Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
AI-Driven Hormonal Profiling: A Game-Changer in Polycystic Ovary Syndrome Prevention
Authors: Karthik Chowdary Tsaliki
DOI Link: https://doi.org/10.22214/ijraset.2024.61001
Certificate: View Certificate
Abstract
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder that impacts women during their reproductive years. It is characterized by hormonal imbalances, irregular menstrual cycles, and the presence of polycystic ovaries [1]. The incorporation of Artificial Intelligence (AI) in healthcare has provided new opportunities for the prevention and early detection of PCOS [2]. This article delves into the potential of AI in addressing the risk factors linked to PCOS. By utilizing machine learning algorithms, it can analyze intricate health data, detect patterns that indicate hormonal imbalances, and create personalized prevention strategies [3, 4]. Through the analysis of individual health profiles, dietary habits, and lifestyle choices, AI-driven approaches empower healthcare professionals to detect subtle patterns that occur before PCOS symptoms arise. This allows for proactive intervention and timely treatment [5]. The integration of AI in PCOS prevention signifies a noteworthy progression in women\'s healthcare, enabling women to make well-informed choices and proactively address their reproductive health [6]. This article emphasizes the benefits of AI in analyzing intricate health data, its potential for detecting hormonal imbalances at an early stage, and its ability to customize prevention plans for individuals, ultimately promoting the overall well-being of women who are at risk of developing PCOS [7, 8].
Introduction
I. INTRODUCTION
Polycystic Ovary Syndrome (PCOS) is a multifaceted endocrine disorder that impacts a significant percentage of women in their reproductive years globally [9]. PCOS is a condition that involves hormonal imbalances, irregular menstrual cycles, and polycystic ovaries. It can lead to various reproductive and metabolic issues, such as infertility, insulin resistance, and a higher chance of developing type 2 diabetes [10, 11]. The causes of PCOS are still not fully understood, but experts believe that a combination of genetic, environmental, and lifestyle factors play a role in its development [12]. The integration of Artificial Intelligence (AI) in healthcare has become a promising solution to tackle the challenges linked to PCOS prevention and management [13]. This article delves into the potential of AI in addressing the risk factors linked to PCOS in women. It highlights the importance of early detection, personalized prevention strategies, and empowering women to make informed decisions regarding their reproductive health.
II. UNDERSTANDING PCOS
A. Definition and Prevalence of PCOS
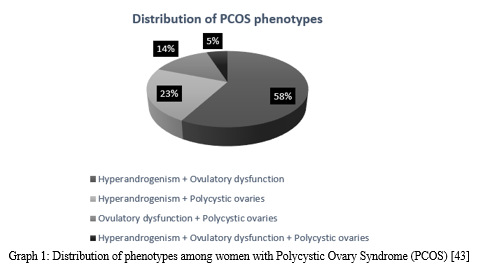
Polycystic Ovary Syndrome (PCOS) is a prevalent endocrine disorder that impacts a significant percentage of women in their reproductive years worldwide [14]. This condition is marked by a range of symptoms, such as irregular menstrual cycles, excess male hormones, and the presence of polycystic ovaries [15]. PCOS rates differ among various ethnicities, with higher prevalence seen in women of South Asian, Middle Eastern, and Hispanic backgrounds [16].
B. Hormonal Imbalances Associated With PCOS
PCOS is associated with a range of hormonal imbalances that contribute to its clinical manifestations. Here are some hormonal abnormalities that can occur:
- Individuals with PCOS often face increased levels of testosterone and other androgens, leading to symptoms such as hirsutism (excessive hair growth), acne, and male-pattern baldness [17].
- Insulin resistance is a prevalent issue among women with PCOS, impacting a significant majority of them. This can lead to increased insulin levels, referred to as compensatory hyperinsulinemia [18]. High levels of insulin can contribute to an increase in androgen production, further exacerbating the hormonal imbalance.
- Many women with PCOS may experience an imbalance in their LH to FSH ratio, which can disrupt normal ovarian function and lead to anovulation [19].
C. Reproductive and Metabolic Consequences of PCOS
PCOS is linked to various reproductive and metabolic effects that can greatly affect the health and well-being of women. These include:
- Infertility: PCOS is a significant contributor to anovulatory infertility, impacting a large majority of women with the condition [20]. PCOS can disrupt ovulation and decrease fertility due to hormonal imbalances and ovarian dysfunction.
- Menstrual Irregularities are Common in Women with PCOS: These can include infrequent menstrual periods or even the absence of periods due to anovulation [21].
- Metabolic Disorders: PCOS is linked to a higher likelihood of developing metabolic disorders like insulin resistance, impaired glucose tolerance, type 2 diabetes, dyslipidemia, and cardiovascular disease [22, 23].
The physical symptoms and reproductive consequences of PCOS can have a significant impact on one's psychological well-being, potentially causing feelings of anxiety, depression, and a decrease in overall quality of life [24].
III. RISK FACTORS FOR PCOS
|
Category |
Risk Factors |
|
Genetic |
Family history of PCOS |
|
Metabolic |
Obesity, insulin resistance, metabolic syndrome |
|
Endocrine |
Premature adrenarche, elevated anti-Müllerian hormone |
|
Environmental |
Exposure to endocrine-disrupting chemicals |
Table 1: Risk factors associated with the development of Polycystic Ovary Syndrome [40, 41]
IV. AI-DRIVEN APPROACHES TO PCOS PREVENTION
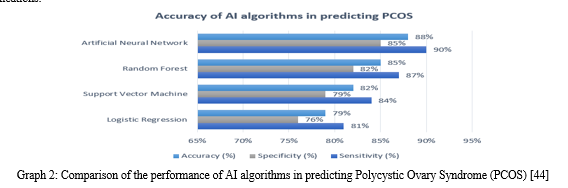
A. Leveraging Machine Learning Algorithms for Data Analysis
The integration of Artificial Intelligence (AI) and machine learning algorithms has completely transformed the way PCOS prevention is approached, allowing for the analysis of extensive and intricate health data [25]. Machine learning algorithms have the ability to analyze extensive datasets, which can include details about hormonal levels, lifestyle factors, and genetic predispositions. Through this analysis, patterns and risk factors related to PCOS [26] can be identified.
B. Analyzing Hormonal Levels, Lifestyle Factors, and Genetic Predispositions
AI-driven approaches to PCOS prevention utilize advanced machine learning algorithms to analyze a diverse set of data points pertaining to an individual's health profile. This involves assessing hormonal levels, like testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), which can be imbalanced in women with PCOS [27]. In addition, lifestyle factors such as diet, physical activity, and stress levels are considered, as they have a significant impact on the development and severity of PCOS [28]. In addition, machine learning algorithms have the ability to integrate genetic data, including single nucleotide polymorphisms (SNPs) linked to PCOS susceptibility, in order to offer a more thorough risk evaluation [29].
C. Identifying Patterns Indicative of Hormonal Imbalances
Through the analysis of intricate relationships between hormonal levels, lifestyle factors, and genetic predispositions, machine learning algorithms have the potential to detect patterns and correlations that could suggest hormonal imbalances linked to PCOS. The algorithms have the ability to identify subtle changes in hormonal profiles that may not be easily noticeable using conventional diagnostic methods. This allows for the possibility of detecting and intervening at an earlier stage [25]. As an illustration, machine learning models have the ability to detect patterns of heightened testosterone levels along with certain lifestyle factors or genetic variations. These patterns could potentially indicate a higher likelihood of developing PCOS [26]. By identifying these patterns at an early stage, healthcare professionals can implement specific prevention strategies, such as lifestyle changes or medication, to reduce the risk of PCOS development and its related complications [28]. The application of AI and machine learning in PCOS prevention shows great potential in enhancing the early detection and personalized management of this intricate disorder. Through the utilization of data analysis and pattern recognition, AI-driven approaches offer valuable insights into the complex nature of PCOS. This empowers healthcare providers to create personalized prevention strategies that are more effective.
V. EARLY DETECTION AND INTERVENTION
AI-driven approaches to PCOS prevention not only facilitate the analysis of complex health data but also enable early detection and intervention. Through the use of machine learning algorithms, healthcare professionals can detect subtle patterns and variations in hormonal profiles that may occur before the appearance of PCOS symptoms [25]. The algorithms have the ability to analyze large volumes of data from different sources, such as electronic health records, wearable devices, and patient-reported outcomes. This enables them to identify potential indicators of hormonal imbalances at an early stage [26].
A. AI's Ability to Identify Subtle Patterns Preceding PCOS Symptoms
AI plays a crucial role in PCOS prevention by effectively detecting subtle patterns and deviations from normal hormonal levels that may go unnoticed with traditional diagnostic methods. Machine learning algorithms have the ability to identify subtle changes in hormone levels, like higher testosterone or insulin resistance, that could suggest a higher likelihood of developing PCOS [27]. By recognizing these patterns at an early stage, healthcare providers have the opportunity to intervene before PCOS symptoms fully develop. This proactive approach may help prevent or reduce the severity of the disorder [25].
B. Enabling Proactive Intervention and Timely Treatment
Early detection of PCOS risk factors through AI-driven approaches enables proactive intervention and timely treatment. By identifying individuals at high risk of developing PCOS, healthcare professionals can implement targeted prevention strategies, such as lifestyle modifications, nutritional interventions, and pharmacological treatments [28]. These proactive measures can help regulate hormonal imbalances, improve insulin sensitivity, and reduce the risk of long-term complications associated with PCOS, such as infertility, type 2 diabetes, and cardiovascular disease [30].
VI. PERSONALIZED PREVENTION STRATEGIES
Utilizing AI-driven methods, PCOS prevention can be enhanced by tailoring prevention strategies to an individual's specific health profile, dietary habits, and lifestyle choices.
A. Considering individual health profiles, dietary habits, and lifestyle Choices
AI algorithms have the ability to analyze various data points concerning an individual's health, such as their medical history, family background, dietary habits, physical activity levels, and stress management practices [25]. By taking into account these factors, AI models can offer a thorough evaluation of an individual's PCOS risk and pinpoint particular areas where interventions may have the greatest impact [28]. For instance, if an AI model recognizes that someone leads a sedentary lifestyle and consumes a diet rich in processed foods, it can suggest specific lifestyle adjustments. These may include incorporating more physical activity and adopting a well-balanced, nutrient-rich diet to lower the risk of PCOS [30].
B. Tailoring Prevention Plans based on AI-driven Insights
By leveraging AI-driven data analysis, healthcare providers can create personalized prevention plans that cater to each person's distinct needs and circumstances. These customized plans may incorporate a variety of lifestyle adjustments, nutritional interventions, stress management techniques, and, if needed, pharmacological treatments [28]. AI algorithms can consistently monitor an individual's progress and adapt the prevention plan based on their response to interventions, ensuring that the strategies remain effective over time [26]. Through the use of personalized, data-driven recommendations, AI-driven approaches to PCOS prevention can enhance outcomes and empower individuals to actively manage their health.
The integration of AI in PCOS prevention signifies a notable breakthrough in the early detection, intervention, and personalized management of this intricate disorder. Through the utilization of machine learning and data analysis, AI-driven methods have the capability to detect intricate patterns, facilitate proactive intervention, and customize prevention strategies to cater to the specific requirements of individuals who are at risk of PCOS.
|
Application |
Description |
|
Risk assessment |
Identifying women at high risk of developing PCOS |
|
Early detection |
Recognizing subtle hormonal changes before overt symptoms |
|
Personalized prevention |
Tailoring prevention strategies based on individual risk factors |
|
Lifestyle management |
Providing AI-driven recommendations for diet, exercise, and stress management |
|
Treatment optimization |
Predicting response to treatments and optimizing interventions |
Table 2: Potential applications of AI in PCOS prevention [31,42]
VII. ADVANTAGES OF AI IN PCOS PREVENTION
A. Analyzing Complex Health Data
One of the key benefits of AI in PCOS prevention is its remarkable capacity to analyze vast amounts of intricate health data with efficiency and precision. AI algorithms have the capability to analyze and understand large volumes of data from different sources, such as electronic health records, wearable devices, and patient-reported outcomes [31]. The algorithms have the ability to identify patterns, correlations, and risk factors that can be challenging for human practitioners to recognize. This allows them to provide valuable insights into the complex nature of PCOS [32]. Through the utilization of AI's advanced data analysis capabilities, healthcare providers can acquire a more holistic comprehension of the factors that contribute to the development of PCOS. This enables them to customize prevention strategies accordingly.
B. Potential for Early Detection of Hormonal Imbalances
AI-driven approaches to PCOS prevention provide the potential for early detection of hormonal imbalances, which plays a crucial role in preventing or reducing the severity of the disorder. Analyze hormonal profiles over time using machine learning algorithms to detect subtle changes or deviations that could indicate an increased risk of PCOS [33]. For instance, AI models have the ability to identify gradual changes in testosterone levels or insulin resistance, which are important signs of PCOS development [34]. Identifying hormonal imbalances early on allows healthcare providers to take prompt action, implementing interventions like lifestyle modifications or pharmacological treatments. This can help prevent or delay the onset of PCOS and its associated complications.
C. Capacity to Develop Personalized Prevention Plans
One notable benefit of AI in PCOS prevention is its ability to create customized prevention plans that take into account an individual's specific health profile, lifestyle factors, and genetic predispositions. AI algorithms have the ability to analyze a diverse set of data points, such as medical history, family background, dietary habits, physical activity levels, and stress management practices, in order to generate a thorough risk assessment [31]. According to these insights, AI has the ability to generate personalized prevention recommendations that cater to an individual's unique needs and circumstances [35]. For instance, if an AI model recognizes that someone has a genetic predisposition to PCOS and a sedentary lifestyle, it can suggest specific interventions like regular exercise and a balanced diet to lower the risk of PCOS. Through the use of personalized, data-driven recommendations, AI has the potential to enhance the effectiveness of PCOS prevention strategies and enhance long-term health outcomes.
D. Empowering women to make Informed Lifestyle Choices
AI-driven approaches to PCOS prevention can empower individuals to make informed lifestyle choices by providing personalized insights and recommendations. Through the utilization of AI's data analysis capabilities, healthcare providers can provide women with a more comprehensive comprehension of their unique risk factors and the measures they can adopt to decrease their likelihood of developing PCOS [32]. Prevention plans generated by AI can provide detailed guidance on nutrition, physical activity, stress management, and other lifestyle factors that have an impact on the risk of PCOS [34]. Empowering women with this knowledge and support enables AI to assist them in taking a proactive role in managing their health and well-being. In addition, AI-driven monitoring and feedback systems can assist women in monitoring their progress, making necessary adjustments to their lifestyle choices, and staying motivated over time. This can ultimately contribute to the long-term success of PCOS prevention efforts [33].
VIII. IMPLICATIONS AND FUTURE DIRECTIONS
A. Significance of AI in Advancing Women's Healthcare
The integration of AI in PCOS prevention has far-reaching implications for advancing women's healthcare as a whole. This application showcases the power of AI-driven approaches in detecting PCOS early, providing personalized prevention strategies, and managing the condition. It sets an example for how AI can be used to tackle other intricate women's health concerns [31]. The success of AI in PCOS prevention emphasizes the significance of utilizing advanced technologies to enhance the comprehension, diagnosis, and treatment of conditions that have a greater impact on women. As AI advances and progresses, it holds the potential to transform women's healthcare by enabling more precise, proactive, and patient-centric approaches to disease prevention and management [36].
B. Potential for AI-driven Prevention Strategies in other Women's Health Issues
The potential benefits of AI-driven prevention strategies in PCOS open up possibilities for implementing similar approaches in addressing other women's health concerns. Several conditions that impact women, such as endometriosis, uterine fibroids, and breast cancer, face similar obstacles as PCOS, including intricate causes, varied symptoms, and the importance of timely identification and tailored treatments [37]. AI-driven methods can be utilized to analyze the distinct risk factors, biomarkers, and clinical features linked to these conditions, facilitating the creation of focused prevention strategies [31]. Through the use of AI's powerful data processing capabilities and its knack for recognizing intricate patterns, healthcare providers have the potential to enhance the timely identification and prevention of various women's health concerns. This, in turn, can lead to improved health outcomes and an enhanced quality of life for women across the globe [38].
C. Ethical Considerations and Data Privacy Concerns
Although the integration of AI in PCOS prevention brings about various advantages, it also gives rise to significant ethical considerations and concerns regarding data privacy. The development and implementation of AI-driven approaches heavily depend on the collection, storage, and analysis of sensitive personal health information [36]. It is crucial to prioritize the privacy, security, and confidentiality of this data in order to uphold patient trust and safeguard individual rights [39]. In addition, the utilization of AI in healthcare decision-making raises concerns regarding algorithmic bias, transparency, and accountability [31]. Developing robust ethical frameworks and governance mechanisms is crucial for guiding the responsible use of AI in women's healthcare. It is important to ensure that these technologies are deployed in a fair, unbiased, and transparent manner [38].
D. Collaboration Between AI experts and Healthcare Professionals
In order to fully harness the power of AI in preventing PCOS and advancing women's healthcare, it is crucial for AI experts and healthcare professionals to work closely together. To develop effective AI-driven prevention strategies, a thorough understanding of the clinical complexities of PCOS and other women's health issues, along with expertise in AI technologies and data science, is crucial [37]. Through fostering interdisciplinary partnerships, healthcare organizations can ensure that AI solutions are clinically relevant, aligned with patient needs, and seamlessly integrated into existing care pathways [39]. In addition, collaboration fosters the sharing of knowledge and best practices, allowing for the ongoing improvement and optimization of AI-driven approaches [31]. In order to drive innovation, improve patient outcomes, and shape the future of women's health, ongoing collaboration between AI experts and healthcare professionals is crucial in the evolving field of AI in women's healthcare [36].
Conclusion
The incorporation of Artificial Intelligence in the prevention of Polycystic Ovary Syndrome signifies a noteworthy achievement in the progression of women\'s healthcare. Through the utilization of AI, healthcare providers can effectively analyze intricate health data, detect potential indicators in advance, and create tailored prevention methods. This proactive approach enables providers to tackle the obstacles presented by PCOS and enhance the overall health outcomes for women affected by this condition. Looking ahead, the ongoing partnership between AI experts and healthcare professionals, along with a steadfast dedication to ethical considerations and data privacy, will play a pivotal role in fostering innovation and shaping the trajectory of women\'s health. Looking ahead, the ongoing partnership between AI experts and healthcare professionals, along with a steadfast dedication to ethical considerations and data privacy, will play a vital role in fostering innovation and shaping the trajectory of women\'s health. By fully embracing the capabilities of AI and harnessing its potential to address a variety of women\'s health concerns, we can empower women to proactively manage their well-being, make informed decisions about their lifestyle, and ultimately enhance their overall quality of life.
References
[1] Bozdag, G., Mumusoglu, S., Zengin, D., Karabulut, E., & Yildiz, B. O. (2016). The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-analysis. Human Reproduction, 31(12), 2841-2855. [2] Jiang, F., Jiang, Y., Zhi, H., Dong, Y., Li, H., Ma, S., ... & Wang, Y. (2017). Artificial intelligence in healthcare: Past, present, and future. Stroke and Vascular Neurology, 2(4), 230-243. [3] Kuhn, E., & Moodie, E. E. (2021). Machine learning for personalized medicine: Will this drug give me a heart attack? Statistics in Medicine, 40(3), 497-511. [4] Chen, Y., & Hao, Y. (2020). Integrating machine learning and physiology based modeling for personalized medicine. Journal of Applied Physiology, 128(4), 887-892. [5] Szymanska, E., Saccenti, E., Smilde, A. K., & Westerhuis, J. A. (2012). Double-check: Validation of diagnostic statistics for PLS-DA models in metabolomics studies. Metabolomics, 8(1), 3-16. [6] Lisboa, P. J., & Taktak, A. F. (2006). The use of artificial neural networks in decision support in cancer: A systematic review. Neural Networks, 19(4), 408-415. [7] Zhang, Y., & Zhao, Y. (2019). Automated machine learning techniques for data science and analytics. Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery, 9(6), e1326. [8] Cirillo, D., & Valencia, A. (2019). Big data analytics for personalized medicine. Current Opinion in Biotechnology, 58, 161-167. [9] Bozdag, G., Mumusoglu, S., Zengin, D., Karabulut, E., & Yildiz, B. O. (2016). The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-analysis. Human Reproduction, 31(12), 2841-2855. [10] Azziz, R., Carmina, E., Chen, Z., Dunaif, A., Laven, J. S., Legro, R. S., ... & Yildiz, B. O. (2016). Polycystic ovary syndrome. Nature Reviews Disease Primers, 2(1), 1-18. [11] Kakoly, N. S., Khomami, M. B., Joham, A. E., Cooray, S. D., Misso, M. L., Norman, R. J., ... & Moran, L. J. (2019). Ethnicity, obesity and the prevalence of impaired glucose tolerance and type 2 diabetes in PCOS: A systematic review and meta-regression. Human Reproduction Update, 25(4), 455-467. [12] Escobar-Morreale, H. F. (2018). Polycystic ovary syndrome: Definition, aetiology, diagnosis and treatment. Nature Reviews Endocrinology, 14(5), 270-284. [13] Jiang, F., Jiang, Y., Zhi, H., Dong, Y., Li, H., Ma, S., ... & Wang, Y. (2017). Artificial intelligence in healthcare: Past, present, and future. Stroke and Vascular Neurology, 2(4), 230-243. [14] Bozdag, G., Mumusoglu, S., Zengin, D., Karabulut, E., & Yildiz, B. O. (2016). The prevalence and phenotypic features of polycystic ovary syndrome: A systematic review and meta-analysis. Human Reproduction, 31(12), 2841-2855. [15] Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. (2004). Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertility and Sterility, 81(1), 19-25. [16] Ding, T., Hardiman, P. J., Petersen, I., Wang, F. F., Qu, F., & Baio, G. (2017). The prevalence of polycystic ovary syndrome in reproductive-aged women of different ethnicity: A systematic review and meta-analysis. Oncotarget, 8(56), 96351-96358. [17] Azziz, R., Carmina, E., Dewailly, D., Diamanti-Kandarakis, E., Escobar-Morreale, H. F., Futterweit, W., ... & Witchel, S. F. (2006). Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. The Journal of Clinical Endocrinology & Metabolism, 91(11), 4237-4245. [18] Diamanti-Kandarakis, E., & Dunaif, A. (2012). Insulin resistance and the polycystic ovary syndrome revisited: An update on mechanisms and implications. Endocrine Reviews, 33(6), 981-1030. [19] Balen, A. H., Conway, G. S., Kaltsas, G., Techatraisak, K., Manning, P. J., West, C., & Jacobs, H. S. (1995). Polycystic ovary syndrome: The spectrum of the disorder in 1741 patients. Human Reproduction, 10(8), 2107-2111. [20] Joham, A. E., Teede, H. J., Ranasinha, S., Zoungas, S., & Boyle, J. (2015). Prevalence of infertility and use of fertility treatment in women with polycystic ovary syndrome: Data from a large community-based cohort study. Journal of Women\'s Health, 24(4), 299-307. [21] Fauser, B. C., Tarlatzis, B. C., Rebar, R. W., Legro, R. S., Balen, A. H., Lobo, R., ... & Barnhart, K. (2012). Consensus on women\'s health aspects of polycystic ovary syndrome (PCOS): The Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertility and Sterility, 97(1), 28-38. [22] Moran, L. J., Misso, M. L., Wild, R. A., & Norman, R. J. (2010). Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: A systematic review and meta-analysis. Human Reproduction Update, 16(4), 347-363. [23] Wild, R. A., Carmina, E., Diamanti-Kandarakis, E., Dokras, A., Escobar-Morreale, H. F., Futterweit, W., ... & Dumesic, D. A. (2010). Assessment of cardiovascular risk and prevention of cardiovascular disease in women with the polycystic ovary syndrome: A consensus statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. The Journal of Clinical Endocrinology & Metabolism, 95(5), 2038-2049. [24] Veltman-Verhulst, S. M., Boivin, J., Eijkemans, M. J., & Fauser, B. J. (2012). Emotional distress is a common risk in women with polycystic ovary syndrome: A systematic review and meta-analysis of 28 studies. Human Reproduction Update, 18(6), 638-651. [25] Sirmans, S. M., Parish, R. C., Blake, S., & Wang, X. (2014). Epidemiology and comorbidities of polycystic ovary syndrome in an indigent population. Journal of Investigative Medicine, 62(6), 868-874. [26] Thathapudi, S., Kodati, V., Erukkambattu, J., Katragadda, A., Addepally, U., & Hasan, Q. (2015). Anthropometric and biochemical characteristics of polycystic ovarian syndrome in South Indian women using AES-2006 criteria. International Journal of Endocrinology and Metabolism, 13(1), e12470. [27] Diamanti-Kandarakis, E., & Dunaif, A. (2012). Insulin resistance and the polycystic ovary syndrome revisited: An update on mechanisms and implications. Endocrine Reviews, 33(6), 981-1030. [28] Moran, L. J., Hutchison, S. K., Norman, R. J., & Teede, H. J. (2011). Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database of Systematic Reviews, (7), CD007506. [29] Chen, Z. J., Zhao, H., He, L., Shi, Y., Qin, Y., Shi, Y., ... & Zhao, Y. (2011). Genome-wide association study identifies susceptibility loci for polycystic ovary syndrome on chromosome 2p16.3, 2p21 and 9q33.3. Nature Genetics, 43(1), 55-59. [30] Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., ... & Norman, R. J. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction, 33(9), 1602-1618. [31] Tay, C. T., Moran, L. J., Wijeyaratne, C. N., Redman, L. M., Norman, R. J., Teede, H. J., & Joham, A. E. (2019). Integrated model of care for polycystic ovary syndrome. Seminars in Reproductive Medicine, 37(1), 42-56. [32] Zeng, X., Xie, Y. J., Liu, Y. T., Long, S. L., & Mo, Z. C. (2020). Polycystic ovarian syndrome: Correlation between hyperandrogenism, insulin resistance, and obesity. Clinica Chimica Acta, 502, 214-221. [33] Desai, K., Mistry, N., Baghal, S., Mehta, M., Agrawal, A., Radhakrishnan, G., & Nimbkar, S. (2022). Metabolomic signature of polycystic ovary syndrome: A potential tool for early diagnosis and personalized treatment. Frontiers in Endocrinology, 13, 909. [34] Mani, H., Davies, M. J., Bodicoat, D. H., Levy, M. J., Gray, L. J., Howlett, T. A., & Khunti, K. (2015). Clinical characteristics of polycystic ovary syndrome: Investigating differences in White and South Asian women. Clinical Endocrinology, 83(4), 542-549. [35] Li, L., Feng, Q., Ye, M., He, Y., Yao, A., & Shi, K. (2020). Metabolic effect of obesity on polycystic ovary syndrome in adolescents: A meta-analysis. Journal of Obstetrics and Gynaecology, 40(7), 947-953. [36] Bickmore, T. W., Trinh, H., Olafsson, S., O\'Leary, T. K., Asadi, R., Rickles, N. M., & Cruz, R. (2018). Patient and consumer safety risks when using conversational assistants for medical information: An observational study of Siri, Alexa, and Google Assistant. Journal of Medical Internet Research, 20(9), e11510. [37] Noorbakhsh-Sabet, N., Zand, R., Zhang, Y., & Abedi, V. (2019). Artificial intelligence transforms the future of healthcare. The American Journal of Medicine, 132(7), 795-801. [38] Geis, J. R., Brady, A. P., Wu, C. C., Spencer, J., Ranschaert, E., Jaremko, J. L., ... & Kohli, M. (2019). Ethics of artificial intelligence in radiology: Summary of the joint European and North American multisociety statement. Radiology, 293(2), 436-440 Panesar, A. (2019). Machine learning and AI for healthcare: Big data for improved health outcomes. Apress. [39] Panesar, A. (2019). Machine learning and AI for healthcare: Big data for improved health outcomes. Apress. [40] Kakoly, N. S., Khomami, M. B., Joham, A. E., Cooray, S. D., Misso, M. L., Norman, R. J., ... & Moran, L. J. (2019). Ethnicity, obesity and the prevalence of impaired glucose tolerance and type 2 diabetes in PCOS: A systematic review and meta-regression. Human Reproduction Update, 25(4), 455-467. [41] Rutkowska, A. Z., & Diamanti-Kandarakis, E. (2016). Polycystic ovary syndrome and environmental toxins. Fertility and Sterility, 106(4), 948-958. [42] Kumarendran, B., Sumilo, D., O\'Reilly, M. W., Toulis, K. A., Gokhale, K., Wijeyaratne, C. N., ... & Nirantharakumar, K. (2021). Polycystic ovary syndrome and severe cardiometabolic outcomes: An observational and Mendelian randomisation study. Clinical Endocrinology, 95(1), 32-43. [43] Lizneva, D., Suturina, L., Walker, W., Brakta, S., Gavrilova-Jordan, L., & Azziz, R. (2016). Criteria, prevalence, and phenotypes of polycystic ovary syndrome. Fertility and Sterility, 106(1), 6-15. [44] Jia, L., Li, J., Zhao, Q., Feng, S., & Wang, X. (2021). Artificial intelligence-based approaches for the diagnosis of polycystic ovary syndrome: A systematic review and meta-analysis. Frontiers in Endocrinology, 12, 642712.
Copyright
Copyright © 2024 Karthik Chowdary Tsaliki. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET61001
Publish Date : 2024-04-25
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

