Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Study of Nausea and Vomiting can be Symptoms of Many Different Conditions
Authors: Dr. Chilakalapudi Meher Babu
DOI Link: https://doi.org/10.22214/ijraset.2024.63791
Certificate: View Certificate
Abstract
Before the twentieth century, drugs used for the treatment of diseases were obtained from natural sources like plants, animals, microorganisms, and minerals, and among them, plants were the major source of natural drugs. At present, most of the drugs are obtained from synthetic and biosynthetic sources. The nature was once served as the source of all medicaments and plants, especially the higher plants have been continuing the service since antiquity as important sources of novel compounds useful directly as medicinal agents, as model compounds for synthetic or semi-synthetic structure modifications and optimization, as biochemical and/or pharmacological probes, and as sources of inspiration for generations of synthetic organic medicinal chemists. Plant-derived compounds which have recently under- gone development include the anti-cancer agents, taxol and camptothecin, the Chinese antimalarial drug, artemisinin, and the East Indian Ayurvedic drug, for-skolin. These and many other examples serve to illustrate the continuing value of plant-derived secondary metabolites as viable compounds for modern drug devel- opment (Newman et al. 2003; Newman and Cragg 2007). Natural sources are most primitive and abundant. Drugs obtained from the natural sources include a. Plant, b. Animal, c. Microbial, d. Marine, e. Mineral, and f. Geographical sources. Plant, Animal, Microbial and Marine may be put under common heads—the biological sources.
Introduction
I. INTRODUCTION OF VOMITING
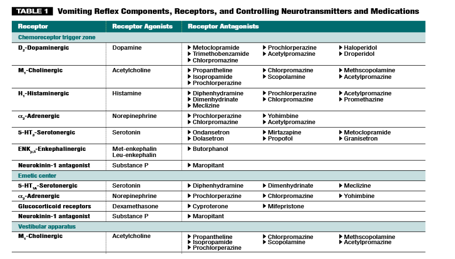
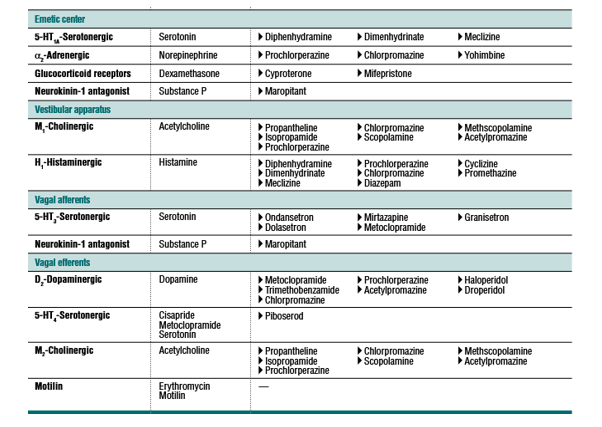
Vomiting is the forceful expulsion of stomach contents through the mouth, caused by humoral stimulation of the chemoreceptor trigger zone (CRTZ) or neural stimulation of the emetic center. The CRTZ is activated and controlled by neurotransmitter manipulation at the receptor level. Clinical signs preceding vomiting may include ptyalism, tachycardia, depression, hiding, and yawning. Gastritis, gastrointestinal ulceration, pancreatitis, motion sickness, uremia, chemo-therapy, and drug administration are common initiating causes of vomiting. This article reviews the anatomic and physiologic aspects of the vomiting reflex and its neurotransmitters, associated receptors, and rational management.
II. ANATOMY
The act of vomiting is composed of three phases: nausea, retching, and expulsion of proximal duodenal and gastric contents. Nausea is the conscious recognition of sub-conscious excitation in an area of the medulla that is closely associated with the vomiting center. This excitation is caused by irritative impulses coming from the gastroin-testinal tract, lower brain, or cerebral cortex.Ptyalism, tachycardia,nervousness, hiding or seeking attention, shivering, and yawning are all characteristic signs of nausea triggered by general activation of the sympathetic and parasympa-thetic branches of the autonomic nervous system. Hypersalivation stimulates swallowing, which stimu-lates relaxation of the gastroesopha-geal sphincter. The bicarbonate-rich saliva secreted by the salivary glands in the mouth lubricates the esopha-gus and helps neutralize the stomach’s acidic environment before vomiting. 8,13 Before retching, abo-ral gastric and esophageal motility diminishes and the lower esopha-geal and pyloric sphincters relax. Retching is the second phase of vomiting and begins with the on setof a retrograde giant contraction.20,21 This contraction is a single-phase, ret-rograde, peristaltic motion that emp-ties the proximal duodenal contents into the stomach.20–22 It is followed by deep inspiratory movements, force-ful contractions of the abdominal muscles and diaphragm, and closure of the glottis. These actions produce negative intra thoracic pressure and positive intra abdominal pressure, facilitating the movement of gastric contents into the esophagus. Before expulsion, the respiratory center is inhibited and the nasopharynx and glottis close to prevent pulmonary aspiration and nasal regurgitation of the gastric contents. The third and last phase of vomiting is the expul-sion of stomach contents through the mouth.
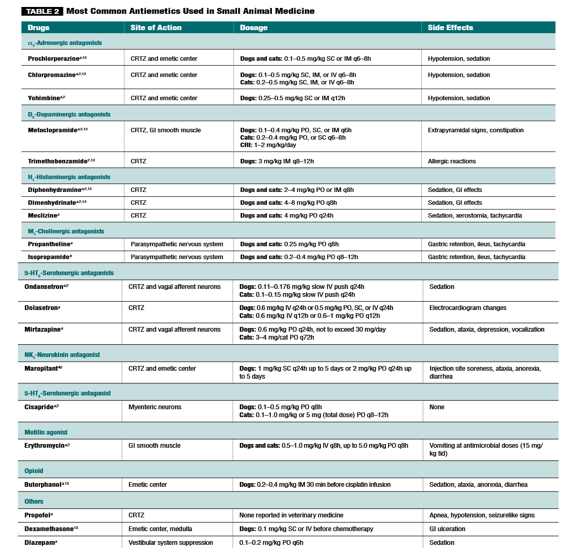
III. ANTIHISTAMINES
Antihistamines can intercept cholinergic and histaminic nerve transmission responsible for vestibular stimulation of the vomiting center. Drugs in this classification include diphen-hydramine, dimenhydrinate, and meclizine. These drugs display H1 –antihistaminergic properties and are mainly used to control the clinical signs of motion sickness. Mild seda-tion, xerostomia, and drowsiness are some of the adverse effects. Meclizine can be terato-genic if administered at high doses. Cats do not have histamine receptors in the CRTZ, and antihistaminic drugs do not control their vomiting.
IV. SEROTONIN ANTAGONISTS
Serotonin antagonists are specific inhibitors of 5-HT-serotonergic receptors. They control vomiting by acting on receptors located on the periphery of vagal nerve terminals and centrally on the CRTZ. These receptors are normally stimulated by serotonin released from the entero chromaffin cells of the small intestine in response to damage to the gastro-intestinal mucosa. Ondansetron, a member of this class of antiemetic drugs, has been shown to control vomiting in dogs and is used in dogs receiving radiation and chemotherapy when metoclopramide and other antiemetics fail to control vomiting. Dolasetron, another member of this group, acts on recep-tors in the CRTZ. 25 Both of these drugs are used extensively in human medicine, and they seem to be safe antiemetic alternatives in veterinary medicine. However, they are not effective in controlling vomiting caused by motion sickness. Side effects of these drugs that have been reported in people include electrocardiographic changes, including PR and QT prolongation and
QRS widening, that are believed to be caused by sodium channel blockage by dolasetron metabolites. Diarrhea, headache, dizziness, and musculoskeletal pain have been reported as well. These medications can be expensive.
V. OTHER DRUGS
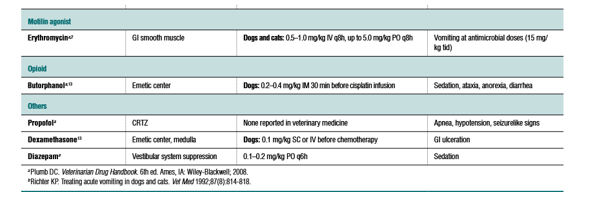
Other drugs used to control vomiting centrally include yohimbine, diazepam, dexamethasone, propofol, and mirtazapine. Yohimbine, a pure α2 -adrenergic antagonist, is a very potent antiemetic used in dogs and cats. It may cause CNS excitement, excessive sedation, muscle tremors, tachypnea, ptyalism, and hyperemic mucous membranes. Diazepam relieves nausea and vomiting in people. Studies with animal models and clinical trials in human medicine suggest that this drug suppresses the vestibular system. The antiemetic properties of corticosteroids are incompletely understood, but their mechanism involves the activation of glucocorticoid receptors in the medulla, especially the emetic center in cats. Dexamethasone has been shown to be useful in controlling chemotherapy-associated nausea and vomiting in human patients and dogs. Propofol, an alkylphenol derivative, is used as an antiemetic in people with chemotherapy-asso-ciated nausea and vomiting that is unresponsive to serotonin antagonists or dexamethasone. It has been proposed that its antiemetic mechanism involves reduction of the serotonin concentration in the CRTZ via γ-aminobutyric acid activity and 5-HT3 serotonin receptor antagonism. Mirtazapine is a piperazinoazepine drug used as an antidepressant in people. It antagonizes central presynaptic α2 -receptors and blocks serotonin receptors.50 It is a weak 5-HT1 sero-tonin receptor antagonist, a potent 5-HT2 and 5-HT3 serotonin receptor antagonist, and an H1-histamine antagonist.50 It is used to control chemotherapy-associated nausea and vomiting in humans and, more recently, in small animals.
VI. TREATMENT OF COMMON VOMITING CONDITIONS
Box 1 lists several conditions and diseases that commonly cause vomiting. Gastritis or Gastric Ulceration Treatment to manage vomiting caused by gastritis or gastric ulceration must include proper fluid therapy and gastric mucosal protection. Many clinicians use broad-spectrum antiemetics because they cover local and peripheral receptors. Chlorpromazine, serotonin antagonists, and metoclopramide are good options. Maropitant seems to work extremely well in dogs. If vomit-ing is associated with gastrointestinal ulceration due to NSAID administration, therapy with misoprostol, a prostaglandin E1 (PGE) analog, may be effective in controlling both the ulcerative lesion and vomiting as a secondary problem. Proton pump inhibitors and H2 –histamine antagonists provide more complete inhibition of gastric acid secretion in severe cases of ulceration. If Helicobacter spp are the underlying cause of ulceration, appropriate antibiotic
therapy and antacids should relieve the clinical signs of the infection. Patients with neoplastic diseases often have gastrointestinal ulceration. Mast cell tumors of any stage, grade, and size can cause vomit- ing in dogs by increasing the plasma hista-mine concentration. Histamine acts on the CRTZ and the gastric mucosa. Mast cell tumor ulceration and its effects are treated with H 2 -histamine antagonists. Tumor size and his-tamine release in dogs are controlled with the administration of corticosteroids.
VII. PANCREATITIS
Pancreatitis causes ileus due to intestinal inflammation, resulting in direct afferent input to the vomiting center. Metoclopramide is the most common antiemetic used in these patients because it acts centrally and peripherally. In dogs, phenothiazines, 5-HT3 –serotonergic antagonists, and maropitant can be useful if metoclopramide fails to control vomiting Motion Sickness Motion sickness, or kinetosis, is generated from the vestibular apparatus. Studies in humans have revealed that motion sickness is caused by three mechanisms: (1) conflicting inputs from the visual and vestibular systems; (2) conflict-ing inputs from the two vestibular systems (the semicircular canals and the otolith organs); or (3) comparison of input from these systems with the individual’s expectations derived from previous experiences. Vomiting caused by motion sickness involves M1 –cholinergic and H1 -histaminergic receptors,2,11 and treatment should antagonize both receptors. Phenothiazines like chlorpromazine and prochlorperazine can antagonize both receptors at the same time, but diphenhydramine, dimenhydrinate, cyclizine, meclizine, and promethaz- ine are H1 -histamine blocking agents only, and they should be combined with a M1 –cholinergic receptor blocker for effective control of emetic signals originating from the vestibular apparatus. Maropitant prevents kinetosis in dogs by blocking the final common pathways of the vomiting reflex, including signals from the vestibular system.40 Scopolamine is a muscarinic M1 -cholinergic antagonist used to treat motion sickness, but results are not consistent.
VIII. UREMIA
Uremic toxins cause decreased gastrin clear-ance and irritate the gastrointestinal mucosa, resulting in ulcerative lesions and gastritis. When these toxins cross the blood–brain barrier, they stimulate central and peripheral receptors and activate D2 -dopaminergic recep-tors in the CRTZ. Dopamine antagonists like metoclopramide and chlorpromazine effectively block these receptors. Diuresis with appropriate fluid therapy and a proton pump inhibitor or H 2 –histaminergic antagonist helps relieve uremia by diminish-ing the secretion of hydrogen ions into the stomach, providing protection and promoting mucosal healing.
IX. GASTROINTESTINAL MOTILITY DISORDERS
Prokinetics—cisapride, metoclopramide, and erythromycin—should be used to control vom-iting due to nonobstructive delayed gastric emptying. These drugs exert their effects on different receptors. Cisapride, the most effective prokinetic agent available,11 lacks direct anti- emetic effects but stimulates 5-HT4 –serotonergic receptors. Metoclopramide’s antagonism of D2 -dopaminergic receptors enables it to stimu-late motility in areas where these receptors are present (the higher gastrointestinal tract, lower esophageal sphincter, stomach.
X. UNDETERMINED ETIOLOGY
Patients with vomiting of undetermined etiology must be treated with the safest approach pos-sible once systemic diseases (e.g., liver disease,renal disease, endocrine disease) have been ruled out. Patients that are uncomfortable from excessive vomiting or are at high risk for aspira-tion pneumonia and have not been exposed to a toxic agent should be treated with antiemetics when available. α2 -Adrenergic antagonists and D2 -dopaminergic receptors are first-line anti-emetics. Maropitant is a good alternative not only because it seems to block impulses in the final common pathways of the vomiting reflex but also because it is administered once daily, dogs seem to tolerate it fairly well, and, so far, adverse effects are minimal. 5-HT3 –serotonergic antagonists have become very popular over the past few years and have good results. The addi-tion of other drugs to antiemetic therapy should be considered if vomiting becomes refractory in these patients
XI. TREATMENT OF VOMITING
There are various vomiting treatments; with one-time vomiting typically considered to be quite serious. However, following an incident of vomiting, hydration is essential. Thus, individuals must consume plenty of water since they contain the necessary electrolytes to help in this situation.
Moreover, solid food can upset a sensitive stomach at this point. Thus, it is better to avoid such food at this point. Furthermore, medication can help to reduce or control vomiting. Apart from these, alternative remedies like consuming ginger, lemongrass oil, or bergamot are an effective vomiting solution. Additionally, dietary changes can also help in case of repeated vomiting.
Conclusion
1) Dry Heaves: Dry heaves are the type of vomit where the feeling is present, but nothing comes out. It is termed as non-productive vomit. 2) Blood-Streaked Vomit: Blood streaked vomiting causes a cut in the esophagus or stomach. Here, vomit comes out filled with blood, having red or dark-brown colour. 3) Coffee-Ground Vomit: Intestinal bleeding in the upper-gastro results in exposure of iron in the blood to the stomach acid. This acid oxides the iron and causes the vomit to resemble coffee grounds. It could be a sign of health issues like GERD, peptic ulcer, liver disease, etc. 4) Bile-Stained Vomiting: Bile vomiting is persistent vomiting following a meal. Moreover, bile reflux and bowel obstruction result in this vomit. Bile blends with food in the duodenum and when the small intestine is blocked, its substances expulse with the bile. Furthermore, following surgical removal of a gallbladder, gastric bypass surgery, etc. this reflux of bile takes place in the stomach and leads to this vomit. 5) Faecal Vomit: This type of vomiting occurs due to intestinal obstruction, or unusual connection between colon and stomach. As a result, an expulsion of fully or partially digested matter happens via the mouth. 6) Projectile Vomiting: Here, the contents of the stomach comes out in a massive force. Typically, it occurs following feeding.
References
[1] Tams TT. A diagnostic approach to vomiting in dogs and cats. Vet Med 1992;87(8):785-792. [2] Washabau RJ, Elie S. Antiemetic therapy. In: Kirk RW, Bonagura JD, eds. Kirk’s Current Veterinary Therapy XII Small Animal Practice. Philadel-phia: WB Saunders; 1995:679-684. [3] Andrews PLR, Rapeport WG, Sanger GJ. Neuropharmacology of emesis induced by anti-cancer therapy. Trends Pharmacol Sci 1988;9:334-341. [4] Johnson SE. Clinical pharmacology of antiemetics and antidiarrheals. Proc of the Kal Kan Waltham Symp Treat Small Anim Dis 1984;8:7-15. [5] Merrifield KR, Chaffee BJ. Recent advances in the management of nausea and vomiting caused by antineoplastic agents. Clin Pharm 1989;8:187-199. [6] Leib MS. Acute vomiting: a diagnostic approach and symptomatic management. In: Kirk RW, Bonagura JD, eds. Kirk’s Current Veterinary Therapy XI Small Animal Practice. Philadelphia: WB Saunders; 1995:583-587. [7] Burrows CF. Vomiting and Regurgitation in the Dog: A Clinical Perspec-tive. Lehigh, Pennsylvania. ALPO Pet Center; 1990:18-38. Viewpoints in Veterinary Medicine. [8] Guyton AC, Hall JE. Textbook of Medical Physiology. 9th ed. Philadel-phia: WB Saunders; 1996. [9] Adams HR. Veterinary Pharmacology and Therapeutics. 8th ed. Ames: Iowa State University Press; 2001. [10] Cunningham JG. Textbook of Veterinary Physiology. 3rd ed. Philadel-phia: WB Saunders; 1997 [11] Richter K. Approach to acute vomiting. Proc WVC 2004. Accessed January 2009 at vin.com/Members/Proceedings/Proceedings.plx?CID=wv c2004&PID=pr05345&O=VIN. [12] Simpson KW. Managing persistent vomiting. Proc ACVIM 2003. Ac-cessed January 2009 at vin.com/Members/Proceedings/Proceedings.plx?CID=acvim2003&PID=pr03873&O=VIN. [13] Strombeck DA, Guilford WG. Vomiting: pathophysiology and phar-macology control. In: Strombeck DA, Guilford WG, Center SA, et al, eds.Strombeck’s Small Animal Gastroenterology. 3rd ed. Philadelphia: WB Saunders; 1996:256-260. [14] Willard MD. Some new approaches to the treatment of vomiting. JAVMA 1984;184:590. [15] Miller AD, Leslie RA. The area postrema and vomiting. Front Neuroen-docrinol 1994;15(4):301-320. [16] Twedt DC. Vomiting. In: Ettinger SJ, Feldman EC, eds. Textbook of Veterinary Internal Medicine. 6th ed. Philadelphia: WB Saunders; 2005:132- 136. [17] Miller AD. Central mechanisms of vomiting. Dig Dis Sci 1999; 44(8suppl):31S-43S. [18] Miller AD, Nonaka S, Jakus J, et al. Modulation of vomiting by the medullary midline. Brain Res 1996;737(1-2):51-58. [19] Miller AD, Nonaka S, Jakus J. Brain areas essential or non-essential for emesis. Brain Res 1994;647(2):255-264. [20] Lang IM, Dana N, Medda BK, et al. Mechanisms of airway protection during retching, vomiting, and swallowing. Am J Physiol Gastrointest Liver Physiol 2002;283(3):G529-G536. [21] Sarna SK, Otterson MF. Small intestinal physiology and pathophysiology. Gastroenterol Clin North Am 1989;18(2):375-404. [22] Furukawa N, Hatano M. An acute experiment on retrograde intesti-nal peristalsis with emesis using decerebrated dogs. J Auton Nerv Syst 1998;70(1-2):56-65. [23] Peroutka SJ, Snyder SH. Antiemetics: neurotransmitter receptor bind-ing predicts therapeutic actions. Lancet 1982;1(8273):658-659. [24] Costall B, Naylor RJ. Neuropharmacology of emesis in relation to clini-cal response. Br J Cancer Suppl 1992;19:S2-S8. [25] Dowling PM. GI therapy: when what goes in won’t stay down. Proc WVC 2003. Accessed January2009atvin.com/Members/Proceedings/Proceedings.plx?CID=wvc2003&PID=pr03480&O=VIN. [26] Flake ZA, Scalley RD, Bailey AG. Practical selection of antiemetics. AmFam Phys 2004;69:1169-1174,1176. [27] King GL. Animal models in the study of vomiting. Can J Physiol Phar-macol 1990;68:260 [28] Martirosov KS, Grigor’ev IuG, Borovkov MV, Zorin VV. Experimental study of the role of blocking 5-HT3-receptors of serotonin and D2-recep-tors of dopamine in the mechanism of early radiation vomiting in dogs. Radiats Biol Radioecol 2002;42(1):75-79. [29] Martirosov KS, Grigor’ev IuG, Borovkov MV, Zorin VV. Comparative experimental study of antiemetic action of lantranum in radiation-induced vomiting and vomiting caused by apomorphine. Radiats Biol Radioecol 2003;43(1):60-64. [30] Product information: Zofran. Research Triangle Park, NC: GlaxoSmith- Kline; 2006. [31] Andrews PLR, Naylor RJ, Joss RA. Neuropharmacology of emesis and its relevance to anti-emetic therapy: consensus and controversies. Support Care Cancer 1998;6:197-203. [32] Takahashi T, Kurosawa S, Wiley JW, et al. Mechanism for the gastrokinetic actions of domperidone. Gastroenterology 1991;101:703-710. [33] Kolh RL, MacDonald S. New pharmacologic approaches to the preven-tion of space/motion sickness. J Clin Pharmacol 1991; 31(10):934-946.
Copyright
Copyright © 2024 Dr. Chilakalapudi Meher Babu. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET63791
Publish Date : 2024-07-28
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

