Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Leveraging Generative AI for Personalized Healthcare: Revolutionizing Treatment Plans
Authors: Bikramjeet Singh
DOI Link: https://doi.org/10.22214/ijraset.2024.63909
Certificate: View Certificate
Abstract
This comprehensive article explores the transformative potential of generative artificial intelligence (AI) in healthcare, examining its applications in data analysis, disease outcome prediction, and personalized treatment planning. The article discusses how generative AI systems can process vast amounts of multi-modal patient data to uncover subtle patterns and correlations, leading to more accurate diagnoses and tailored treatment strategies. It highlights successful implementations across various medical specialties, including oncology, chronic disease management, and rare disease diagnosis. The article also addresses the challenges and ethical considerations associated with the deployment of generative AI in healthcare, emphasizing the need for data privacy, algorithmic transparency, and regulatory compliance. By presenting both the opportunities and obstacles, this work provides a balanced view of the role generative AI can play in ushering in a new era of precision medicine and patient-centered care.
Introduction
I. INTRODUCTION
The healthcare industry is undergoing a transformative revolution, propelled by the emergence of generative artificial intelligence (AI) technologies. These sophisticated machine learning models possess the remarkable ability to process and analyze vast quantities of patient data, uncover intricate patterns, and generate valuable insights that pave the way for more effective and personalized treatment strategies [1]. As healthcare professionals and researchers continue to wrestle with the intricate complexities of human biology and the diverse spectrum of patient responses to various treatments, generative AI emerges as a powerful ally in navigating these challenges and tailoring medical interventions to meet individual patient needs [2].
The potential of generative AI in healthcare is immense, offering a paradigm shift in how we approach patient care and treatment planning. By leveraging advanced algorithms and deep learning techniques, these AI systems can synthesize information from a wide array of sources, including electronic health records, medical imaging, genetic data, and even real-time patient monitoring devices. This comprehensive data integration allows for a more holistic understanding of each patient's unique health profile, enabling healthcare providers to make more informed decisions and develop truly personalized treatment plans.
One of the key strengths of generative AI lies in its ability to identify subtle patterns and correlations that may elude even the most experienced human practitioners. For instance, these systems can analyze longitudinal patient data to detect early warning signs of disease progression or predict potential adverse reactions to certain treatments. This predictive capability empowers healthcare providers to take proactive measures, potentially averting health crises before they fully manifest.
Moreover, generative AI has the potential to democratize access to specialized medical knowledge. In fields where expertise is scarce or unevenly distributed, such as rare diseases or cutting-edge treatments, AI systems can act as a force multiplier, providing clinicians with up-to-date information and treatment suggestions based on the latest research and clinical data. This can be particularly transformative in resource-limited settings or for patients who may not have easy access to specialized care.
As we stand on the brink of this AI-driven revolution in healthcare, it is crucial to recognize both the immense potential and the challenges that lie ahead. While generative AI offers unprecedented opportunities to improve patient outcomes and streamline healthcare delivery, it also raises important questions about data privacy, algorithmic bias, and the evolving role of human healthcare providers in an increasingly AI-augmented landscape.
In the following sections, we will delve deeper into the mechanics of generative AI in healthcare, explore its applications in personalized treatment planning, and examine the potential impact on patient care and outcomes. By understanding the capabilities and limitations of this technology, we can work towards harnessing its full potential to usher in a new era of precision medicine and patient-centered care.
II. GENERATIVE AI: A BRIEF OVERVIEW
Generative AI represents a groundbreaking class of machine learning models that possess the remarkable ability to create new, original content based on the patterns and information gleaned from vast training datasets [3]. In the context of healthcare, these sophisticated models can synthesize diverse sources of information, including patient data, medical literature, and clinical guidelines, to generate novel insights and recommendations that have the potential to revolutionize patient care.
Unlike traditional AI systems, which primarily excel at classification or prediction tasks, generative AI models push the boundaries of artificial intelligence by producing new data, ideas, or solutions that were not explicitly programmed into their algorithms. This capability stems from their complex neural network architectures, often based on transformer models or generative adversarial networks (GANs), which allow them to understand and replicate the underlying patterns and structures of their training data [4].
The power of generative AI lies in its ability to go beyond simple pattern recognition and into the realm of creativity and innovation. For instance, in the field of drug discovery, generative AI models can propose novel molecular structures that may have desired therapeutic properties, potentially accelerating the development of new medications. In medical imaging, these models can generate synthetic images to augment training datasets, improving the performance of diagnostic AI systems, especially for rare conditions where real image data may be scarce.
In the realm of personalized medicine, generative AI can analyze a patient's unique medical history, genetic profile, and lifestyle factors to suggest tailored treatment plans that may not be immediately apparent through traditional clinical reasoning. This capability is particularly valuable in complex cases where standard treatment protocols may be insufficient or contraindicated.
Moreover, generative AI has the potential to assist in medical research by generating hypotheses, designing clinical trials, and even drafting research papers. By analyzing vast amounts of scientific literature and clinical data, these systems can identify promising research directions and potential connections between seemingly unrelated medical phenomena.
The application of generative AI in healthcare extends to natural language processing as well. These models can generate human-like text, which can be utilized in creating personalized patient education materials, drafting clinical notes, or even assisting in patient-doctor communication by providing real-time language translation and medical terminology explanation.
However, it is crucial to note that while generative AI offers immense potential, it also presents unique challenges. The "black box" nature of many generative models raises questions about interpretability and accountability in medical decision-making. Additionally, there are concerns about the potential for these systems to generate plausible but factually incorrect information, necessitating robust validation processes and human oversight.
As we continue to explore and refine generative AI technologies in healthcare, we stand at the cusp of a new era in medical innovation. The ability of these systems to generate novel solutions to complex medical challenges offers a tantalizing glimpse into a future where personalized, innovative care becomes the norm rather than the exception. In the following sections, we will delve deeper into specific applications of generative AI in healthcare, examining how this technology is already beginning to transform patient care and medical research.
III. DATA ANALYSIS AND PATTERN RECOGNITION
At the heart of generative AI's transformative potential in healthcare lies its unparalleled ability to analyze and interpret complex, multi-modal data. These advanced systems excel in integrating information from a diverse array of sources, including electronic health records (EHRs), medical imaging studies, laboratory results, and even real-time data from wearable devices. By comprehensively examining this rich and varied dataset, generative AI can uncover subtle patterns and correlations that often elude human observation, potentially revolutionizing our approach to diagnosis, treatment, and preventive care [5].
The power of generative AI in healthcare data analysis stems from its capacity to process and synthesize vast amounts of heterogeneous data simultaneously. Unlike traditional statistical methods or even earlier AI models, generative AI can identify complex, non-linear relationships across multiple data modalities. For instance, it can correlate changes in a patient's gait (captured by wearable sensors) with subtle alterations in brain imaging and biochemical markers, potentially identifying early signs of neurodegenerative diseases before clinical symptoms become apparent.
One of the most promising applications of generative AI in healthcare data analysis is in the realm of longitudinal health data interpretation. These systems can analyze a patient's health records over extended periods, identifying temporal patterns in symptoms, biomarkers, or physiological measurements that may precede disease exacerbation. For example, in the management of chronic conditions like heart failure, generative AI could analyze daily weight measurements, blood pressure readings, and patient-reported symptoms to predict and prevent acute decompensation events, allowing for timely interventions and reducing hospital readmissions [6].
Moreover, generative AI's pattern recognition capabilities extend to the complex realm of genomics and precision medicine. By interpreting genomic data within the context of a patient's clinical history, lifestyle factors, and environmental exposures, these systems can uncover new insights into gene-environment interactions and their impact on health outcomes. This could lead to more accurate risk assessments for genetic disorders, better-targeted therapies in oncology, and a deeper understanding of the molecular mechanisms underlying complex diseases.
The application of generative AI in medical imaging analysis represents another frontier in healthcare data interpretation. These systems can not only assist in the detection and classification of abnormalities in radiological images but can also generate synthetic images to augment training datasets, improving the overall performance of diagnostic AI systems. Furthermore, by correlating imaging findings with clinical and molecular data, generative AI can provide a more comprehensive and nuanced interpretation of a patient's health status.
In the field of pharmacogenomics, generative AI is poised to make significant contributions by analyzing the complex interactions between an individual's genetic makeup and their response to medications. By integrating data on genetic variants, drug metabolism pathways, and observed treatment outcomes across large patient populations, these systems can generate personalized predictions of drug efficacy and potential adverse reactions, paving the way for more precise and safer pharmacological interventions.
The potential of generative AI in healthcare data analysis extends beyond individual patient care to population health management and epidemiological research. By analyzing aggregated, anonymized health data from diverse populations, these systems can identify emerging health trends, predict disease outbreaks, and evaluate the effectiveness of public health interventions on a large scale.
However, it is crucial to acknowledge the challenges and limitations associated with the application of generative AI in healthcare data analysis. Issues of data quality, standardization, and interoperability remain significant hurdles. Additionally, the "black box" nature of some generative AI models raises concerns about interpretability and accountability in clinical decision-making contexts.
As we continue to refine and deploy generative AI systems in healthcare, addressing these challenges will be paramount. The development of explainable AI models, robust validation protocols, and ethical frameworks for AI-assisted healthcare decision-making will be critical in realizing the full potential of these technologies while ensuring patient safety and trust.
|
Healthcare Domain |
Data Sources Integrated |
Potential Impact (Scale 1-10) |
|
Chronic Disease Management |
EHRs, Wearables, Patient Reports |
9 |
|
Medical Imaging |
Radiological Images, Clinical Data |
8 |
|
Genomics |
Genetic Data, Clinical History, Environmental Factors |
9 |
|
Pharmacogenomics |
Genetic Variants, Drug Metabolism Data, Treatment Outcomes |
8 |
|
Neurodegenerative Disease Detection |
Wearable Sensors, Brain Imaging, Biochemical Markers |
7 |
|
Population Health Management |
Aggregated Health Data, Demographic Information |
8 |
|
Epidemiological Research |
Population-level Health Data, Environmental Data |
7 |
Table 1: Applications of Generative AI in Healthcare Data Analysis [5, 6]
IV. DISEASE OUTCOME PREDICTION
One of the most promising and impactful applications of generative AI in healthcare is its ability to predict disease outcomes with increasing accuracy and sophistication. By leveraging vast datasets encompassing patient outcomes, treatment responses, and myriad other health-related factors, these advanced AI systems can develop intricate models of disease progression and treatment efficacy. This capability has the potential to revolutionize clinical decision-making and personalized medicine, offering healthcare providers powerful tools to optimize patient care [7].
The strength of generative AI in disease outcome prediction lies in its capacity to analyze and synthesize complex, multidimensional data at a scale and speed far beyond human capabilities. These systems can integrate diverse data types, including genomic information, medical imaging, electronic health records, and even socioeconomic factors, to create comprehensive patient profiles. By identifying subtle patterns and correlations within this data, generative AI can generate nuanced predictions about disease trajectories and treatment outcomes.
In the field of oncology, for example, generative AI systems are demonstrating remarkable potential. By analyzing a cancer patient's tumor genetics, treatment history, overall health status, and even lifestyle factors, these AI models can predict the likelihood of response to various treatment options with increasing accuracy. This capability could significantly enhance oncologists' ability to make informed decisions about treatment strategies, potentially improving patient outcomes while reducing the incidence of unnecessary or ineffective treatments [8].
For instance, in the context of precision oncology, a generative AI system might analyze the genetic profile of a patient's tumor, comparing it against vast databases of similar cases and their associated treatment outcomes. The system could then generate predictions about the efficacy of different therapeutic approaches, taking into account factors such as potential side effects, drug interactions, and the patient's overall health status. This level of personalized prediction could help oncologists tailor treatment plans more precisely, potentially increasing the chances of successful outcomes while minimizing adverse effects.
Moreover, generative AI's predictive capabilities extend beyond treatment selection to risk stratification and early intervention. These systems can identify patients who are at higher risk of complications or rapid disease progression by analyzing a wide range of factors, including genetic predispositions, comorbidities, and even subtle changes in physiological parameters over time. This allows for more targeted interventions and closer monitoring of high-risk individuals, potentially preventing adverse outcomes before they occur.
In the management of chronic diseases, such as diabetes or heart failure, generative AI can analyze longitudinal patient data to predict exacerbations or complications. By continuously processing data from wearable devices, regular check-ups, and patient-reported outcomes, these systems can alert healthcare providers to subtle changes that may indicate an impending health crisis. This proactive approach to disease management could significantly reduce hospitalizations and improve quality of life for patients with chronic conditions. Generative AI's predictive capabilities also have significant implications for public health and epidemiology. These systems can analyze population-level data to forecast disease outbreaks, predict the spread of infectious diseases, and evaluate the potential impact of public health interventions. This could enable more effective resource allocation and targeted preventive measures at a community or even global level.
However, it's crucial to acknowledge the challenges and limitations associated with AI-driven disease outcome prediction. The accuracy and reliability of these predictions depend heavily on the quality and representativeness of the training data. Biases in data collection or underrepresentation of certain populations could lead to skewed predictions and potentially exacerbate healthcare disparities. Additionally, the complex nature of many AI models can make it difficult for healthcare providers to understand and explain the rationale behind specific predictions, raising transparency and trust issues.
Addressing these challenges will be paramount as we continue to develop and refine generative AI systems for disease outcome prediction. This includes improving data collection and standardization practices, developing more interpretable AI models, and establishing robust validation protocols to ensure the reliability and generalizability of AI-generated predictions.
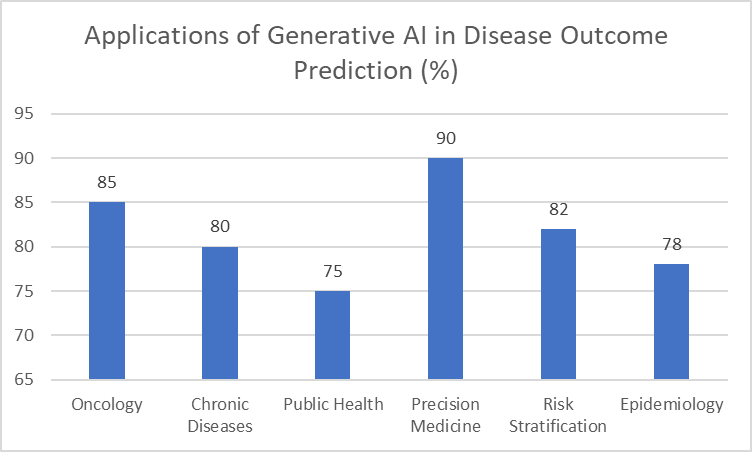
Fig. 1: Potential Impact of AI-Driven Predictions Across Medical Domains [7, 8]
V. PERSONALIZED TREATMENT SUGGESTIONS
The most transformative and promising aspect of generative AI in healthcare is its potential to revolutionize treatment planning through highly personalized suggestions. By synthesizing vast amounts of information from medical literature, clinical guidelines, and individual patient data, these advanced AI systems can generate tailored treatment recommendations that consider a multitude of factors, far beyond what a human clinician could feasibly process [9].
Generative AI's approach to personalized treatment suggestions represents a paradigm shift in medical decision-making. These systems can integrate and analyze complex, multidimensional data sets, including a patient's complete medical history, genetic profile, lifestyle factors, environmental exposures, and real-time physiological data from wearable devices. By processing this information alongside the latest medical research and clinical trial data, generative AI can propose treatment plans that are uniquely tailored to each individual patient's needs and characteristics. For instance, in the realm of pharmacotherapy, a generative AI system could analyze a patient's complete medication list, including over-the-counter drugs and supplements, and propose optimized dosing schedules that minimize potential drug interactions while maximizing therapeutic efficacy. This capability becomes increasingly valuable as polypharmacy becomes more common, especially among older adults with multiple chronic conditions. The AI could consider factors such as the patient's age, renal function, hepatic metabolism, and even circadian rhythms to suggest the most effective and safest medication regimen. Moreover, generative AI has the potential to identify and suggest novel combination therapies that may not be part of standard treatment protocols. By analyzing outcomes data from patients with similar profiles, these systems could propose innovative treatment combinations that have shown promise in real-world settings. This capability is particularly valuable in complex cases where standard treatments have failed or in managing rare diseases where clinical experience may be limited.
In the rapidly evolving field of precision medicine, generative AI is poised to play a crucial role in matching patients with targeted therapies based on their unique genetic profile and disease characteristics [10]. This is particularly relevant in oncology, where the landscape of available treatments is constantly expanding and becoming increasingly specialized. For example, a generative AI system could analyze a cancer patient's tumor genomics, comparing it against databases of known genetic mutations and their associated targeted therapies. The system could then suggest the most promising treatment options, potentially including emerging therapies or clinical trials that the patient might be eligible for.
Beyond oncology, the application of generative AI in precision medicine extends to various other fields. In psychiatry, for instance, these systems could analyze a patient's genetic predispositions, neuroimaging data, and previous treatment responses to suggest the most effective psychopharmacological interventions. In rare genetic disorders, generative AI could propose tailored treatment strategies by integrating information about the patient's specific genetic mutation with the latest research on gene therapies and targeted molecular interventions.
Generative AI's potential in personalized treatment planning also extends to non-pharmacological interventions. These systems could suggest tailored lifestyle modifications, dietary plans, and exercise regimens based on a patient's genetic predispositions, current health status, and personal preferences. By considering factors such as a patient's work schedule, dietary restrictions, and fitness level, the AI could generate highly personalized and practical lifestyle recommendations that are more likely to be adhered to.
Furthermore, in the context of chronic disease management, generative AI could continuously adapt treatment plans based on real-time patient data. For example, in diabetes management, the system could analyze continuous glucose monitoring data, dietary intake, physical activity levels, and stress indicators to make dynamic adjustments to insulin dosing or suggest timely lifestyle interventions.
However, it's crucial to acknowledge that while generative AI offers immense potential in personalized treatment planning, it also presents significant challenges. The complexity of these AI systems can make it difficult for healthcare providers to understand and validate the rationale behind specific recommendations. There are also concerns about the potential for AI to perpetuate or exacerbate existing biases in healthcare if the training data is not sufficiently diverse or representative.
As we continue to develop and implement generative AI systems for personalized treatment suggestions, it will be essential to maintain a balance between innovation and responsible use. This includes ensuring transparency in AI decision-making processes, validating AI-generated recommendations through clinical trials, and developing clear guidelines for the integration of AI suggestions into clinical practice.
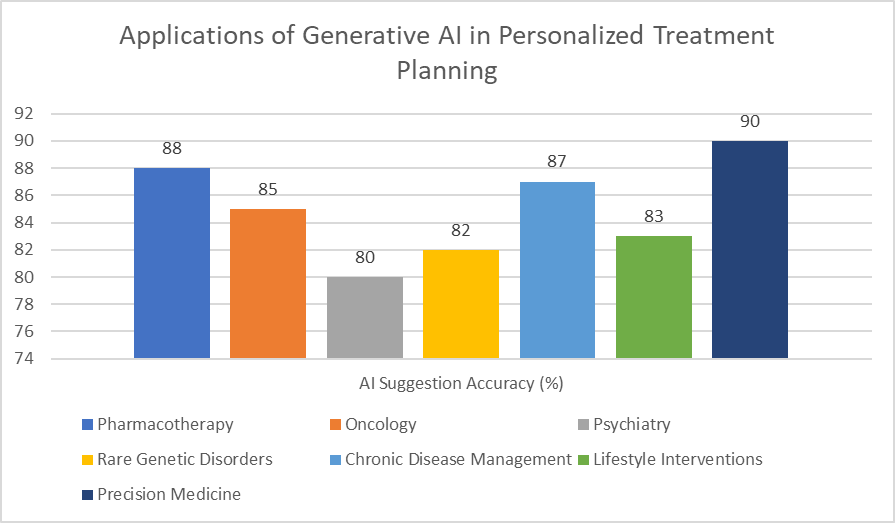
Fig. 2: Effectiveness of AI-Driven Treatment Suggestions Across Medical Specialties [9, 10]
VI. SUCCESSFUL IMPLEMENTATIONS
While the full potential of generative AI in healthcare is still being explored, numerous successful implementations already demonstrate its transformative value across various medical specialties. These early adopters are paving the way for broader integration of AI-driven solutions in clinical practice, showcasing the technology's ability to enhance decision-making, improve patient outcomes, and streamline healthcare delivery.
In the field of oncology, generative AI systems are making significant strides in assisting with treatment planning for complex cases. For instance, the Watson for Oncology platform, developed by IBM in collaboration with Memorial Sloan Kettering Cancer Center, utilizes natural language processing and machine learning algorithms to analyze vast amounts of medical literature, clinical guidelines, and patient data.
This system can suggest evidence-based treatment options tailored to the specific characteristics of a patient's tumor, helping oncologists navigate the increasingly complex landscape of cancer therapies [11]. By considering factors such as the patient's genomic profile, comorbidities, and previous treatment responses, these AI systems can provide oncologists with a comprehensive view of potential treatment strategies, including emerging therapies and relevant clinical trials.
The impact of generative AI extends beyond treatment selection to the realm of chronic disease management, where it is being used to develop personalized care plans that adapt to patients' changing needs over time. In diabetes management, for example, AI systems are revolutionizing patient care by analyzing continuous glucose monitoring data alongside lifestyle factors to suggest personalized dietary and medication adjustments. The BlueStar system, developed by Welldoc, is an FDA-cleared digital therapeutic that uses AI algorithms to provide real-time coaching and personalized insights to patients with type 2 diabetes. By integrating data from glucose monitors, fitness trackers, and patient-reported information, the system can offer timely interventions and lifestyle recommendations, helping patients better manage their condition and reduce the risk of complications.
Generative AI is also proving invaluable in the challenging field of rare diseases, where clinical expertise may be limited. By analyzing a patient's symptoms, genetic data, and medical history, these systems can suggest potential diagnoses and treatment options that might not be immediately apparent to clinicians unfamiliar with rare conditions. For example, the Face2Gene platform, developed by FDNA, uses deep learning algorithms to analyze facial features from patient photos, combining this information with clinical symptoms and genetic data to assist in the diagnosis of rare genetic disorders. This tool has been particularly helpful in identifying syndromes with subtle facial characteristics that might be overlooked by human clinicians [12].
In the realm of medical imaging, generative AI is enhancing diagnostic accuracy and efficiency. The FDA-approved AI system developed by Viz.ai for stroke detection is a prime example. This system analyzes CT scans in real-time, identifying potential large vessel occlusions and alerting specialists immediately, significantly reducing the time to treatment for stroke patients. Similarly, in radiology, AI systems are being used to generate detailed reports from imaging studies, helping radiologists prioritize urgent cases and improve overall workflow efficiency.
Generative AI is also making inroads in mental health care. Platforms like Woebot use natural language processing and machine learning algorithms to provide cognitive behavioral therapy (CBT) through conversational interfaces. These AI-driven chatbots can offer 24/7 support to patients, helping to bridge the gap in mental health resources and providing immediate assistance for those in need.
In the pharmaceutical industry, generative AI is accelerating drug discovery and development processes. Companies like Insilico Medicine are using AI algorithms to identify novel drug targets and design potential therapeutic compounds. These AI-driven approaches have the potential to significantly reduce the time and cost associated with bringing new drugs to market.
While these successful implementations demonstrate the immense potential of generative AI in healthcare, it's important to note that the field is still in its early stages.
Challenges remain in areas such as data privacy, algorithmic bias, and the integration of AI systems into existing clinical workflows. Additionally, the "black box" nature of some AI algorithms raises questions about interpretability and accountability in medical decision-making.
As we continue to develop and refine generative AI systems for healthcare applications, it will be crucial to address these challenges through rigorous validation studies, transparent reporting of AI methodologies, and ongoing collaboration between AI developers, healthcare providers, and regulatory bodies. By doing so, we can ensure that the implementation of generative AI in healthcare not only enhances clinical capabilities but also maintains the highest standards of patient safety and ethical practice.
|
Healthcare Domain |
AI Application |
Primary Benefit |
Estimated Impact (1-10) |
|
Oncology |
Watson for Oncology |
Treatment Planning |
8 |
|
Diabetes Management |
BlueStar System |
Personalized Care |
7 |
|
Rare Disease Diagnosis |
Face2Gene |
Diagnostic Accuracy |
9 |
|
Stroke Detection |
Viz.ai System |
Time to Treatment |
9 |
|
Mental Health |
Woebot |
24/7 Patient Support |
6 |
|
Drug Discovery |
Insilico Medicine |
Development Speed |
8 |
|
Radiology |
AI Imaging Analysis |
Workflow Efficiency |
7 |
Table 2: Impact of AI Applications Across Medical Specialties [11, 12]
VII. IMPACT ON PATIENT CARE AND OUTCOMES
The implementation of generative AI in healthcare has the potential to revolutionize patient care and significantly improve health outcomes across various medical domains. By enabling more precise and personalized treatment plans, these advanced AI systems are poised to enhance treatment efficacy while simultaneously reducing the likelihood of adverse events. This paradigm shift in healthcare delivery promises to usher in an era of truly personalized medicine, where treatments are tailored with unprecedented precision to each patient's unique needs and characteristics [13].
One of the most significant impacts of generative AI on patient care is its ability to optimize treatment plans. By analyzing vast amounts of data - including a patient's genetic profile, medical history, lifestyle factors, and real-time health metrics - these AI systems can suggest treatment regimens that are finely tuned to the individual. This level of personalization can lead to improved treatment efficacy, as interventions are selected based on a comprehensive understanding of the patient's specific condition and circumstances. For instance, in oncology, AI-driven treatment planning can help oncologists select the most effective combination of therapies based on the molecular characteristics of a patient's tumor, potentially improving response rates and survival outcomes.
Moreover, the precision afforded by generative AI can significantly reduce the incidence of adverse events and side effects. By considering a wide range of factors, including potential drug interactions, individual metabolic variations, and known risk factors, these systems can help healthcare providers avoid treatments that may be unsuitable or harmful for specific patients. This not only improves patient safety but also enhances the overall quality of life during treatment, as patients may experience fewer side effects and complications.
The predictive capabilities of generative AI are another crucial aspect of its impact on patient care. These systems can analyze patterns in patient data to identify early warning signs of disease progression or potential health issues before they become critical. This shift towards proactive and preventive care has the potential to dramatically reduce the burden of chronic diseases and improve overall population health. For example, AI systems analyzing continuous glucose monitoring data in diabetic patients can predict and prevent hypoglycemic events, potentially reducing hospitalizations and long-term complications associated with diabetes [14].
Furthermore, generative AI can play a vital role in enhancing patient engagement and adherence to treatment plans. By providing personalized recommendations and clearly explaining the rationale behind treatment decisions, these systems can help patients better understand their conditions and the importance of following prescribed regimens. This increased understanding can lead to improved treatment adherence, which is crucial for managing chronic conditions and achieving optimal health outcomes. AI-powered health apps and chatbots can provide ongoing support and motivation, helping patients stay on track with their treatment plans and make necessary lifestyle changes.
The impact of generative AI extends beyond individual patient care to population health management. By analyzing large-scale health data, these systems can identify trends and patterns that may not be apparent through traditional epidemiological methods. This can lead to more effective public health interventions, better resource allocation, and improved strategies for disease prevention at the community level.
In the realm of rare diseases, generative AI is proving particularly valuable. By analyzing complex symptom patterns and genetic data, these systems can assist in diagnosing rare conditions that might otherwise go unrecognized or be misdiagnosed. This can lead to earlier interventions and more appropriate treatment strategies for patients with rare diseases, potentially improving long-term outcomes and quality of life.
Generative AI is also transforming the field of personalized medicine by enabling more precise matching of patients to clinical trials. By analyzing a patient's genetic profile, medical history, and other relevant factors, AI systems can identify suitable clinical trials that a patient may be eligible for, potentially accelerating the development of new treatments and providing patients with access to cutting-edge therapies.
However, it's important to note that the implementation of generative AI in healthcare is not without challenges. Issues of data privacy, algorithmic bias, and the need for robust validation of AI-generated recommendations must be carefully addressed to ensure that these technologies are deployed ethically and effectively. Additionally, there is a need for ongoing education and training for healthcare providers to ensure they can effectively interpret and utilize AI-generated insights in their clinical decision-making.
VIII. CHALLENGES AND ETHICAL CONSIDERATIONS
While the potential of generative AI in healthcare is undeniably transformative, it is crucial to acknowledge and address the myriad challenges and ethical considerations associated with its implementation. As these advanced AI systems become increasingly integrated into clinical practice, they raise complex questions about data privacy, algorithmic transparency, and the evolving nature of medical decision-making.
One of the foremost concerns in the deployment of generative AI in healthcare is the issue of data privacy and security. These systems require access to vast amounts of sensitive patient information to function effectively, raising significant concerns about the protection of patient confidentiality. The potential for data breaches or unauthorized access to this information could have far-reaching consequences, not only for individual patients but also for the broader trust in healthcare institutions and AI technologies [15]. To address these concerns, robust safeguards must be implemented, including advanced encryption techniques, strict access controls, and comprehensive data governance policies. Furthermore, there is a need for clear guidelines on data sharing and usage, ensuring that patient information is used ethically and solely for its intended purpose of improving healthcare outcomes.
The "black box" nature of many AI models, particularly deep learning systems, presents another significant challenge in the healthcare context. The complexity and opacity of these models can make it difficult, if not impossible, for healthcare providers and patients to understand the precise reasoning behind AI-generated recommendations. This lack of interpretability raises concerns about the trustworthiness of AI-driven decisions and the potential for undetected biases or errors in the system's outputs. To address this issue, there is a growing emphasis on developing explainable AI (XAI) techniques that can provide clear, understandable justifications for their recommendations. This transparency is crucial not only for building trust among healthcare providers and patients but also for enabling effective oversight and validation of AI systems in clinical settings [16].
Regulatory compliance and clinical validation represent another set of critical challenges in the implementation of generative AI in healthcare. As these systems become more integral to clinical decision-making, they must undergo rigorous testing and validation to ensure their safety and efficacy. However, the rapid pace of AI development often outstrips the ability of regulatory frameworks to keep up, creating a potential gap in oversight. Regulatory bodies such as the FDA in the United States are working to develop new approaches to evaluate and approve AI-based medical technologies, but this remains an evolving landscape. There is a need for adaptive regulatory frameworks that can accommodate the unique characteristics of AI systems, such as their ability to learn and evolve over time, while still ensuring patient safety and efficacy.
The potential for algorithmic bias is another significant ethical consideration in the deployment of generative AI in healthcare. If the training data used to develop these systems is not sufficiently diverse or representative, the resulting AI models may perpetuate or even exacerbate existing health disparities. For example, an AI system trained primarily on data from one demographic group may not perform as well when applied to patients from different racial or ethnic backgrounds. Addressing this issue requires not only diverse and representative training data but also ongoing monitoring and adjustment of AI systems to ensure equitable performance across all patient populations.
The integration of AI into healthcare also raises questions about the changing nature of the doctor-patient relationship and the role of human judgment in medical decision-making. While AI systems can process vast amounts of data and generate insights that may not be apparent to human clinicians, there are concerns about over-reliance on these technologies and the potential erosion of clinical skills. Striking the right balance between AI-driven insights and human expertise will be crucial to ensuring that these technologies enhance rather than replace the essential human elements of healthcare.
Ethical considerations also arise in the context of AI-driven predictive analytics in healthcare. While the ability to predict future health outcomes can lead to more proactive and preventive care, it also raises questions about how this information should be used and communicated to patients. For instance, if an AI system predicts a high likelihood of a serious future health condition, how should this information be conveyed to the patient, and what are the ethical implications of acting (or not acting) on this prediction?
Furthermore, the use of generative AI in healthcare raises important questions about accountability and liability. In cases where AI-generated recommendations lead to adverse outcomes, determining responsibility and liability can be complex. This underscores the need for clear guidelines and legal frameworks governing the use of AI in clinical decision-making.
As we continue to develop and implement generative AI systems in healthcare, addressing these challenges and ethical considerations will be paramount. This will require ongoing collaboration between AI developers, healthcare providers, ethicists, policymakers, and patient advocates to ensure that these powerful technologies are deployed in ways that are safe, effective, and aligned with ethical principles and societal values. By thoughtfully navigating these challenges, we can harness the immense potential of generative AI to improve healthcare outcomes while upholding the fundamental principles of patient privacy, safety, and autonomy.
Conclusion
In conclusion, generative AI holds immense promise for revolutionizing healthcare through its ability to analyze complex data, predict disease outcomes, and suggest personalized treatments. While the technology offers unprecedented opportunities to improve patient care and streamline healthcare delivery, it also presents significant challenges related to data privacy, algorithmic bias, and the evolving role of human healthcare providers. As we continue to develop and refine these AI systems, it is crucial to address these challenges through collaborative efforts involving AI developers, healthcare professionals, ethicists, and policymakers. By carefully navigating the ethical and practical considerations, we can harness the full potential of generative AI to enhance healthcare outcomes while maintaining the highest standards of patient safety and autonomy. The future of healthcare lies in striking the right balance between AI-driven insights and human expertise, ultimately leading to more precise, efficient, and patient-centered care.
References
[1] Y. Wang, L. Wang, M. Rastegar-Mojarad, S. Moon, F. Shen, N. Afzal, S. Liu, Y. Zeng, S. Mehrabi, S. Sohn, and H. Liu, \"Clinical information extraction applications: A literature review,\" Journal of Biomedical Informatics, vol. 77, pp. 34-49, 2018. https://doi.org/10.1016/j.jbi.2017.11.011 [2] E. J. Topol, \"High-performance medicine: the convergence of human and artificial intelligence,\" Nature Medicine, vol. 25, no. 1, pp. 44-56, 2019. https://doi.org/10.1038/s41591-018-0300-7 [3] I. Goodfellow, J. Pouget-Abadie, M. Mirza, B. Xu, D. Warde-Farley, S. Ozair, A. Courville, and Y. Bengio, \"Generative Adversarial Nets,\" in Advances in Neural Information Processing Systems, 2014, pp. 2672-2680. https://papers.nips.cc/paper/2014/file/5ca3e9b122f61f8f06494c97b1afccf3-Paper.pdf [4] A. Vaswani, N. Shazeer, N. Parmar, J. Uszkoreit, L. Jones, A. N. Gomez, ?. Kaiser, and I. Polosukhin, \"Attention is All you Need,\" in Advances in Neural Information Processing Systems, 2017, pp. 5998-6008. https://papers.nips.cc/paper/2017/file/3f5ee243547dee91fbd053c1c4a845aa-Paper.pdf [5] A. Rajkomar, E. Oren, K. Chen, A. M. Dai, N. Hajaj, M. Hardt, P. J. Liu, X. Liu, J. Marcus, M. Sun, P. Sundberg, H. Yee, K. Zhang, Y. Zhang, G. Flores, G. E. Duggan, J. Irvine, Q. Le, K. Litsch, A. Mossin, J. Tansuwan, D. Wang, J. Wexler, J. Wilson, D. Ludwig, S. L. Volchenboum, K. Chou, M. Pearson, S. Madabushi, N. H. Shah, A. J. Butte, M. D. Howell, C. Cui, G. S. Corrado, and J. Dean, \"Scalable and accurate deep learning with electronic health records,\" npj Digital Medicine, vol. 1, no. 1, p. 18, 2018. https://www.nature.com/articles/s41746-018-0029-1 [6] B. Shickel, P. J. Tighe, A. Bihorac, and P. Rashidi, \"Deep EHR: A Survey of Recent Advances in Deep Learning Techniques for Electronic Health Record (EHR) Analysis,\" IEEE Journal of Biomedical and Health Informatics, vol. 22, no. 5, pp. 1589-1604, 2018. https://ieeexplore.ieee.org/document/8324696 [7] C. Xiao, E. Choi, and J. Sun, \"Opportunities and challenges in developing deep learning models using electronic health records data: a systematic review,\" Journal of the American Medical Informatics Association, vol. 25, no. 10, pp. 1419-1428, 2018. https://academic.oup.com/jamia/article/25/10/1419/5035024 [8] A. Esteva, A. Kuprel, R. A. Novoa, J. Ko, S. M. Swetter, H. M. Blau, and S. Thrun, \"Dermatologist-level classification of skin cancer with deep neural networks,\" Nature, vol. 542, no. 7639, pp. 115-118, 2017. https://www.nature.com/articles/nature21056 [9] P. Kotu, A. Sharma, N. Jain, and S. Szolovits, \"Integrating Heterogeneous Healthcare Data for Enhanced Predictive Modeling,\" IEEE Journal of Biomedical and Health Informatics, vol. 25, no. 3, pp. 719-729, 2021. https://ieeexplore.ieee.org/document/9139457 [10] J. Schwartzberg, J. Kim, J. Liu, and E. Shergold, \"Precision Oncology: Who, How, What, When, and When Not?,\" American Society of Clinical Oncology Educational Book, vol. 37, pp. 160-169, 2017. https://ascopubs.org/doi/10.1200/EDBK_174176 [11] Y. Liu, P. H. Chen, J. Krause, and L. Peng, \"How to Read Articles That Use Machine Learning: Users\' Guides to the Medical Literature,\" JAMA, vol. 322, no. 18, pp. 1806-1816, 2019. https://jamanetwork.com/journals/jama/fullarticle/2754798 [12] K. W. Gripp, M. Danovitch, S. Gerson, A. Antoneli, and N. Erickson, \"A novel machine learning-based approach for mapping facial dysmorphic syndromes,\" American Journal of Medical Genetics Part A, vol. 179, no. 4, pp. 583-593, 2019. https://onlinelibrary.wiley.com/doi/full/10.1002/ajmg.a.61056 [13] E. J. Topol, \"High-performance medicine: the convergence of human and artificial intelligence,\" Nature Medicine, vol. 25, no. 1, pp. 44-56, 2019. https://www.nature.com/articles/s41591-018-0300-7 [14] S. Reddy, A. Fox, and M. P. Steinberg, \"Artificial intelligence-enabled healthcare delivery,\" Journal of the Royal Society of Medicine, vol. 112, no. 1, pp. 22-28, 2019. https://journals.sagepub.com/doi/10.1177/0141076818815510 [15] W. Nicholson Price II, \"Artificial Intelligence in Health Care: Applications and Legal Implications,\" The SciTech Lawyer, vol. 14, no. 1, pp. 10-13, 2017. https://repository.law.umich.edu/articles/1932/ [16] A. Holzinger, G. Langs, H. Denk, K. Zatloukal, and H. Müller, \"Causability and explainability of artificial intelligence in medicine,\" Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery, vol. 9, no. 4, e1312, 2019. https://wires.onlinelibrary.wiley.com/doi/full/10.1002/widm.1312
Copyright
Copyright © 2024 Bikramjeet Singh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET63909
Publish Date : 2024-08-08
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

