Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Integral Review on Pulmonary Tuberculosis
Authors: Role Shital .S, Mane Anant .M, Parsewar Hrushikesh .B, Nidwanche Shruti .V
DOI Link: https://doi.org/10.22214/ijraset.2024.64233
Certificate: View Certificate
Abstract
Since tuberculosis is a chronic, systemic occupational disease that is common in developing nations, it is an important public health concern. The primary pulmonary pathogen that causes disease by infection is Mycobacter tuberculosis. Pathogens can cause disease by infecting almost any part of the body. The primary goal of the study was to raise awareness and provide information about tuberculosis infection, which is caused by bacteria isolated from the host\'s implementary cells. This infection can progress to a highly contagious stage, at which point the patient may experience symptoms such as bloody coughing, fever, night sweats, and weight loss. only those with infectious active pulmonary tuberculosis. The purpose of that quick study was to broaden students\' and society members\' knowledge. India has the highest rate of tuberculosis deaths worldwide, with about 600 deaths each day from the disease. The infectious disease that kills the greatest number of adults in India is tuberculosis. In 2012, the Indian government designated tuberculosis (TB) as a notifiable ailment, meaning that any physician who suspects a patient has TB must report the case to the government. TB control and treatment are covered by a national program in India that provides free treatment to all TB cases. The bacillus calmette guerin (BCG) vaccination is widely used globally to prevent the diagnosis of tuberculosis in infants and early children, even though it was unable to stop the global TB pandemic. Novel vaccinations are being developed in an attempt to increase immunisation effectiveness.
Introduction
I. INTRODUCTION
Tuberculosis (TB), one of the oldest illnesses known to man, has existed for at least several million years in human evolution. Tuberculosis remains a major global public health concern, especially in developing countries in Asia, Africa, and Latin America, despite notable progress in immunology and chemotherapy. Actually, half of all cases worldwide are found in China and India.It wasn't until the 1820s that TB was acknowledged as a separate disease. The illness was eventually dubbed "tuberculosis" by J. L. Schonlein in 1839. In 1882, Robert Koch discovered the cause of tuberculosis, an infectious disease transmitted by airborne organisms belonging to the mycobacterium tuberculosis (fig1) complex. [1] The mycobacterium species that cause tuberculosis (TB) that make up the M. tuberculosis complex are M. bovis, M. africanum, M. microti, M. caprae, M. pinnipedii, M. canetti, and M. mungi. Despite being primarily a lung pathogen, mycobacterium tuberculosis can transmit disease throughout the body. A person who has tuberculosis in their lungs can transfer the disease through the air when they cough, sneeze, or talk. Coughing for at least three weeks is one of the general symptoms associated with tuberculosis. heart issues, bloody coughs, persistent exhaustion, chills, night sweats, cold, loss of appetite, and weight loss. Pulmonary tuberculosis is a sickness spread by air.A chest x-ray, sputum test, and other techniques can be used to diagnose tuberculosis. Antibiotic cocktail therapies are a type of care that lasts longer than six months. BCG (bacille-clamette Guerin) vaccination, early detection and diagnosis, appropriate and thorough treatment, awareness campaigns, and other measures can all help lower the prevalence of tuberculosis.[2]
The micron-to-five-micron-diameter airborne droplet nuclei that carry M. tuberculosis are how it spreads. Infectious droplet nuclei are released when individuals suffering from pulmonary or laryngeal tuberculosis cough, sneeze, shout, or sing. By airborne means, tuberculosis can spread from one person to another. The dust in the air is a representation of the tubercle bacilli contained in the droplets nucleus.
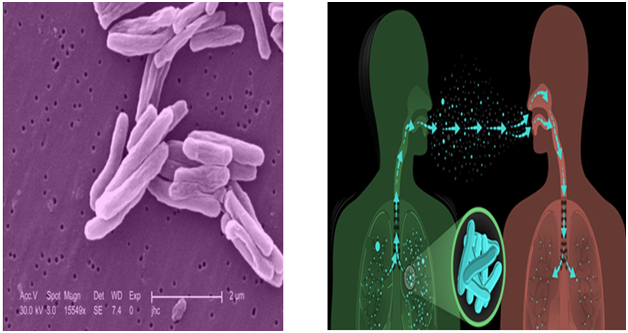
Fig no: 1 Pulmonary pathogen Fig no: 2 Spread pulmonary tuberculosis
Little children are less likely than adults to infect others with pulmonary and laryngeal TB infection. Children usually do not cough up phlegm, which explains why. Transmission from children is a conceivable, though. Therefore, when evaluating the infectiousness of children and adolescents with tuberculosis (TB) infection, the same criteria that apply to adults should be applied. In order to diagnose and track pulmonary tuberculosis (PTB), radiologists need to look for certain symptoms, such as a cough that lasts for three weeks or more, cavitation on a chest radiograph, or a respiratory tract infection that affects the larynx, lungs, or airways. Between 1995 and 2015, it is estimated that 66 million cases, or 85% of reported cases, of drug-susceptible pulmonary tuberculosis were successfully treated.Even after a microbiologic cure, as many as 50% of TB survivors still suffer. Persist in having some kind of lung impairment.Heart failure, which can range from minor irregularities to severe dyspnoea, may raise the risk of dying from respiratory causes.Furthermore, it seems to have treated TB patients. considerably increase the burden of chronic obstructive pulmonary disease (COPD) worldwide.The development of pulmonary impairment following TB treatment techniques is required by these facts. [3]
A. Epitomeology
The breadth and evolution of tuberculosis across time must be considered in order to ascertain its epidemiology. Epidemiology, the cornerstone of public health practise, provides strategies for managing the illness. There are several sophisticated epidemiological indices that are used.
B. Mortality
The number of deaths caused by tuberculosis has historically been used to gauge the intensity of the pandemic. Mortality is expressed as the number of tuberculosis deaths per unit of time (typically per year) and per unit of population (commonly 100,000). However, this data is not routinely collected in most of the countries where tuberculosis is prevalent. The World Health Organisation estimated that over 1.9 million fatalities globally in 1997 were attributable to TB. Of these deaths, over a million happened in South East Asia, less than 42,000 happened in developed countries, and the remaining instances were spread equally around the globe. TB is thought to be the cause of 2.8% of deaths globally across all age groups, and 26% of these preventable deaths occur in underdeveloped nations.
C. Morbidity
To quantify the morbidity of tuberculosis, two primary metrics are used: the prevalence and incidence indices.[4]
II. DISEASE PREVALENCE
Prevalence can only be determined by studies that use results that can be generalized to the entire population. These surveys are expensive and time-consuming, but they have been carried out in many nations to track the epidemiological evolution of tuberculosis. The number of cases per unit of population that are present in the neighborhood at any given period (usually 100 000) is known as the predominance of a disease.
- Variables or indicators: The annual number of tuberculosis-related fatalities per 100,000 people is known as the mortality rate.
- Rate of morbidity: The number of incidents in a certain time period per 100,000 people is known as the prevalence. Annual incidence is the number of new cases per 100,000 people in a given year. Virus Infection
- Prevalence: The proportion of the population that is afflicted at any one time The percentage of the population who become infected within a year is known as the annual incidence, or ARI. parameters (established by surveys carried out prior to the HIV epidemic) that connect the variables in the untreated state of the illness during its natural progression.
- Cases Die –this is the case-fatality rate: The yearly death toll is two times lower than the incidence and four times lower than the prevalence. All of these parameters are impacted by the implementation of national tuberculosis programs, especially those that include chemotherapy. [5]
The impact of the HIV epidemic that each trait is impacted by the incidence of HIV. In certain settings, an immunosuppressed individual has a 10-fold lower risk of contracting tuberculosis than an HIV-positive individual. Patients with tuberculosis who test positive for HIV die at a higher rate than those who test negative for HIV. [6]
III. GLOBAL INCIDENCE OF ACTIVE PULMONARY TB DISEASE
High-income nations, which include most of India, Indonesia, the Philippines, Bangladesh, China, and Pakistan, have the fewest cases of active tuberculosis (TB) disease. Ten cases of active tuberculosis are reported for every 100,000 persons in these nations each year. On the other hand, TB is more common in countries with lower incomes. The data utilized to generate these estimates came from capture-recapture processes, case notifications with expert views, prevalence surveys, and case notifications with standard modifications. Reprinted from World Health Organization’s Global Tuberculosis Report 2020, 20th edition. [7]
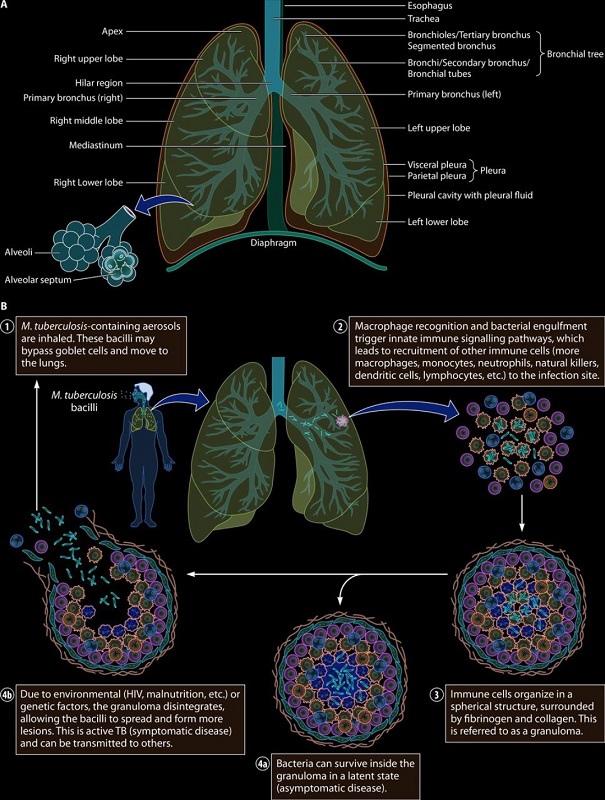
Fig No: 3 Process Of Developing Tb In Human Body
IV. PATHOPHYSIOLOGY OF PULMONARY TUBERCULOSIS
Nuclei from droplets harboring tubercle bacilli that enter the lungs' alveoli through inhalation cause infection. These tubercle bacilli are eaten by alveolar macrophages, whereupon the majority are either eliminated or inhibited. A small percentage of the dead macrophages may multiply inside the cell and be released. If these bacteria are still living, they may spread via 0
V. INFECTION OF TAP PULMONARY TUBERCULOSIS
A) Mycobacterium TB enters the lungs through inhalation and travels to the alveolar space, where it combines with the alveolar macrophages in the area to cause infection. If the germs are not eliminated by this first line of defense, M. tuberculosis either infects the alveolar macrophages or the alveolar epithelium directly, causing the latter to migrate to the lung parenchyma and infiltrate the lung interstitial tissue. Next, M. tuberculosis is transported to the pulmonary lymphatic system by either polymorph nuclear leukocytes or chronic inflammatory monocytes, which in turn activate T cells. Immune cells, such as T and B cells, are drawn to the lung parenchyma by this mechanism, where they develop into granulomas.
B) As the germs grow, the granuloma is getting bigger. If the bacterial burden is too great, the granuloma will not be able to contain the infection, and the germs will eventually move to the brain and other organs. The host has become infected, exhibiting symptoms, and is believed to be experiencing active tuberculosis. At this point, the germs have the potential to re-enter the respiratory tract and get discharged into the circulation. [9]
A. Types of Plumomary Tuberculosis
1) Primary tuberculosis Pneumonia
This rare type of tuberculosis is highly transmissible and presents as pneumonia. The individuals have an intense cough and a high fever. The most common demographics to experience it are the extremely young and the elderly. It is also seen in immunosuppressed patients, including those with HIV/AIDS, and those on long-term corticosteroid medication.[10]
2) Tuberculosis Pleurisy
Usually, this occurs soon after the first infection. The granuloma Lung edge rupture takes place in the pleural space, which is the region between the lungs and the chest wall. There are frequently a few tablespoons of fluid in the pleural space. [11]
3) Cavitary TB
Cavitary TB is a lung disease that affects the higher lobes. The germs cause cavities or enlarged air spaces, which eventually kill the lungs. Reactivation illnesses are a manifestation of this strain of tuberculosis. The higher lobes of the lung are affected due to their elevated oxygen concentration (an environment in which M. tuberculosis thrives). Rarely, cavitary tuberculosis can appear shortly after the first infection.[12]
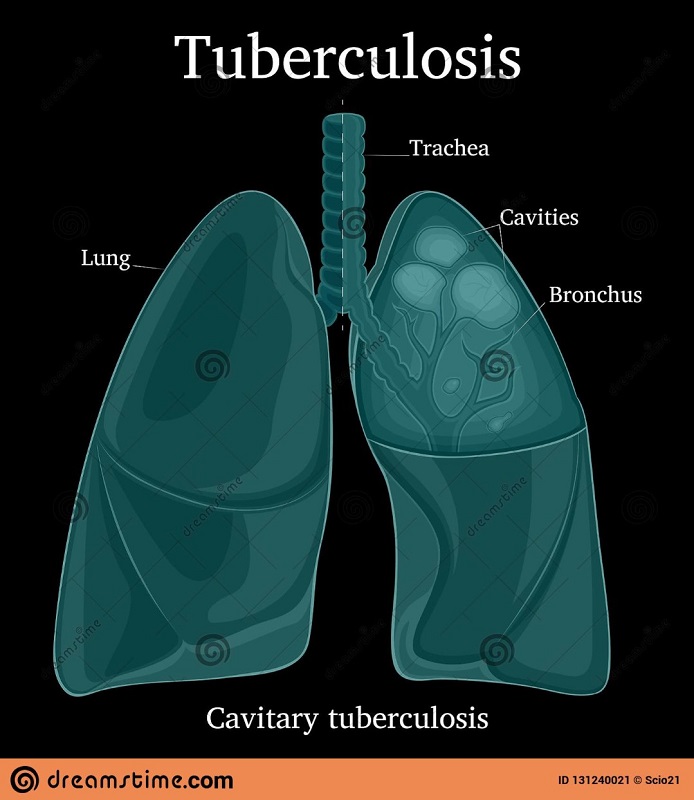
Fig No: 4 Diagram of cavity TB
4) Miliary TB
Military TB is a type of spread TB. Chest x-rays reveal tiny nodules throughout the lungs that resemble millet seeds; these are called "miliary" lesions. Promptly following the initial infection, mild TB may develop. The patient becomes extremely feverish and faces an imminent risk of death. The condition may also result in chronic illness and progressive decline.[13]
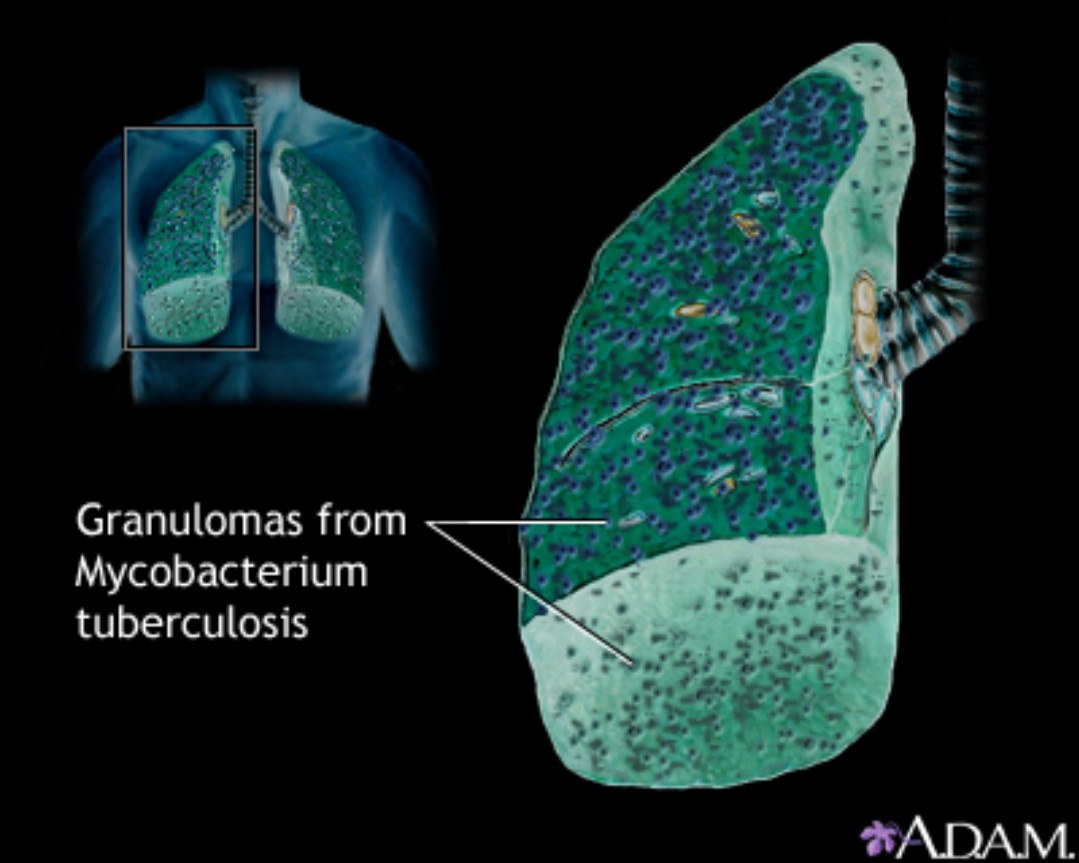 Fig No :4 Digaram Of Miliary Tb
Fig No :4 Digaram Of Miliary Tb
5) Laryngeal TB
TB can infect the larynx, or the vocal chord area. It is extremely infectious.

Fig No: 5 Laryngeal TB
VI. CAUSES OF PULMONARY TUBERCULOSIS
- The bacterium Mycobacterium tuberculosis (M. tuberculosis) causes the illness known as tuberculosis (TB).
- Thirty percent of humans carry this type of bacteria. However, only 10 to 20 percent of those infected with this virus go on to develop "active TB."
- Latent TB is the term used to describe those who possess the germs but do not exhibit any symptoms.This is not communicable, but it can become active tuberculosis later on, especially if an individual has compromised immune function due to an illness such as HIV.
- If the immune system is unable to stop the bacteria from multiplying, tuberculosis (TB) may develop. But a lot of latent tuberculosis patients never get active TB. A physician may perform a blood or skin test to identify M. tuberculosis.
- The germs are exhaled by a person with active pulmonary TB when they speak, sneeze, cough, or exhale little water droplets. These droplets can be inhaled as they move through the atmosphere.[7]
VII. RISK FACTORS FOR PULMONARY TB
Those who often interact with TB patients are most at risk of developing pulmonary tuberculosis. This entails being surrounded by friends or family who are TB carriers or working in locations such as those mentioned below, which often host individuals afflicted with the disease:
- Correctional facilities
- Group homes
- Nursing homes
- Hospitals
- Shelters [8]
A. The Following People Are Also At Risk For Pulmonary Tb Disease
- Older adults
- Small children
- People who smoke
- Individuals suffering from autoimmune diseases like lupus or rheumatoid arthritis.
- Those who suffer from chronic diseases like diabetes or kidney disease.
- Users of injectable medications.
- Those with impaired immune systems, such as HIV-positive individuals.
- Either receiving chemotherapy or taking long-term steroids.[9]
B. General Symptoms Of Plumomary Tuberculosis
- Weight loss
- A loss of appetite
- Nausea and vomiting
- Low energy or fatigue
- Fever and chills
- Night sweat
Patients with latent tuberculosis do not feel sick or show any symptoms. Another possible symptom of Plumomary TB is fatigue. Your doctor will be able to determine whether you require a TB test after reviewing all of your symptoms. [10]
C. Saviour Symptoms Of Pulmonary Tuberculosis
The symptoms of TB might differ and develop gradually.
The principal symptoms of Plumomary TB are as follows:
A chronic cough that lasts three weeks or longer dependable source Breathlessness; coughing up phlegm or blood from the lungs; chest pain [11]
D. Diagnosis Of The Plumomary Tuberculosis
- During the examination, your physician will: Assess your physical state to check for lung fluid.
Find out about your past medical conditions. - Arrange for a chest x-ray.
Order a medical examination to be sure. - TB of the lungs
- A microbiological test is performed on sputum samples to diagnose pulmonary tuberculosis.
- Bacterial diagnosis of tuberculosis can be performed, depending on the number of samples examined and the time of day the sample is obtained (Appendices 3 and 4).
- For any patient suspected of having tuberculosis, three sputum samples should be obtained over the course of two days: two should be obtained at home by the patient the morning of the consultation, and one should be taken on the spot during the interview.construction day. These samples must be microscopically analysed and, if practical, cultivated. [12]
If all three investigative results are clear but the chest radiograph shows symptoms suggestive of microscopic inspection, the patient should be recommended a course of large and diversified antibiotics. If appropriate, a culture should be performed a week later if symptoms have not improved after therapy. If all light microscope exams are negative, it is necessary to wait for the results of the culture, if one has been performed, or to refer the patient to a more qualified physician for confirmation of tuberculosis or the formation of a different diagnosis. It is never recommended to confirm a tuberculosis diagnosis with a trial course of anti-tuberculosis treatment. Seldom does touch constitute a serious threat to life. Generally speaking, there is always enough time to fully assess the situation utilizing the expanding corpus of evidence suggesting. [13]
E. Criteria For The Diagnosis Of Pulmonary Tuberculosis
1) Smear-Positive Cases:
Two or more positive smear results; one positive smear with radiographic abnormalities suggestive of lung tuberculosis; or one positive smear plus one positive culture .
2) Smear-Negative Cases
At least two series of negative smears from samples obtained at least two weeks apart, along with one or more positive cultures and three negative smears, or at least two series of negative smears with persistent radiographic abnormalities consistent with active tuberculosis, not improved with a minimum of one week of treatment with broad-spectrum antibiotics. [14]
3) Other exams
These tests may also screen for pulmonary tuberculosis (TB), which can be challenging to diagnose in adults and children with drug-resistant tuberculosis or HIV (MDR-TB). The two most successful TB drugs, isoniazid and rifampin, do not completely eradicate the TB bacteria that cause multidrug-resistant tuberculosis (MDR TB). All TB patients are treated with these medications. Treatment for MDR TB should involve consultation with experts in the field. [15]
4) TEST
- CT scan
- A lung imaging test to check for disease-related evidence.
- Bronchoscopy
A procedure when a scope is put into your mouth or nose to allow your doctor to view your airways and pulmonary system. [16]
- Thoracentesis
A procedure to remove fluid from the junction of your chest wall and the outside of your lungs.
5) Lungs biopsy
A technique for obtaining a small amount of respiratory system [17]
6) Treatment
If you are asymptomatic, treatment for latent tuberculosis is still necessary. Future cases of pulmonary tuberculosis are still possible. You might only require one TB drug if you have latent tuberculosis. A number of therapies may be recommended by your doctor if you have pulmonary tuberculosis. To have the best outcomes, you should take these medications for at least six months. [18]
The most often used TB medications are:
Ionized
Pyrazinamide
Ethambutol (Myambutol)
Rifampin (Rifadin)
Directly observed therapy (DOT) is a technique that your doctor may use to ensure that you complete your treatment. Drug resistance in pulmonary tuberculosis can be exacerbated by skipping or quitting treatment, and this can lead to MDR-TB. [19]
With DOT, you don't have to worry about forgetting to take your medication because a medical professional visits you once a day or several times each week to administer it.If you are not on the DOT, establish a regimen for taking your meds to ensure that you don't miss a dose. to assist you in remembering to take your prescription. For six months, take isoniazid and rifampicin together. Two more antibiotics (pyrazinamide and ethambutol) were provided for the first two months of the six-month therapy period. Before you feel better, it could take a few weeks. The severity of your tuberculosis and your overall health will determine how long it takes.[20]
After taking antibiotics for two weeks, most patients start to feel better and become less contagious. However, it's crucial that you adhere to the directions on your prescription medication and complete the course of antibiotics. The best method to make sure the TB bacteria are eliminated is to take medicine for six months. Your tuberculosis infection may become resistant to the antibiotic if you stop taking it before the recommended time frame or forget to take a dose. If, on a daily basis, you find it difficult to remember to take your prescription, your healthcare team can work with you to find a solution. [21]
This may entail communicating often with your treatment team at home, at the clinic, or at a more convenient location. If the prescribed treatment plan is followed, you shouldn't require any additional TB expert exams. It's unusual, but you can receive guidance on recognizing symptoms of the illness reoccurring. [22]
Ayurvedic drugs pulmonary tuberculosis.
- Ashwagandha (Withania somnifera)
- Chavanprash
- Guduchi (Tinospora cordifolia)
- Amla (phllyantus emblica) [23]
VIII. CLASSIFICATION OF TUBERCULOSIS
Antituberculosis drugs.
A. First line drugs
- Isoniazide(H)
- Rifampin (R)
- Pyrazinamide (Z)
- Ethambutol (E)
- Streptomycin (S)
B. Second Line Drugs
1) Fluiroquinolones
- Ofloxacin
- Levofloxacin
- Moxifloxacin
- Ciprofloxacin
2) Othar Oral Drugs
- Ethionamide
- Prothionamide
- Cycloserine
- Para amino salicylic acid (PAS)
- Rifabutin
3) Injectable Drugs
- Kanamycin . [24]
RNTCP- Revised National Tb Control Programme.
Launched in 1997 and gradually expanded throughout the nation with assistance from the World Bank and other development partners, the RNTCP is based on the globally advised directly observed treatment short course DOTS model. For bacteriological examination of sputum, the RNTCP qualified assurance laboratory network consists of three tiers: designated microscopy in (DMC), intermediate reference laboratory in (IRL), and national reference laboratory. [25]
IX. PREMIUM BENEFITS
A. Prevention
If your test results indicate that you have a latent tuberculosis infection, your doctor may recommend medication to reduce your risk of developing active tuberculosis. Spread is limited to active tuberculosis. [26]
B. Protocol your family and friends
No matter how many years you are, it usually takes a few weeks of anti-tuberculosis medication treatment when you have active tuberculosis. You can maintain the health of your friends and family by implementing this advice. [27]
- Stay at home: Don't go to work or school, or share a bed with anybody else, for the first few weeks of therapy.
- Open the door to the room. The bacteria that cause tuberculosis can proliferate faster in cramped, enclosed areas with stagnant air. Open the windows and use a fan to circulate the inside air outside if it's not too cold outside. [28]
- Cover your mouth: Use a tissue to shield your lips whenever you cough, sneeze, or laugh.
- Wear a face mask: During the first three weeks of therapy, having to wear a face mask while you are around various individuals may help reduce the chance of transference. [29] Completing your medicine is likely the most crucial action you can take to prevent tuberculosis in both yourself and other people. Missing doses or ending treatment early increase the chance that the TB bacteria will adapt and develop resistance to even the strongest TB medications. Drug-resistant varieties become increasingly lethal and challenging to cure as they evolve.[30]
- Vaccinations: Infants are frequently given the Bacille Calmette-Guerin (BCG) vaccine in places where tuberculosis is more common. Due to its ineffectiveness un adults, the BCG vaccine is not advised for widespread use in the US. At various phases of development and testing, numerous new TB vaccines are being created.[31]
Conclusion
People have used their lungs to give drugs for thousands of years. Several such drugs are still primarily administered using pulmonary drag administration today. Pulmonary medication distribution is an important area of research that affects the diagnosis of conditions such as chronic obstructive pulmonary disease and other illnesses. Breathing is the most direct pathway to the pharmaceutical target. Because the medication is injected directly into the lung\'s conducting zone during pulmonary administration, there is less chance of systemic side effects, a prompt response, and a lower dosage required to treat obstructive respiratory diseases. Recently, numerous alternative needle-free techniques have been developed to improve the pulmonary medicine delivery system\'s efficacy without sacrificing its integrity. Therefore, the optimal route of administration is through the lungs. A. Future perspective Because of its state, TB is more likely to spread throughout India. Immense poverty, malnutrition dense population, smoking the largest number of diabetes patients in the world HIV. Thus, all of these factors promote the growth of the TB bacterium. to eradicate TB in India. Reducing poverty and promoting excellent nutrition and smoking cessation are important goals. in order to reduce the number of patients suffering from tuberculosis. A healthy diet is your best defense in this conflict. The Indian government launched the DOTS (direct observer treatment) program and the RNTCP (revised national TB control programs). The DOTS program has been quite successful in treating tuberculosis in the nation, however there are several issues with it that make it difficult to treat the disease effectively. B. Alternate day therapy The plan of alternate therapy should be give to the patient on daily basis. C. Timing of DOTS centres 1) The timing of most of the dots Centre are not as per the convenience of patient. 2) Patience have to leave their work and come to the clinic. 3) So government of Indian should change that timing. 4) Shortage of drug and unavailable of drug so medicine should be met on time. 5) The MDR test should be included to the program by the government so that TB patients can begin using first-line medications. Whether it\'s MDR TB or regular TB, an early diagnosis willbemade. There should be a small modification to the way tuberculosis is treated. There are too many tablets in this medication; fewer tablets are needed. For example, the use of nanoparticles and polymers in NDDS technology to combine drugs, if at all possible. in order to minimize the amount of pills required and increase the patient\'s level of comfort. The patient should get instructions from the pharmacist on how to take their medications correctly and on schedule.
References
[1] http://www.CDC.gov / tb / education / corecurr / pdf. Chapter 2.pdf [2] Madhukar pai. Tuberculosis International Journal of nature 27 oct ok;16076 [3] Maria T. A Westchester. Active pulmonary tuberculosis something old, something new, something Insights Imaging, 09 jan 2022. [4] Dye C et al. Global burden of tuberculosis: estimated incidence, prevalence and mortality by country. Journal of the American Medical Association, 1999; 282:677–686. [5] Robert L Tuberculosis 2: pathophysiology and microbiology of Pulmonary tuberculosis. South Sudan medical journal, 13 february [6] Dr. Michael Iseman tuberculosis : types. National Jewish health. 1 february 2013 [7] J. Keith fisher. What to know about pulmonary tuberculosis. https://www.medical newstoday. 20 june 2019 [8] Pulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysis, journey of clinical medicine. 30 jan 2022 [9] Alana biggers, Tuberculosis, healthline 12Nov 2021 [10] World Health Organization. Global tuberculosis report 2014 [Internet] Geneva: World Health Organization; 2014. [cited 2015 Mar 1]. Available from: http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf?ua=1. [Google Scholar] [11] Centers for Disease Control and Prevention https://g.co/kgs/hZGn5v [12] Marcelo Fouad Rabahi, Tuberculosis treatment, jornal barsileirode pneumologia 2017 Nov-Dec [13] K. D tripaathi book of pjarmacology.. [14] Patrick K Moonan. Tuberculosis preventive treatment: the next chapter of tuberculosis elimination in India, journal of BMJ global health 11 sep 2018 [15] ComPulmonary Tuberculosis and Risk of Lung Cancer: A Systematic Review and Meta-Analysisarticles/325526 20 jun 2019Sudan medical journal [16] Maria T. A Westchester. Active pulmonary tuberculosis something old, something new, something brought, something blue. Insights / maging ( 2022) https://doing. Org/10.1186/s 13244 [17] https://apps.Who.int/iris/bits tream/ handle/10665/68559/Who-CDC- The 99.272.pdf; sequence=1 [18] Robert L. Tuberculosis 2: pathophysiology and microbiology of Pulmonary tuberculosis. South Sudan medical journal. [19] J. Keith fisher. What to know about pulmonary tuberculosis. https://www.medical newstoday. Com/articles/325526 20 jun 2019 [20] Alana bigger, tuberculosis https://www/ healthline.com/helath/tuberculosis 12 Nov 2021 [21] J. Keith fisher. What to know about pulmonary tuberculosis. https://www.medical newstoday. Com/articles/325526 20 jun 2019 [22] Valeria saraceni, prevalent tuberculosis at HIV dignosis. Journal of acquired immuno deficiency syndrome(1999) 1sep 2015 1:67(1) :98-101 [23] Giovanni battista. Surgery and pulmonary tuberculosis. Journal of thoracic disease 11 Apr 2016 10.21037 [24] Gursimarat k sandhu. Tuberculosis: current situation, challenging overeview of it’s Control Programme in India. Journal of global infection diseases. 2011Apr-jun 10.4103 [25] World Health Organisation. Who Global project on anti tuberculosis [26] https://medicostimes.com/Ananthanarayana-and- painter’s-Microbiology-pdf/ [27] https://medicostimes.com/harsh-mohan-pathology-pdf/ [28] Anderson P, Doherty TM. The success and failure of BCG: implications for a novel tuberculosis vaccine. Nat Rev Microbiol 2005;3: 656-62. [29] Centres for disease control and prevention https://g.co/kgs/hZGn5v [30] https://medicostimes.com/harsh-mohan-pathology-pdf/ [31] https://www.cdc.gov/tb/topic/basics/default.htm
Copyright
Copyright © 2024 Role Shital .S, Mane Anant .M, Parsewar Hrushikesh .B, Nidwanche Shruti .V. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET64233
Publish Date : 2024-09-13
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

