 25 857-66 [59] Al-Hayali M, Garces A, Stocks M, Collins H and Bradshaw T D 2021 Concurrent Reactive Oxygen Species Generation and Aneuploidy Induction Contribute to Thymoquinone Anticancer Activity Molecules 26 5136 [60] Shoieb A M, Elgayyar M, Dudrick P S, Bell J L and Tithof P K 2003 In vitro inhibition of growth and induction of apoptosis in cancer cell lines by thymoquinone Int J Oncol 22 107-13 [61] Sherr C J and Roberts J M 1999 CDK inhibitors: positive and negative regulators of G1-phase progression Genes Dev 13 1501-12 [62] Alnuqaydan A M, Rah B, Almutary A G and Chauhan S S 2020 Synergistic antitumor effect of 5-fluorouracil and withaferin-A induces endoplasmic reticulum stress-mediated autophagy and apoptosis in colorectal cancer cells Am J Cancer Res 10 799-815 [63] Dey D K, Chang S N, Vadlamudi Y, Park J G and Kang S C 2020 Synergistic therapy with tangeretin and 5-fluorouracil accelerates the ROS/JNK mediated apoptotic pathway in human colorectal cancer cell Food and Chemical Toxicology 143 111529 [64] Sarman H, Bayram R and Sb B 2016 Anticancer drugs with chemotherapeutic interactions with thymoquinone in osteosarcoma cells European review for medical and pharmacological sciences 20 7 1263-70 [65] Al-Jassir M S 1992 Chemical composition and microflora of black cumin (Nigella sativa L.) seeds growing in Saudi Arabia Food Chemistry 45 239-42 [66] Harakeh S, Qari Y, Tashkandi H, Almuhayawi M, Saber S H, aljahdali E, El-Shitany N, Shaker S, Lucas F, Alamri T, Al-Jaouni S and Mousa S 2022 Thymoquinone nanoparticles protect against cisplatin-induced nephrotoxicity in Ehrlich carcinoma model without compromising cisplatin anti-cancer efficacy Journal of King Saud University - Science 34 101675 [67] Mondéjar-López M, López-Jiménez A J, Martínez J C G, Ahrazem O, Gómez-Gómez L and Niza E 2022 Thymoquinone-Loaded Chitosan Nanoparticles as Natural Preservative Agent in Cosmetic Products Int J Mol Sci 23 [68] Mohammadabadi M R and Mozafari M R 2018 Enhanced efficacy and bioavailability of thymoquinone using nanoliposomal dosage form Journal of Drug Delivery Science and Technology 47 445-53
Copyright
Copyright © 2023 Beshikwashi Peter Ugbe, Roopika Chandran. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Download Paper
Paper Id : IJRASET56786
Publish Date : 2023-11-19
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

