Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
A Review of Machine Learning Technologies in Multiple Sclerosis Disease Detection
Authors: Fathimath Nihala T, Dr. N. Syed Siraj Ahmed
DOI Link: https://doi.org/10.22214/ijraset.2024.58117
Certificate: View Certificate
Abstract
Multiple sclerosis (MS) is a complex neurological disorder affecting the central nervous system, presenting challenges in accurate and timely diagnosis. This review paper provides a comprehensive overview of the evolving landscape of machine learning (ML) technologies employed in the detection and diagnosis of multiple sclerosis. Spanning the period from 2011 to 2022, the review synthesizes findings from a myriad of studies utilizing diverse data sources, including magnetic resonance imaging (MRI) and clinical data. The paper discusses various ML models and techniques applied in MS detection, with a focus on their strengths, limitations, and comparative performances. Key areas of exploration include the utilization of convolutional neural networks (CNN), support vector machines (SVM), and random forests (RF), among other approaches. The integration of advanced ML architectures, data augmentation strategies, and the incorporation of diverse data modalities are examined for their impact on diagnostic accuracy. Challenges such as distinguishing MS from diseases with similar symptoms, ensuring patient data confidentiality, and developing interpretable ML models are explored, along with proposed solutions. The review identifies promising opportunities for future research, including the implementation of secure platforms, the development of improved disease prognosis systems, and the combination of multiple data types for enhanced predictive capabilities. Additionally, the review emphasizes the potential for larger, multi-center datasets to bolster model reliability and advocates for the commercialization of ML solutions in MS diagnosis. In conclusion, this review consolidates current knowledge, highlights trends in ML applications for MS detection, and offers valuable insights to guide further advancements in this critical domain.
Introduction
I. INTRODUCTION
The most common chronic inflammation of the central nerve system is called multiple sclerosis (MS). The protective covering of the nerve cells is destroyed by this medical condition, which eventually results in deteriorated masses called plaques. Impaired eyesight, loss of balance, and learning struggles are just a few of the adverse consequences that result from cellular damage to the brain or spinal cord [1,2].
Currently, visual comparison of images taken at different times is used to diagnose and track the progression of diseases. The small size of the lesions, the various severities of the lesion progression (white, gray, and black holes), the size of lesions and their spatial distribution, and the degree of brain atrophy make this a time-consuming and difficult procedure for specialists. The main emphasis of an MS diagnosis is on the clinical signs of the suspected condition. After then, an MRI is used to provide a final diagnosis. The position and size of lesions in the brain's white matter portion are visible in these images, and this information is crucial for the diagnosis, course of treatment, and eventual outcome of the illness. The photos are also used to assess the response to MS treatment and verify the diagnosis, location of destruction, and severity of the disease. Since various illnesses result in brain lesions, a precise and expert identification of lesions due to multiple sclerosis is required [3].
The literature review focus on to find and compare the existing models of machine learning to detect progression of machine learning technologies. The lesions in the brain and spine helps to detect the same. There are currently 4 types of multiple sclerosis variants. The review goes through the possible image classification technologies and advancements on those.
Currently, the best method for diagnosing multiple sclerosis (MS), tracking the progression of the condition, and evaluating the efficacy of various treatments in trials is magnetic resonance imaging (MRI) [4, 5]. MRI-based MS diagnosis is laborious, time-consuming, and prone to human error. Consequently, machine learning (ML) and deep learning (DL) approaches are being employed in artificial intelligence (AI) to automate MS diagnosis [6,7]. ML is a sort of AI where computers are given the ability to learn without being explicitly programmed, whereas DL is a subset of ML built of techniques permitting the software to train itself to accomplish tasks by exposing multilayered neural networks to enormous amounts of data.
Several studies have analyzed prior research on AI-assisted MS diagnosis. For example, [6] examined many earlier studies that employed DL approaches for the automated diagnosis of MS using MRI data. They addressed the current issues and potential directions for future research in addition to talking about the most popular preprocessing methods.
Arani et al.'s [8] additional goal was to identify the best practices and procedures for MS diagnosis. To suggest the best approach, the writers examined how well each option worked. They discovered that the most popular techniques for MS diagnosis are rule-based, fuzzy logic (FL), and artificial neural networks (ANN). Additionally, they noted the drawbacks of each of these methods and suggested combining them to get around them.
DL and ML have been known to provide numerous advantages to medicine over the years. Among these are their ability to help clinicians identify patients who are at risk for the disease and warn them to stay away from triggers; identify patients who have the disease early and accurately so that treatment agents can be used to improve the quality of life for those patients; predict when a mild case of the disease will turn into a more serious one by analyzing different blood, cerebrospinal fluid (CSF), and radiological markers; and determine whether certain medications will be helpful in preventing the disease from getting worse and in conjunction with treatment monitoring.
II. TYPES OF MULTIPLE SCLEROSIS
A chronic autoimmune neurological disease that affects the brain and spinal cord, multiple sclerosis (MS) is a neurological illness that affects the central nervous system (CNS). Myelin, the covering that protects nerve fibers, is wrongly attacked by the immune system in multiple sclerosis (MS), which causes communication issues between the brain and the body. Multiple sclerosis comes in a variety of forms, each having unique symptoms and patterns of the disease. There are four primary types of MS:
A. Relapsing-Remitting MS (RRMS)
This is the most common form of MS, affecting approximately 85% of people diagnosed. Individuals with RRMS experience periods of relapses or flare-ups, during which new symptoms appear or existing ones worsen. These relapses are followed by periods of remission, during which the symptoms partially or completely improve. Over time, some people with RRMS may transition to a more progressive form of the disease.
B. Secondary Progressive MS (SPMS)
Many individuals with RRMS eventually transition to SPMS. In SPMS, there is a gradual worsening of symptoms and disability, with or without occasional relapses or plateaus. The progression can be steady or occur in a more unpredictable manner.
C. Primary Progressive MS (PPMS)
PPMS is less common than RRMS and SPMS, accounting for about 10-15% of cases. Unlike RRMS, PPMS is characterized by a steady progression of symptoms from the onset, without distinct relapses or remissions. People with PPMS may experience occasional plateaus or temporary improvements in symptoms.
D. Progressive-Relapsing MS (PRMS)
PRMS is a less common form of MS that combines features of both primary progressive and relapsing-remitting MS. Individuals with PRMS experience a steady progression of symptoms with occasional relapses and periods of remission.
It's crucial to remember that every person's experience with MS is unique, and the category of the illness may alter with time. Furthermore, there exist diverse disease-modifying therapies (DMTs) that aid in symptom management and decelerate the advancement of the illness. Treatment regimens are frequently customized based on the individual's unique MS type and stage. To properly monitor and manage their condition, people with MS must collaborate closely with medical specialists.
III. PATHOLOGY
Although the precise etiology is unknown, it is thought to have both acquired and hereditary contributing factors. An infectious agent (e.g. EBV), or at least a catalyst, has long been suggested due to the geographic dispersion and occurrence of clusters of patients; however, no agent has yet been clearly verified. Further research has not supported the idea put forth by certain authors that "chronic cerebrospinal venous insufficiency" can either cause or worsen MS.
In the initial phase of multiple sclerosis, there is little to no axonal degeneration due to oligodendrocyte loss; however, in later stages, axonal degeneration is thought to be the consequence of a cell-mediated autoimmune reaction against one's own myelin components. Demyelination occurs in discrete perivenular foci, termed plaques, which range in size from a few millimeters to a few centimeters.
Each lesion goes through three pathological stages:
- Early Acute Stage: These are active plaques with symptoms as active myelin breakdown. Also, they are mostly pink in color and swollen.
- Subacute Stage: In these case plaques are paler in color or chalky. These are seen as abundant macrophages.
- Chronic Stage: These are also known as inactive plaques or gliosis. They are also little in size or mostly no myelin breakdown. Color is grey/translucent. Finds gliosis with associated volume loss.
IV. SEQUENCE UTILITY
A. T1
Defective tyres, especially those with worn-out treads or inadequate tread depth, have reduced traction. This loss of traction can result in poor grip on the road, particularly in wet or slippery conditions, leading to skidding and increased chances of accidents.
Typically, lesions range from iso- to hypointense (T1 black holes). There could be several little hypointense lesions at the callososeptal interface (Venus necklace), or the corpus callosum could just seem thinner. Hyperintense lesions are linked to progressive illness and brain shrinkage.
B. T2
Usually, lesions are really severe. Around acute lesions, edema is frequently present.
C. SWI
Central vein sign: at higher field strengths most plaques have been shown to be perivenular (at 3 T, 45% of lesions; at 7 T, 87% of lesions)
D. FLAIR
Usually, lesions are really severe. The ependymal dot-dash sign 16 is an extremely early indication. Dawson's fingers are created when they propagate centrifugally along the medullary venules and are placed in a triangle arrangement perpendicular to the lateral ventricles (extending radially outward - best seen on parasagittal imaging). T2 is more sensitive to infratentorial lesions, whereas FLAIR is more sensitive than T2 in the identification of juxtacortical and periventricular plaques.
E. T1 C+ (Gd)
Active lesions exhibit improvement. Enhancement is frequently lacking in the periphery.
F. DWI/ADC
There are two possible ADCs for active plaques: high and low (increased or decreased diffusion). 10 Morphologically also usually an open ring.
G. PD
When T2W scans are unable to show cervical spinal cord MS lesions, PD images are more effective at identifying them.
H. MR Spectroscopy
Reduction of NAA peaks inside plaques is the most typical and noteworthy observation. In the acute pathologic phase, there is a rise in choline and lactate.
I. Double inversion recovery (DIR)
A pattern that improves plaque delineation by suppressing both CSF and white matter signal.
V. MACHINE LEARNING FOR MULTIPLE SCLEROSIS DETECTION
Fiorini et al. [10] developed a machine learning algorithm to evaluate clinical data and identify the MS disease course. Making a distinction between benign and advancing structures was the goal. Ordinary least squares (OLS) regularized least squares (RLS), logistic regression (LR), K-nearest neighbors (KNN), and linear SVM were the classifiers that were employed. First, 457 patients provided 91 attributes for collection. The median was then used to impute missing data. The dataset features were then normalized using a min-max scaling technique to fit them within the [0:1] interval. When the L1L2 feature selection was combined with the OLS algorithm, the highest accuracy of 78.32% was achieved. In addition, the greatest F1-score of 70.2% was obtained utilizing the RLS algorithm with L1L2 feature selection.
Similar to this, Sarbaz et al. [11] sought to create a decision support system (DSS) that uses a straightforward, noninvasive technique to identify MS patients who depend on balance disorders. In that study, 20 healthy controls and 14 MS patients were enrolled. Every participant had a marking placed between their eyebrows on their forehead. After then, participants were videotaped for three minutes while they stood in front of a dark backdrop. We used an image processing method to study and assess the relocation of these markers. Using a "tan-sigmoid" transfer function, an ANN was employed. The process of extracting features involved identifying the characteristics that demonstrated a substantial difference between the MS patients and the healthy controls.
The accuracy of the ANN was 92.35%. In addition, the researchers created a different DSS with an accuracy of 84.8% that detects individuals who may have MS in the future. It was advised that these individuals, who were categorized as being in this intermediate state, avoid any situations that could aggravate their MS and take part in activities that could delay the onset of the condition. More specifically, it was advised that they minimize stress, stay away from industrial and environmental pollutants, and take the prescribed dosages of vitamin D.
Ettema et al. [12] investigates the efficacy of an electronic nose (eNose) in identifying MS using exhaled breath analysis. This technique was used on 129 healthy controls and 124 MS patients with a verified MS diagnosis. All subjects breathed into the AeonoseTM for five minutes at a time. The AeonoseTM diagnostic test instrument can be used to identify the volatile organic chemicals in exhaled breath. The ability of AeonoseTM to discriminate between MS patients and healthy control volunteers was examined. Moreover, data on exhaled air was used to train an ANN. Using a subset of MS patients without prescriptions for MS drugs, a second prediction model was developed. Based on the ANN model, there was a 75% sensitivity and 75% specificity between MS patients and healthy controls.
Using supervised machine learning methods like random forests, Lötsch et al. [13] suggested developing a sophisticated classifier for serum lipid biomarkers. 403 people were used to train the biomarker based on Bayesian statistics to determine if they had MS or were in good health. After collection, preprocessing was done on their clinical dataset. Additionally, the most essential features were extracted using RF. With the whole feature set, the RF classifier was trained to 100% sensitivity, specificity, and accuracy. Nonetheless, a discrepancy in age between MS patients and healthy participants was noted, and there was an imbalance in the data among classes. Similarly, Martynova et al. [14] intended to establish blood and CSF cytokine-based markers for MS diagnosis from a panel of 45 cytokines. Twenty-five healthy controls and 101 MS patients' CSF were collected. Cytokines were evaluated utilizing multiplex immunoassay. Additionally, using specific serum and CSF cytokines, five machine learning models—KNN, DT, XGB (XG Boost), Gaussian naïve Bayes (gNB), and RF—were developed to diagnose MS and categorize patients into PPMS, SPMS, and RRMS. Based on ANOVA and Pearson correlation coefficient scores, the features that were used as inputs to the machine learning models were chosen; in CSF and serum, these features represented changes in 22 and 20 cytokines, respectively. Using a randomized sample of five biomarkers, the overall accuracy of MS diagnosis was ≥92%. Santiago et al.'s [16] goal was to use multifocal visual evoked potentials (mfVEPs) to categorize people into the various stages of MS. Ninety-six people were included in the dataset; they were divided into four groups: patients with confirmed multiple sclerosis (MS), patients with CIS, and healthy controls. The KNN algorithm was used to build both the hierarchical classifier (HC) and the flat multiclass classifier (FMC) that were suggested by the study. In this technique, the individuals' eyes are first classified based on their mfVEP recordings, and then the diagnosis is made. With classification accuracy for subjects and eyes of 74% and 95%, respectively, the HC achieved the highest results. Similar to this, Yperman et al. [17] suggested an additional method that uses an LR classifier and an RF classifier with 100 DTs and balanced class weights to predict how MS patients' disabilities will progress after two years. EPs from the Rehabilitation & MS Center in Overpelt, Belgium were used in the investigation.
The MEPs of 642 patients were examined by the writers. From these MEPs, they retrieved a vast amount of time-series information. The Boruta approach and mutual knowledge with the target were used to identify the best features. AUC of 0.75 ± 0.07 was the best result obtained by the RF. The goal of Solana et al.'s research [18] was to create a model that could use structural brain connection traits to distinguish between people with MS and healthy controls. In order to construct an SVM with k-fold cross validation, they determined 42 features from the node strength and local efficiency properties that best characterized the two groups. In this investigation, 188 MS patients and 45 healthy people were gathered from the MS Unit of the Hospital Clinic of Barcelona. Random undersampling was utilized for the majority class. Their approach produced accuracy values of 74.84% for node strength and 77.15% for local efficiency. According to their findings, MS patients can be distinguished from healthy controls based on central network features of susceptible nodes. Kawahara [19] sought to use aspects of the spinal cord to predict MS impairment. To extract novel features, they used MRI and spinal cord segmentation that are associated with the clinical status. They applied a variety of regression models, including non-linear non-parametric RFs, multiple LR models, and simple LR models, using the retrieved features. They looked at the feature data that was connected to the clinical status in order to determine whether traits were useful biomarkers. The greatest results and an improvement over clinical prediction about spinal cord volume were obtained by measuring the distance between the cord's border feature and center-of-mass. The root mean square error (RMSE) and mean absolute error (MAE) of the RF were both the lowest at 0.293 and 0.353
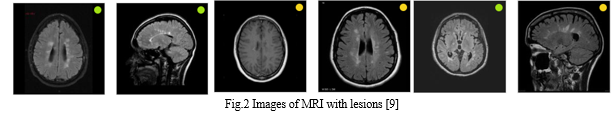
Ek¸si et al. [20] created an ANN model to distinguish MS lesions from low-grade brain malignancies. Brain tumors with a strong correlation to multiple sclerosis, such as oligoastrocytoma and gliomatosis cerebri, were not included in the study [21]. In addition, the dataset's sample size is little. Sarbaz et al.'s [11] diagnosis involved watching participant recordings while they were walking and keeping an eye on their balance using an infrared marker placed on their forehead. Although the study produced noteworthy results, the limited dataset may have contributed to overfitting. Two investigations were carried out by Dorado et al. to diagnose MS. In the first investigation [22], a sample of 21 individuals was employed to provide multifocal ERG data for diagnosis. Apart from the limited dataset, there was a bias in the samples towards MS. In the second investigation, Dorado et al. [23] examined retinal alterations using OCT data to diagnose MS. To train the CNN model, 96 patients were included in the sample. Because the CNN model needs a sizable dataset to be properly trained, data augmentation was done. Even though the suggested CNN model produces notable outcomes, data augmentation might occasionally cause the model to overfit. Both investigations used a short dataset and excluded all patient samples with additional ocular disorders, while achieving 100% specificity. In a similar vein, Azarmi et al. [24] reported a 100% specificity rate, but their study only included 20 patients from an Iranian hospital. The study employed an SVM and the patients' fMRI data. Some studies do prognosis or differentiate between the many kinds of MS, such as RRMS, PPMS, and SPMS, in addition to the diagnosis. Although Cattani et al. [25] attained a 99.78 accuracy rate in categorizing various forms of MS, there is a significant imbalance in that study. For patients with RRMS, Zurita et al. [26] suggested a classification approach. The model's performance did not differ significantly amongst patients with varying degrees of impairment. SVM is the most often used machine learning algorithm for MS diagnosis, followed by RF. Nonetheless, RF is the algorithm that performs the best. CNN is the most widely utilized and performs the best among DL methods. Furthermore, although some research relied on clinical data to diagnose the illness, most of the studies used datasets made up of MRI scans. The sizes of the employed datasets varied from 10 to 9390 instances. Nevertheless, the amount of the dataset utilized in several of the investigations was not stated. A summary of the frequently employed ML and DL methods from the earlier investigations may be found in Figure 2.

VI. OPPORTUNITIES
A. Early Detection and Prediction:
Machine learning models can analyze diverse data sources, including imaging and clinical records, to identify subtle patterns indicative of early-stage multiple sclerosis. Early detection facilitates timely intervention and improved management.
- Preclinical Marker Identification: Preclinical data, including as genetic characteristics, lifestyle details, and results from early imaging studies, can be analyzed by machine learning models to detect signs that point to a higher risk of multiple sclerosis. This makes early intervention techniques possible.
- Finding Biomarkers: By sifting through large datasets, machine learning algorithms can find modest indicators linked to the early phases of multiple sclerosis. These biomarkers could be changes in protein levels, genetic abnormalities, or imaging features that indicate the development of a disease.
- Predictive Analysis Using Clinical Information: By incorporating clinical data into machine learning models, such as patient demographics, history, and initial symptoms, predictive algorithms can be created. Based on early indicators, these models are able to predict an individual's risk of acquiring multiple sclerosis.
- Finding Biomarkers: Machine learning algorithms are able to recognize and rank putative multiple sclerosis biomarkers. These biomarkers, which aid in more precise and effective identification, may comprise imaging features, clinical factors, or molecular signs.
- Telemedicine and Real-time Monitoring: Wearables and telemedicine platforms allow for real-time patient monitoring thanks to machine learning. Constant data streams feed into dynamic models that enable early detection of changes in illness condition and prompt, proactive action.
- Automated Segmentation of Lesions: Machine learning systems are quite good at automatically dividing up MS lesions from imaging data. This automation expedites the diagnostic procedure, lessens the burden for radiologists, and improves uniformity in lesion identification.
B. Personalized Medicine:
The creation of customized models that take into account a patient's genetics, characteristics, and reaction to treatment is made possible by machine learning. Adapting treatment and diagnostic plans to the unique requirements of every patient improves overall effectiveness.
- Using genetic Profiling: By examining an individual's genetic composition, genetic variants related to MS susceptibility, illness progression, and treatment response can be identified. Decisions on individualized treatment are guided by this data.
- Identification of Biomarkers: Determining the molecular and imaging indicators unique to a person's MS profile facilitates more precise diagnosis, prognosis, and therapy decision-making. Serum markers, imaging characteristics, and genetic markers are a few examples of these biomarkers.
- Subtyping of Diseases: Personalized medicine acknowledges the variability of multiple sclerosis and endeavors to categorize individuals into distinct subgroups according to their unique disease attributes. This method enables customized treatment regimens that take into account the special characteristics of every subtype.
- Treatment Reaction Forecast: Examining variables including genetic markers, biomarkers, and clinical information aids in forecasting a person's possible reaction to various disease-modifying treatments (DMTs). This makes it possible to choose the therapies that are both most successful and well-tolerated.
- Customized Rehab Initiatives: Personalized medicine includes more than just medication regimens; it also includes specially designed programs for rehabilitation. Specific symptoms and functional constraints are addressed through individualized physical therapy, occupational therapy, and cognitive therapies.
- Environmental and Lifestyle Factors to Consider: Personalized medicine takes lifestyle and environmental factors into account when creating treatment programs since it recognizes their impact on multiple sclerosis. Every patient receives specific recommendations for nutrition, exercise, stress reduction, and other lifestyle changes.
C. Integration of Multi-Modal Data in Multiple Sclerosis
In the context of multiple sclerosis (MS), integration of multi-modal data refers to the thorough examination and blending of many information types, such as clinical, imaging, genetic, and molecular data. By integrating knowledge from multiple sources, this method seeks to offer a comprehensive view of the illness, enabling more precise diagnosis, prognosis, and customized treatment plans.
- Clinical Data: Clinical information must include patient demographics, medical history, symptomatology, and information on the course of the disease. Enhancing the contextual understanding of the patient's overall health status is possible through integration with various modalities.
- Imaging Data: An overview of the central nervous system's structure, function, and molecular makeup can be obtained by using a variety of imaging modalities, including positron emission tomography (PET), optical coherence tomography (OCT), and magnetic resonance imaging (MRI). Integrating these imaging datasets enables a more thorough evaluation of MS pathology.
- Genetic Information: Hereditary profiling sheds light on a person's propensity for multiple sclerosis (MS) as well as possible hereditary variables affecting the severity of the illness and how well it responds to therapy. Combined with clinical and imaging data, genetic data adds to a more individualized picture of the disease.
D. Automated Lesion Segmentation in Multiple Sclerosis
The term "automated lesion segmentation" describes the process of identifying and defining lesions in medical imaging data, such as magnetic resonance imaging (MRI), linked to multiple sclerosis (MS), using computer algorithms, namely machine learning and image processing techniques. By streamlining the study of lesions connected to multiple sclerosis, this automated method seeks to produce accurate and timely results.
- Machine Learning Algorithms: Lesion segmentation is a frequent application of supervised machine learning methods, such as random forests, support vector machines (SVMs), and convolutional neural networks (CNNs). These algorithms automatically detect lesions in new images by picking up patterns from labeled training data.
- Image Processing Techniques: Lesion segmentation frequently makes use of conventional image processing methods like thresholding, region growth, and morphological processes.
- Deep Learning Architectures: Automating lesion segmentation has proven to be a surprising success for deep learning systems, especially CNNs. These architectures are able to recognize complicated patterns linked to multiple sclerosis lesions by directly learning hierarchical features from raw imaging data.
- Multi-Modal Integration: Lesion segmentation accuracy is improved by combining data from various imaging modalities, such as fluid-attenuated inversion recovery (FLAIR) MRI sequences, T1-weighted, and T2-weighted MRI sequences. With multi-modal integration, MS pathology is shown more thoroughly.
- Atlas-Based Segmentation: Aligning a patient's MRI data with an already-existing anatomical atlas is known as atlas-based segmentation. After that, lesions are located using the atlas's departures from the norm. This method works especially well for finding tiny or inconspicuous lesions.
- Semi-Automated Approaches: Semi-automated approaches are those that combine human intervention with automated algorithms. To increase the accuracy of the lesion segmentation findings produced by automated algorithms, clinicians might offer suggestions or changes.
E. Quantitative Imaging Analysis in Multiple Sclerosis
The practice of extracting objective and numerical information from medical imaging data, especially magnetic resonance imaging (MRI), using sophisticated image processing techniques and quantitative metrics is known as quantitative imaging analysis in multiple sclerosis (MS). With this method, MS-related pathology should be more precisely and in-depthly characterized, which will help with diagnosis, prognosis, and treatment monitoring.
- Quantification of Lesion: The quantity, size, and location of MS lesions in brain and spinal cord pictures are measured using automated methods. Quantification of lesions yields important insights about the prevalence and course of the disease.
- Volumetric Evaluation: Measurements of the volume of various brain structures, such as white matter, gray matter, and particular regions of interest, are made using volumetric analysis. Variations in volumetric measurements over time may point to the expansion or atrophy of specific brain areas.
- Metrics for Diffusion Tensor Imaging (DTI): DTI measures the diffusion of water molecules to provide information about the microstructural organization of white matter. Axonal damage and tissue integrity can be inferred from quantitative parameters acquired from DTI, such as mean diffusivity (MD) and fractional anisotropy (FA).
- Magnetic Resonance Spectroscopy (MRS): By measuring biochemical markers in the brain, MRS makes it possible to determine the quantities of metabolites. Changes in markers that indicate neuronal health and inflammation, such as N-acetylaspartate (NAA), creatine, and choline, can be found through quantitative analysis of MRS data.
- Cortical Thickness and Surface Area Analysis: Measurements of cortical thickness and surface area shed light on cortical atrophy, a prevalent symptom of multiple sclerosis. The disease's precise afflicted regions can be identified with the use of quantitative cortical analysis.
- Dynamic Contrast-Enhanced MRI (DCE-MRI): In order to measure perfusion, DCE-MRI tracks the movement of contrast chemicals through blood vessels. Information regarding blood flow, capillary permeability, and vascularization in MS lesions can be obtained through quantitative analysis of DCE-MRI data.
F. Big Data Analytics in Multiple Sclerosis
In the context of multiple sclerosis (MS), big data analytics entails the thorough examination of sizable and varied datasets, such as genetic data, imaging data, clinical records, and other pertinent sources. This strategy makes use of statistical methods, machine learning, and advanced analytics to improve patient care in multiple sclerosis and provide important insights.
- Integration of Multi-Modal Data: Big data analytics combines data from multiple sources, such as genetic information, imaging investigations (MRI, CT scans), clinical records, and patient-reported results. A comprehensive understanding of MS is made possible by the integrated analysis of multi-modal data, which facilitates better decision-making.
- Machine Learning Algorithms: To find patterns, connections, and prediction factors linked to MS, machine learning algorithms—including supervised and unstructured models—are applied to massive datasets. Making decisions about diagnosis, prognosis, and treatment can be aided by these algorithms.
- Predictive Analytics: Predictive analytics is a technique that makes use of past data to spot trends and forecast future events. Predictive analytics can be used in MS to help with individualized patient care by predicting the course of the disease, how well a patient responds to treatment, and the chance of relapses.
- Natural Language Processing (NLP): NLP techniques are utilized to extract meaningful information from unstructured clinical notes, reports, and literature. This enables researchers and healthcare providers to leverage a vast amount of textual data for analysis.
- Network Analysis: Network analysis explores the relationships and interactions between different factors in MS, such as genetic markers, clinical symptoms, and treatment responses. This approach helps identify key influencers and factors contributing to the complexity of the disease.
- Real-time Data Processing: Big data analytics enables real-time processing of streaming data, allowing for immediate analysis and decision-making. This is particularly valuable for monitoring patient health in real-time and making timely adjustments to treatment plans.
- Population Health Management: Big data analytics analyzes enormous datasets to find patterns, risk factors, and intervention opportunities in order to enhance population health management projects. Taking a population-level approach makes it easier to create public health initiatives for MS that work.
VII. CHALLENGES
A. Clinical and Radiological Heterogeneity
Developing machine learning models that generalize across the wide range of multiple sclerosis is difficult due to the disease's different clinical presentations and imaging features.
B. Dual-Domain Adaptation Model
Finding strong and trustworthy biomarkers for machine learning models is difficult due to our incomplete understanding of the underlying pathophysiology and course of multiple sclerosis. The interpretability of the model is hampered by the unclear causal links.
C. Multi-scale Defect Detection Network (MDDN)
Different imaging platforms, clinical settings, and institutions may have varying data quality, which can affect how well machine learning models perform. Ensuring data quality and standardizing data collecting techniques are difficult but necessary responsibilities.
D. Small and Imbalanced Datasets
Training and validating machine learning models for multiple sclerosis identification may be hampered by the scarcity of big, well-annotated datasets. An unbalanced class distribution could result in a biased model's output.
E. Ethical Considerations and Data Privacy
Concerns around data ownership, consent, and privacy are raised by the use of patient data to train machine learning algorithms. A fine balance must be struck between guaranteeing adequate data availability and putting strong privacy controls in place.
F. Overfitting and Model Complexity
Overfitting can happen when a model learns noise in the training data instead of real underlying patterns, especially in complicated models. Requiring a balance between generalizability and model complexity is essential for reliable multiple sclerosis identification.
G. Resource and Infrastructure Constraints
Deploying machine learning models for multiple sclerosis detection may require significant computational resources and infrastructure. This poses challenges, especially in resource-constrained healthcare settings.
H. Clinical Adoption and Integration
Getting healthcare workers to accept machine learning models into clinical workflows can be difficult. It is imperative to tackle concerns pertaining to trust, interpretability, and smooth interaction with current systems.
Conclusion
The goal of this work was to present a thorough analysis of the earlier advancements made by scientists in the automated diagnosis of multiple sclerosis. The medical applications for MS diagnosis have improved with the use of ML algorithms and AI technologies. In this research, we analyzed various machine learning algorithms used for MS diagnosis and found that SVM was the most widely used methodology, followed by CNN and RF. In addition, we talked about the difficulties and possibilities associated with MS diagnosis in order to identify areas in which practitioners and researchers may enhance their methods. Any and all of the research opportunities found in this study can be pursued in the future. Nonetheless, the viewpoint of the current authors seeks to further knowledge about MS in many settings. In other words, real datasets will be used to inform ML algorithms for disease diagnosis and prognosis.These could include clinical, lab, and demographic data as well as machine or radiological data (patient monitoring, etc.). Additionally, novel traits will be investigated in order to find possible predictors.
References
[1] Reich DS, Lucchinetti CF, Calabresi PA. Multiple Sclerosis. N Engl J Med. 2018;378(2):169-180. [2] Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. [3] Erbayat Altay E, Fisher E, Jones SE, Hara-Cleaver C, Lee JC, Rudick RA. Reliability of classifying multiple sclerosis disease activity using magnetic resonance imaging in a multiple sclerosis clinic. [4] Zhao Y, Guo S, Luo M, et al. A level set method for multiple sclerosis lesion segmentation. Magn Reson Imaging. 2018; 49:94-100. [5] Ghribi O, Sellami L, Ben Slima M, Ben Hamida A, Mhiri C, Mahfoudh KB. An advanced MRI multi-modalities segmentation methodology dedicated to multiple sclerosis lesions exploration and differentiation. IEEE Trans Nanobioscience. 2017;16 [6] Zhang Y-D, Zhang Y, Phillips P, Dong Z, Wang S. Synthetic minority oversampling technique and fractal dimension for identifying multiple sclerosis. Fractals. 2017; 25:1740010. [7] Xueyan W, Mason L. Multiple sclerosis slice identification by Haar wavelet transform and logistic regression. Paper presented at: Advances in Materials, Machinery, Electrical Engineering (AMMEE 2017); June 2017. [8] Nayak DR, Dash R, Majhi B. Pathological brain detection using curvelet features and least squares SVM. Multimed Tools Appl.2018;77(3):3833-3856. [9] Jasperse, B., Barkhof, F. (2023). Machine Learning in Multiple Sclerosis. In: Colliot, O. (eds) Machine Learning for Brain Disorders. Neuromethods, vol 197. Humana, New York, NY. https://doi.org/10.1007/978-1-0716-3195-9_28 [10] Fiorini, S.; Verri, A.; Tacchino, A.; Ponzio, M.; Brichetto, G.; Barla, A. A machine learning pipeline for multiple sclerosis course detection from clinical scales and patient reported outcomes. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS 2015, Milan, Italy, 25–29 August 2015. [11] Sarbaz, Y.; Pourakbari, H.; Vojudi, M.H.; Ghanbari, A. Introducing a decision support system for multiple sclerosis based on postural tremor: A hope for separation of people who might be affected by multiple sclerosis in the future. Biomed. Eng. Appl. Basis Commun. 2017, 29, 1750046. [12] Ettema, A.R.; Lenders, M.W.P.M.; Vliegen, J.; Slettenaar, A.; Tjepkema-Cloostermans, M.C.; de Vos, C.C. Detecting multiple sclerosis via breath analysis using an eNose, a pilot study. J. Breath Res. 2021, 15, 027101. [13] Lötsch, J.; Schiffmann, S.; Schmitz, K.; Brunkhorst, R.; Lerch, F.; Ferreiros, N.; Wicker, S.; Tegeder, I.; Geisslinger, G.; Ultsch, A.Machine-learning based lipid mediator serum concentration patterns allow identification of multiple sclerosis patients with high accuracy. Sci. Rep. 2018, 8, 14884. [14] Martynova, E.; Goyal, M.; Johri, S.; Kumar, V.; Khaibullin, T.; Rizvanov, A.A.; Verma, S.; Khaiboullina, S.F.; Baranwal, M. Serum [15] and cerebrospinal fluid cytokine biomarkers for diagnosis of multiple sclerosis. Mediat. Inflamm. 2020, 2020, 2727042. [16] De Santiago, L.; Morla, E.M.S.; Ortiz, M.; López, E.; Usanos, C.A.; Alonso-Rodríguez, M.C.; Barea, R.; Cavaliere-Ballesta, C.; Fernández, A.; Boquete, L. A computer-aided diagnosis of multiple sclerosis based on mfVEP recordings. PLoS ONE 2019, 14, e0214662. [17] Yperman, J.; Becker, T.; Valkenborg, D.; Popescu, V.; Hellings, N.; Wijmeersch, B.V.; Peeters, L.M. Machine learning analysis of motor evoked potential time series to predict disability progression in multiple sclerosis. BMC Neurol. 2020, 20, 105. [18] Solana, E.; Martinez-Heras, E.; Casas-Roma, J.; Calvet, L.; Lopez-Soley, E.; Sepulveda, M.; Sola-Valls, N.; Montejo, C.; Blanco, Y.; Pulido-Valdeolivas, I.; et al. Modified connectivity of vulnerable brain nodes in multiple sclerosis, their impact on cognition and their discriminative value. Sci. Rep. 2019, 9, 20172. [19] Kawahara, J. Spinal Cord Segmentation and Disability Prediction in Multiple Sclerosis Using Novel Optimization and Machine Learning Methods. Ph.D. Dissertation, Vancouver Island University, Nanaimo, BC, Canada, 2013. [20] Ek¸si, Z.; Özcan, E.M.; Çak?ro ?glu, M.; Öz, C.; Arala¸smak, A. Differentiation of multiple sclerosis lesions and low-grade brain tumors on MRS data: Machine learning approaches. Neurol. Sci. 2021, 42, 3389–3395. [21] Plantone, D.; Renna, R.; Sbardella, E.; Koudriavtseva, T. Concurrence of multiple sclerosis and brain tumors. Front. Neurol. 2015, 6, 6–9. [22] 66.López-Dorado, A.; Pérez, J.; Rodrigo, M.J.; Miguel-Jiménez, J.M.; Ortiz, M.; de Santiago, L.; López-Guillén, E.; Blanco, R.; Cavalliere, C.; Morla, E.M.S.; et al. Diagnosis of multiple sclerosis using multifocal ERG data feature fusion. Inf. Fusion 2021, 76, 157–167 [23] 101.López-Dorado, A.; Ortiz, M.; Satue, M.; Rodrigo, M.J.; Barea, R.; Sánchez-Morla, E.M.; Cavaliere, C.; Rodríguez-Ascariz, J.M.; Orduna-Hospital, E.; Boquete, L.; et al. Early diagnosis of multiple sclerosis using swept-source optical coherence tomography and convolutional neural networks trained with data augmentation. Sensors 2022, 22, 167. [24] 51. Azarmi, F.; Miri Ashtiani, S.N.; Shalbaf, A.; Behnam, H.; Daliri, M.R. Granger causality analysis in combination with directed network measures for classification of MS patients and healthy controls using task-related fMRI. Comput. Biol. Med. 2019, 115, 103495. [25] 106. Karaca, Y.; Cattani, C.; Moonis, M. Comparison of deep learning and support vector machine learning for subgroups of multiple sclerosis. Lect. Notes Comput. Sci. 2017, 10405, 142–153. [26] 54. Zurita, M.; Montalba, C.; Labbé, T.; Cruz, J.P.; Dalboni da Rocha, J.; Tejos, C.; Ciampi, E.; Cárcamo, C.; Sitaram, R.; Uribe, S.Characterization of relapsing-remitting multiple sclerosis patients using support vector machine classifications of functional and diffusion MRI data. NeuroImage Clin. 2018, 20, 724–730. [27] Aslam N, Khan IU, Bashamakh A, Alghool FA, Aboulnour M, Alsuwayan NM, Alturaif RK, Brahimi S, Aljameel SS, Al Ghamdi K. Multiple Sclerosis Diagnosis Using Machine Learning and Deep Learning: Challenges and Opportunities. Sensors (Basel). 2022 Oct 16;22(20):7856. doi: 10.3390/s22207856. PMID: 36298206; PMCID: PMC9609137. [28] https://doi.org/10.1002/ima.22492
Copyright
Copyright © 2024 Fathimath Nihala T, Dr. N. Syed Siraj Ahmed. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET58117
Publish Date : 2024-01-20
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

