Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Information-Technology in Healthcare
Authors: Dr. Anupriya Jain, Kumkum Sharma, Alisha Singh, Melbin Kurien
DOI Link: https://doi.org/10.22214/ijraset.2023.55180
Certificate: View Certificate
Abstract
Healthcare changes dramatically because of technological developments, from aesthetics and antibiotics to magnetic resonance imaging scanners and radiotherapy. Future technological innovation is going to keep transforming healthcare, yet while technologies (new drugs and treatments, new devices, new social media support for healthcare, etc) will drive innovation, human factors will remain one of the stable limitations of breakthroughs. No predictions can satisfy everybody; instead, this article explores fragments of the future to see how to think more clearly about how to get where we want to go. Significance for public health technology drives healthcare more than any other force, and in the future, it will continue to develop in dramatic ways. While we can glimpse and debate the details of future trends in healthcare, we need to be clear about the drivers so we can align with them and actively work to ensure the best outcomes for society as a whole.
Introduction
I. INTRODUCTION
Pluck a nurse and surgeon out of the nineteenth century and transport them into a modern 21st-century hospital and it would be a thoroughly recognizable place, with the same hierarchies and strict cultures. Patients are treated as helpless, stripped of their clothes and possessions, lying in beds, and almost completely ignorant of their illness. They might be disappointed in our treatment, particularly of old people, but I don’t think it would surprise them.

If our two time-travellers were able to attend a post-mortem and listen in on a discussion of human error, very little would seem novel. Clinicians would still be in denial, lawyers would still be hovering, and the delay and deny culture would be no surprise. However, the changes that would surprise the nurse and surgeon are all changes to technology. Infusion pumps, dialysis machines, antibiotics, heart valves, MRI scanners, even hand washing stations would be new ideas. All the hidden technology used in the laboratories behind the scenes, from path labs to decontamination, would be startlingly new if it was noticed.

Although the medical culture is similar, there have been dramatic technological changes, and actually these changes would be hard to explain. Does anybody even know how an infusion pump works? They used to be clockwork (and before that, gravity fed) and now almost everything contains a computer and has a colourful screen and lots of buttons. Implanted defibrillators that use telephone networks and web sites to keep cardiologists up to date with their patients are just magic; new pharmaceuticals that change moods, change blood pressure, or kill bacteria: all are modern magic. On reflection, given the centuries of stability, it is amazing how much healthcare has changed in the last 150 years – and one wonders how this accelerating pace of change will proceed in the future.
Health IT (health information technology) is the area of IT involving the design, development, creation, use, and maintenance of information systems for the healthcare industry. Automated and interoperable healthcare information systems will continue to improve medical care and public health, lower costs, increase efficiency, reduce errors and improve patient satisfaction, while also optimizing reimbursement for ambulatory and inpatient healthcare providers.
Today, the importance of health IT results from the combination of evolving technology and changing government policies that influence the quality of patient care. Modern health IT received a boost when President George W. Bush introduced incentives for hospitals to adopt electronic health record (EHR) systems, and that march has continued with Presidents Barack Obama and Donald Trump, showing that health IT enjoys general bipartisan support.
II. PRINCIPLES OF IT IN HEALTHCARE

In the younger records of IT, researchers and doctors with inside the area have accrued and hooked up simple ideas for true IT in healthcare layout in hopes of accomplishing a number of the principal objectives (As a whole).
Ideas are general, essential, and commonsensical, relevant to nearly any Healthcare layout state of affairs. Here, is a quick evaluation of the principle of IT in healthcare: -
A. Autonomy
The philosophical underpinning for autonomy, as interpreted by philosophers Immanuel Kant (1724– 1804) and John Stuart Mill (1806–1873), and accepted as an ethical principle, is that all persons have intrinsic and unconditional worth, and therefore, should have the power to make rational decisions and moral choices, and each should be allowed to exercise his or her capacity for self-determination. This ethical principle was affirmed in a court decision by Justice Cardozo in 1914 with the epigrammatic dictum, “Every human being of adult years and sound mind has a right to determine what shall be done with his own body”.
The principle of autonomy does not extend to persons who lack the capacity (competence) to act autonomously; examples include infants and children and incompetence due to developmental, mental or physical disorder. Health-care institutions and state governments in the US have policies and procedures to assess incompetence. However, a rigid distinction between incapacity to make health-care decisions (assessed by health professionals) and incompetence (determined by court of law) is not of practical use, as a clinician’s determination of a patient’s lack of decision-making capacity based on physical or mental disorder has the same practical consequences as a legal determination of incompetence.
Respecting the principle of autonomy obliges the physician to disclose medical information and treatment options that are necessary for the patient to exercise self-determination and supports informed consent, truth-telling, and confidentiality.
B. Beneficence
The principle of beneficence is the obligation of physician to act for the benefit of the patient and supports a number of moral rules to protect and defend the right of others, prevent harm, remove conditions that will cause harm, help persons with disabilities, and rescue persons in danger. It is worth emphasizing that, in distinction to nonmaleficence, the language here is one of positive requirements. The principle calls for not just avoiding harm, but also to benefit patients and to promote their welfare. While physicians’ beneficence conforms to moral rules, and is altruistic, it is also true that in many instances it can be considered a payback for the debt to society for education (often subsidized by governments), ranks and privileges, and to the patients themselves (learning and research).
C. Nonmaleficence
Nonmaleficence is the obligation of a physician not to harm the patient. This simply stated principle supports several moral rules – do not kill, do not cause pain or suffering, do not incapacitate, do not cause offense, and do not deprive others of the goods of life. The practical application of nonmaleficence is for the physician to weigh the benefits against burdens of all interventions and treatments, to eschew those that are inappropriately burdensome, and to choose the best course of action for the patient. This is particularly important and pertinent in difficult end-of-life care decisions on withholding and withdrawing life-sustaining treatment, medically administered nutrition and hydration, and in pain and other symptom control. A physician’s obligation and intention to relieve the suffering (e.g., refractory pain or dyspnoea) of a patient by the use of appropriate drugs including opioids override the foreseen but unintended harmful effects or outcome (doctrine of double effect).
D. Justice
Justice is generally interpreted as fair, equitable, and appropriate treatment of persons. Of the several categories of justice, the one that is most pertinent to clinical ethics is distributive justice. Distributive justice refers to the fair, equitable, and appropriate distribution of healthcare resources determined by justified norms that structure the terms of social cooperation. How can this be accomplished? There are different valid principles of distributive justice. These are distributed to each person:-
- An equal share,
- According to need,
- According to the effort,
- According to the contribution,
- According to merit, and
- According to free-market exchanges.
Each principle is not exclusive, and can be, and are often combined in the application. It is easy to see the difficulty in choosing, balancing, and refining these principles to form a coherent and workable solution to distribute medical resources.
Although this weighty health-care policy discussion exceeds the scope of this review, a few examples on issues of distributive justice encountered in hospital and office practice need to be mentioned. These include allotment of scarce resources (equipment, tests, medications, organ transplants), care of uninsured patients, and allotment of time for outpatient visits (equal time for every patient? based on need or complexity? based on social and or economic status?). Difficult as it may be, and despite the many constraining forces, physicians must accept the requirement of fairness contained in this principle. Fairness to the patient assumes a role of primary importance when there are conflicts of interests. A flagrant example of violation of this principle would be when a particular option of treatment is chosen over others, or an expensive drug is chosen over an equally effective but less expensive one because it benefits the physician, financially, or otherwise.
III. TYPES OF HEALTH IT
The use of technology is revolutionizing the healthcare industry. Not all may realize its importance now, but there has been accelerated development and evidence about the impact of health information technology on patient care.
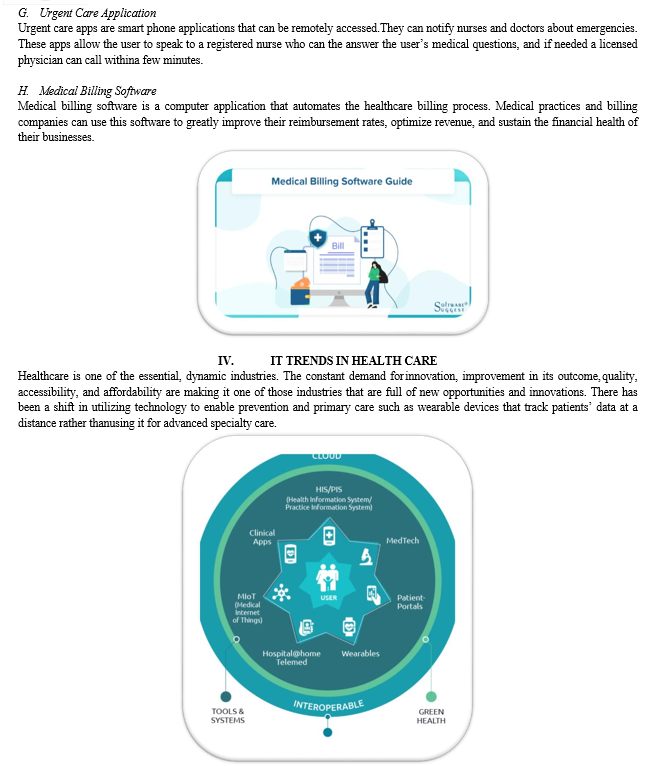
There are many categories of the health information system, and most of them share similar capabilities. Healthcare information technology can provide a seamless experience for all patients as well as practitioners.
Health information technology, or HIT, refers to a system designed to store, share, and analyse the data collected in any healthcare facility. It could be private as well as public clinics, hospitals, and doctor’s private chambers. It also collects, organizes, and manages patients’ electronic medical records.
The use of healthcare software can help improve the quality of patient treatment.
There are different types of healthcare information systems that take care of administerial aspects and patients’ medical data, amongst many other things.
Clearly, a healthcare system has a lot of benefits to offer by increasing the effectiveness of a healthcare institute. For instance, it ensures the accuracy of data collected and thus reduces any chance of medical error.
Not only that, but it saves time and effort, which is spent daily on managerial tasks by streamlining operations. Thus, organizations can focus more on patient treatment and follow-up. Other than that, you get faster prescriptions and reduces paperwork as well.
These were just a few of the examples of how healthcare systems are transforming the patient care industry. You can choose the type of information technology in healthcare systems required depending on your organization’s model and specific needs. Let’s discuss them in detail.
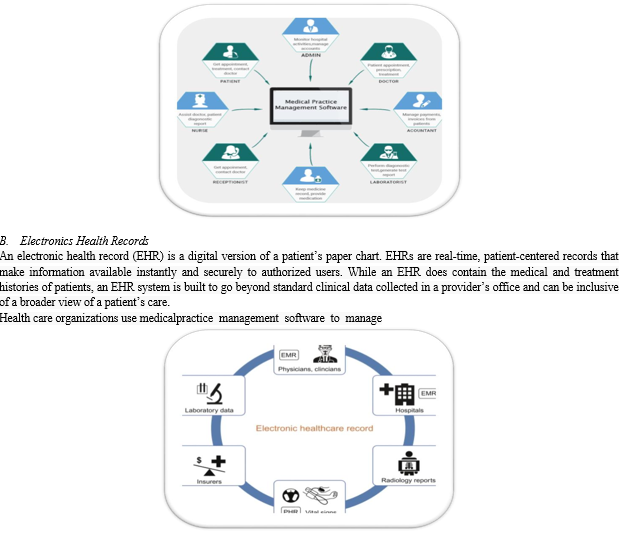
A. Medical Practise System Management
All aspects of their operations, including patient information management, treatment planning and scheduling, and back office functions such as accounting. This type of software helps doctors with patient treatment management, and healthcare administrative personnel with patient influx management. Scaled down versions of medical practice management can address the needs of small clinics or private practices.

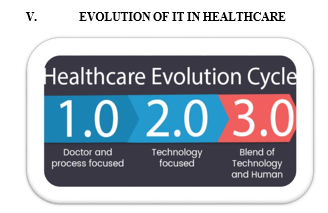
A. Rapid Change Through Telehealth
Telehealth has been evolving over the past few years and rightly so as it can aid urgent care facilities to a great extent. At a time of emergency, telehealth can follow up and treat many patients at a distance.
Telehealth is expected to rise from $79.79 billion in 2020 to $396.76 billion in 2027, according to forecasts. This number is 38 times larger than it was before the COVID 19.
Telehealth is extremely efficient in saving the time and stress of both the physician and the patients. Doctors can follow up with the patients virtually, which reduces the strain of last-minute appointments.
B. Digital Health to Rescue
Digital health is gradually occupying a significant position in our daily lives, making it a worthy tool in medical device trends for 2022.
The worldwide digital health industry was valued at $96.5 billion in 2020 and is expected to increase at a 15.1 percent compound annual growth rate (CAGR) from 2021 to 2028.
From 2021 to 2028, the global wearable sensors market is estimated to grow at a CAGR of 29.3%, from USD 660.89 million in 2020 to USD 5,208.05 million in 2028.
C. Improvement in data science and Predictive Analytics
The healthcare predictive analytics market is estimated to grow from $3.74 billion in 2019 to $28.77 billion by 2027.
Compressing all the data generated from patients suffering from chronic ailments can be challenging. Nonetheless, rapid improvement in data science and predictive analysis has given doctors access to deeper insights like gathering information about ancestry and family history, detecting patients with high risks to diagnose problems effectively.
Congeal ensures that doctors can easily access, monitor, and intervene in patients’ progress at a click of a button by providing patients’ real-time reports available to them.
D. Impact of Artificial Intelligence
Healthcare is significantly impacted by the revolution brought about by artificial intelligence technology. There is no doubt that AI will rule future trends in healthcare since it has improved diagnostic precision through automatic assistance in the workforce, clinical operation optimization, quantitative imaging, etc.
E. The Cybersecurity Mesh
The Cybersecurity Mesh uses a zero-trust network model to operate. It emphasizes the importance of no device trusting and allowing access to the broader network. Previously, with Perimeter-focused security, it was discovered that more than 34% of data was exposed to leaks and breaches within the network itself. Many companies are hoping for better cyber security with The Cybersecurity mesh. Some research anticipated that this security architecture would be able to reduce the financial impact of a security incident by 90%.
F. Cloud Computing
By delivering on-demand healthcare storage, cloud computing in healthcare lowers capital and operational expenses. It increases the efficiency of the industry while cutting costs. Cloud computing makes it easy to share medical records, automate backend operations, and even create and maintain telehealth apps.
The healthcare cloud computing business is expected to expand to USD 64.7 billion by 2025, up from USD 28.1 billion in 2020. Cloud computing enables high-powered analytics for more customized patient care plans using EMRs stored in the cloud. Cognihab helps to restore important data with help of cloud computing.
G. Block chain
The block chain system will generate identical blocks whenever a linked device is involved in any form of transaction. When data on one computer is accessed, edited, shared, or otherwise processed in any way, a block is formed on all devices to record the information locally.
The global block chain technology in the healthcare market is expected to develop at a compound annual growth rate of 21.70 percent from 2021 to 2028.
The medical industry has been severely harmed by the inability to securely share and access sensitive patient data. However, for true interoperability, block chain will provide highly flexible openness while adhering to the strictest security standards.
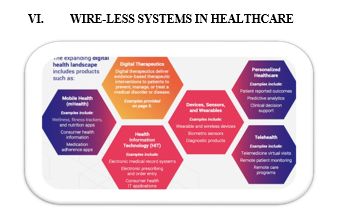
Gone are the days when the delivery of healthcare was confined to the four walls of a hospital. Mayo Clinic is launching its own “hospital at home” model and has autonomous vehicles delivering Covid-19 tests. Maccabi Healthcare Services in Israel plans to deploy an AI system that can identify people at risk of developing Covid- 19 complications. Simply put, the “hospital of tomorrow” will look quite different than the one to which we’re all accustomed.
Until now, the transition has been somewhat gradual — a shift to value-based payment, a renewed focus on patient outcomes rather than volume — but the Covid-19 pandemic has both amplified the gaps in hospital-delivered care and sped up innovation to find better, more efficient, mechanisms to deliver quality care.
The virtually overnight pivot to telemedicine in response to the pandemic has shown us that much of our healthcare can be managed remotely. For many patients, it’s not only more convenient, it’s safer to avoid physically going to a hospital environment for general checkups. Even before Covid-19, the Centres for Disease Control and Prevention (CDC) estimate there are 1.7 million hospital- acquired infections annually, which lead to 99,000 deaths. There’s little data currently available about hospital-acquired COVID infections here in the U.S., but one estimate from the U.K. cited as much as 20% of cases were hospital-acquired.
There will always be a need for in-hospital care as we think of it today. No one’s going to receive ED-level or trauma care via video call. But to understand where we’re headed and why, it’s important to first consider the factors driving changes in how healthcare is delivered. How we think about healthcare will need to evolve in order to deliver better care at a much lower cost.


Hospitals as a physical entity will change — they’ll look different. Sure, there will be more care delivery in a patient’s home. But there will also be care outside the home: the corner pharmacy taking on a bigger role or assisted living (another segment of healthcare ripe for transformation). Another avenue is self-service point of care — think of Amazon delivering at-home Covid-19 test kits directly to consumers.
We also need to embrace new ways to consume healthcare and payers need to incentivize and compensate healthcare providers to leverage technology. As Covid-19 reduced or eliminated elective procedures, routine visits and other bread- and-butter revenue streams have been slashed. Healthcare systems aiming to keep people out of hospitals, clinics and physicians’ offices, opened the doors for telehealth like never before. A friend of mine who is a physician went from seeing 10 to 15 patients a day in the office to 100% remote virtually overnight.
It took all three stakeholders to change: Patients, providers and payers to all had to adapt quickly to leverage existing technology, change workflows, and adopt new billing procedures. So far, it seems to work.
We will continue to see new practice models emerge and we can expect routine visits via telehealth to continue. And this is good news for entrepreneurs and investors. The government kick-started the digital health trend when it invested billions of dollars in the necessary infrastructure to fuel digital health during a push for electronic medical record adoption across the country. Now, the digital backbone is falling into place for connected medical devices and healthcare IT to connect everything together. Devices and services that enable remote monitoring, remote control, data analytics — technology that enables the delivery of care in diverse settings — will drive the next wave of innovation beyond the needs of the current pandemic.
If the injury and situation is serious enough, people will continue to go to the hospital. But if you just need blood drawn, do you really need to go to a hospital or your local lab? Wouldn’t it be easier on you (and less costly to everyone) if you could just prick your finger at your kitchen table and send in your blood sample? Do you really need to physically see your physician for a routine question you could ask via a secure messaging system or video chat?
Providing affordable and effective care is imperative to help solve healthcare’s trillion-dollar problem. Technology has improved our lives in countless ways — it’s time healthcare reaps the reward. Lives, and our economy, depend on it.
The system then traces each individual's movement around a digital floor plan. Matching these movement patterns with other data can provide insights about how people interact with each other and the environment.
In one assisted living facility, with permission from the patient's family and caregivers, the researchers monitored a patient with dementia who would often become agitated for unknown reasons. Over a month, they measured the patient's increased pacing between areas of their unit
- a known sign of agitation. By matching increased pacing with the visitor log, they determined the patient was agitated more during the days following family visits. This shows Marko can provide a new, passive way to track functional health profiles of patients at home, the researchers say.
"These are interesting bits we discovered through data," says first author Chen-Yu Hsu, a PhD student in the Computer Science and Artificial Intelligence Laboratory (CSAIL). "We live in a sea of wireless signals, and the way we move and walk around changes these reflections. We developed the system that listens to those reflections ... to better understand people's behaviour and health."
A convolutional neural network - a machine-learning model commonly used for image processing - uses those tracklets to separate reflections by certain individuals. For each individual its senses, the system creates two "filtering masks," which are small circles around the individual. These masks basically filter out all signals outside the circle, which locks in the individual's trajectory and height as they move. Combining all this information - height, build, and movement - the network associates specific RF reflections with specific individuals.
The researchers hope health care facilities will use Marko to passively monitor, say, how patients interact with family and caregivers, and whether patients receive medications on time. In an assisted living facility, for instance, the researchers noted specific times a nurse would walk to a medicine cabinet in a patient's room and then to the patient's bed. That indicated that the nurse had, at those specific times, administered the patient's medication.
The system may also replace questionnaires and diaries currently used by psychologists or behavioural scientists to capture data on their study subjects' family dynamics, daily schedules, or sleeping patterns, among other behaviours. Those traditional recording methods can be inaccurate, contain bias, and aren't well-suited for long- term studies, where people may have to recall what they did days or weeks ago. Some researchers have started equipping people with wearable sensors to monitor movement and biometrics. But elderly patients, especially, often forget to wear or charge them. "The motivation here is to design better tools for researchers," Hsu says.
VII. HEALTHCARE IT TODAY
- EHRs still need work— the primary complaint by physicians is that poorly designed EHR interfaces are confusing and more time consuming than paper.
- Actionable insights from data — Healthcare organizations are investing in data tools to lower costs, improve care outcomes and comply with value-based mandates.
- Cloud adoption — Healthcare organizations are shifting from data centres to cloud based computing. The goal is to lower the cost of data storage and enhance the ability to share healthcare data within departments and among other entities.
- Internet of Things (IoT) healthcare devices — connected devices are improving real-time data availability and information sharing. But IoT devices are targeted by hackers and the technology still has some maturing to do.
- Accessing unstructured data — EHRs have been structuring data but healthcare organizations have been turning to platforms that support and enable access to unstructured data too.
- Automating healthcare administration — while much of the focus has been on technology use by the clinical side of healthcare, major administrative functions of healthcare — such as hospital billing, financial applications and physician billing — have been automated.
- Technology driven innovation — Emerging opportunities in healthcare innovation mostly have driven by “the availability of large-scale databases; the development of true relational database software; and the emergence of the Internet into the commercial marketplace.” These technological advancements are expected to drive innovation in reducing medical errors, computerized physician data entry (CPDE) and disease management.
- Healthcare organizations are expected to spend $1.5 trillion on technology in 2018. HIT budgets likely will reflect priorities affected by several infrastructure trends in 2018 such as:
- Pace of IT — Market conditions and technology change much more quickly. Long-term plans quickly become outdated.
- Application programing interfaces (APIs) —Healthcare organizations cautiously approach migration to cloud services. Once they do adopt cloud services, HIT departments continuously need to assess how much they’re using and how much it costs.
- Flexible infrastructures — historically, networks have been too complex to adapt quickly to new device connections and increases in workload. Networks are needed that adapt to business needs.
- Application programing interfaces (APIs) — HIT departments are working with APIs to ensure systems can share data and work.
- Customer satisfaction — While HIT departments see themselves as responsible for serving internal staff members, they are realizing how their work influences the customer experience and satisfaction with the healthcare organization.
VIII. FUTURE WORK
It took us a century to go from scribbled notes to the ability to access medical information on hand-held devices and cell phones. But consider that almost 75 percent of all communication among healthcare organizations happens via fax machines. Unbelievable.
The future, like the past, will be driven by everyone with a stake in today’s healthcare industry.
- Payers and government regulators want total portability of health data among patients, physicians, hospital systems and healthcare payers.
- Clinicians want more intuitive EHR interfaces that take less time to enter patient data.
- Patients are using consumer medical devices that collects health data.
- Clinicians want access on any device, anywhere, and at any time.
The future of healthcare is shaping up in front of our very eyes with advances in digital healthcare technologies, including 3D printing, Remote diagnosis, Wearables, Electoceuticals, Digital therapeutics, Virtual Reality (VR), and Augmented Reality, Artificial Intelligence (AI), Computer vision, etc. Health-tech start-ups are incorporate these digital technologies in bringing the future to the present and help millions of patients. The most significant disruption in healthcare is the convergence of these multiple technologies, which exponentially amplifies the impact.
The pandemic undoubtedly accelerated technological advancement and adoption in healthcare. It’s now easier and faster for patients to procure medical services outside of the traditional four walls of the medical establishment, enhancing convenience and accessibility for all. Telehealth has made it possible for patients to receive care without an in-person office visit. In addition, remote patient monitoring is becoming more widely accepted. Having exponentially grown in popularity throughout the pandemic, this now includes wearable technology with impressive capabilities, from remote monitoring of vitals to remote echocardiograms. If not for the pandemic, it probably would have taken the healthcare industry another decade to reach where it is today.
The future of AI in health care could include tasks that range from simple to complex— everything from answering the phone to medical record review, population health trending and analytics, therapeutic drug and device design, reading radiology images, making clinical diagnoses and treatment plans, and even talking with patients. The future of artificial intelligence in health care presents:
- A health care-oriented overview of artificial intelligence (AI), natural language processing (NLP), and machine learning (ML)
- Current and future applications in health care and the impact on patients, clinicians, and the pharmaceutical industry
- A look at how the future of AI in health care might unfold as these technologies impact the practice of medicine and health care over the next decade.
Conclusion
In conclusion, the use of information technology in the healthcare sector is expanding at rapid rate. However, there are so many challenges being experienced by healthcare providers as they endeavour to implement information technology applications. For instance, the quality achieved as a result of investing in information technology is not often rewarded. Instead of rewarding improved service delivery, a majority of service providers put emphasis on the volume of services offered. Another challenge is the healthcare delivery fragmented nature which makes it harder for healthcare organizations to adopt information technology. Regardless these challenges, hospitals are investing in information technology because it enhances information access by patients and healthcare professionals which in turn enhances the quality of care provided to patients. The use of information technology also improves communication between healthcare professionals and consequently reduces missed care. In conclusion, the use of information technology in the healthcare sector is expanding at a rapid rate. However, there are so many challenges being experienced by healthcare providers as they endeavour to implement information technology applications. For instance, the quality achieved as a result of investing in information technology is not often rewarded. Instead of rewarding improved service delivery, a majority of service providers put emphasis on the volume of services offered. Another challenge is the healthcare delivery fragmented nature which makes it harder for healthcare organizations to adopt information technology. Regardless these challenges, hospitals are investing in information technology because it enhances information access by patients and healthcare professionals which in turn enhances the quality of care provided to patients. The use of information technology also improves communication between healthcare professionals and consequently reduces missed care. The study is relevant because it provides healthcare organizations and healthcare providers with detailed information on the importance of implementing information technology. For instance, information technology makes their work easier, reduces operational costs, and enhances the quality of care provided to patients. Accordingly, the research provides them with the challenges faced in implementing information technology so that they can identify strategies to address them earlier before they have a negative impact on the project.
References
[1] Berkman ND, Wynia MK, Churchill LR. Gaps, conflicts, and consensus in the ethics statements of professional associations, medical groups, and health plans. J Med Ethics. 2004 Aug; 30(4):395–401. [2] ABIM Foundation. American Board of Internal MedicineACP-ASIM Foundation. American College of Physicians-American Society of Internal Medicine European Federation of Internal Medicine. Medical professionalism in the new millennium: a physician charter. Ann Intern Med. 2002 Feb; 136(3):243–6. [3] Singh, R., Mathiassen, L., Astapova, E. and Stachura, M. “Dynamic Capabilities in Home Health: IT-enabled Transformation of Post-acute Care.” Journal of Association for Information Systems, Vol. 12, 163-188, 2011. [4] Rai, A., Chen, L., Pye, J., and Baird, A. “Understanding determinants of consumer mobile health (eHealth) usage intentions, assimilation, and channel preferences,” Journal of Medical Internet Research, 2013 (15:8 e149), 1-20. [5] Bhargava, H., Mishra, A.N. “Electronic Medical Records and Physician Productivity: Insights from Panel Data Analysis and Design Implications.” Submitted to Conference on Information Systems and Technology, INFORMS, Charlotte, NC, November 12 – 13, 2011. [6] Gawande A. The checklist manifesto: how to get things right. New York: Picador USA; 2011 [7] Koppel R, Gordon S.First, do less harm: confronting the inconvenient problems of patient safety (the culture and politics of health care work). Ithaca: ILR Press; 2012 [8] Thimbleby H. Improving safety in medical devices and systems. Proceedings IEEE International Conference on Healthcare Informatics (ICHI 2013). September 2013. Available from: http://harold.thimbleby.net [9] McDonald KM , Sundaram V , Bravata DM , Lewis R , Lin N , Kraft S et al. Technical Review 9: Closing the quality gap: a critical analysis of quality improvement strategies: volume 7—care coordination [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; 2007 Jun [cited 2016 Aug 22 ]. (AHRQ Publication No. 04[07]- 0051-7). [10] Mohanan M , Giardili S , Das V , Goldhaber-Fiebert J , Miller G , Rabin T et al. The effect of social franchising and telemedicine on health provider knowledge and quality of care: evidence from Bihar, India. (Unpublished paper, Durham, NC, 2016)
Copyright
Copyright © 2023 Dr. Anupriya Jain, Kumkum Sharma, Alisha Singh, Melbin Kurien. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET55180
Publish Date : 2023-08-04
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

