Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Navigating the Nexus: Examining Job satisfaction, Sleep quality, and Well-being among Mental Health Professionals
Authors: Aarti Kumari Jha , Dr. Vikas Sharma
DOI Link: https://doi.org/10.22214/ijraset.2024.58517
Certificate: View Certificate
Abstract
The research delves into the reciprocal dynamics between Job satisfaction, sleep quality, and Well-being within the realm of clinical psychologists. Examining a sample of professionals in the field, our study unveils a notable impact of job satisfaction on sleep quality, revealing that higher job satisfaction corresponds to decreased sleep quality. Concurrently, poor sleep quality exhibits a significant adverse effect on overall well-being among clinical psychologists. Further analysis exposes a nuanced relationship, as job satisfaction directly influences well-being and exerts a substantial indirect effect mediated by sleep quality. These findings underscore the intricate connections between occupational satisfaction, sleep quality, and mental well-being in the context of clinical psychologists, offering insights that can inform targeted interventions to enhance their overall mental health and work-life balance.
Introduction
I. INTRODUCTION
In the vibrant tapestry of India, where ancient traditions intertwine with contemporary challenges, clinical psychologists play a vital role. They are the empathetic navigators, guiding individuals through the monsoon storms of mental distress, their resilience a beacon amid emotional turbulence. Yet, beneath the stoic facade of their practice, a crucial question remains unanswered: who guides the compass of their well-being? Research indicates that mental health professionals experience higher levels of stress in challenging situations compared to their counterparts in other healthcare fields [Rabin S. et al, (1999); W. Stress Rossler (2012); U Volpe et al., (2014)). Clinical psychologists, particularly those with limited experience, were found to experience elevated levels of stress Rabin S. et al., (1999).
This research embarks on a journey into the uncharted territory of Indian clinical psychologists' inner landscapes, illuminating the intricate dance between job satisfaction, sleep quality, and holistic well-being. Across the nation's diverse tapestry, where an estimated 1 in 5 grapples with mental health burdens, these dedicated professionals stand as pillars of hope. They are the architects of healing, the sculptors of emotional resilience, and the unsung heroes of countless silent victories. However, their well-being, the very source of their strength, often remains veiled in whispers, a hidden melody amidst the orchestra of care they provide.
In the past, healthcare professionals, including nurses, received training and often stayed within a single institution for the duration of their careers. This continuity facilitated the development of enduring relationships with colleagues, patients, and families (Randall & Mckeown, 2013). However, present healthcare dynamics are characterized by fragmented roles, the routine and mechanized nature of practices, job instability, and frequent staff turnover, as healthcare professionals, including nurses, seek opportunities in the open job market. Consequently, this shift has resulted in a certain level of disengagement among healthcare workers from their roles, contributing to the depersonalization of healthcare (Randall & Mckeown, 2013).
The landscape of mental health care is evolving towards greater multidisciplinary collaboration, bringing together professionals with diverse beliefs, values, and practices (Baker & Baker, 1999). Engaging in such collaborations might pose a potential threat of generating or amplifying job dissatisfaction, particularly when collaborative efforts cast uncertainties on an individual's competence or capacity to deliver effective services (G M Acker, 2010). This research transcends the mere pursuit of job satisfaction. We delve deeper, into the multifaceted prism of well-being, encompassing the emotional, physical, and social dimensions that orchestrate a harmonious life for these dedicated professionals
Compose a vibrant score for interventions and support systems tailored to the specific needs of Indian clinical psychologists, acknowledging their cultural context and resource limitations.
Amplify the whispers of their experiences, advocating for systemic changes that prioritize their well-being and dismantle the stigma surrounding mental health professionals.
Contribute to a crescendo of positive change in the mental health landscape, ensuring that the wellspring of those who heal can itself be replenished and flourish.
This research is not merely an academic pursuit; it is a journey of empathy, a quest to understand the silent orchestra of well-being within Indian clinical psychologists. By listening to their melodies, we hope to not only craft a future where their well-being is nurtured but also amplify the impact of their care, ensuring that the helping hand they extend is sustained by a vibrant wellspring within.
A. Job Satisfaction
Job satisfaction is the overall assessment of pleasant emotions that an individual feels regarding their work. (Senter & Morgan, 2010). Indeed, job satisfaction can be viewed as a broad measure reflecting the overall quality of life in a work-related context (Verhaeghe & Bracke, 2012). This perspective underscores why job satisfaction holds significance as a important variable in psychological researches. The complex nature of their work, navigating emotional intricacies and addressing mental health challenges, necessitates a closer look at the factors influencing job satisfaction in clinical psychologists. In a comparative analysis involving 203 psychologists employed across diverse public institutions, it was discovered that psychologists working in correctional facilities and public mental health hospitals reported significantly higher levels of burnout and job dissatisfaction (Senter & Morgan, 2010). In a study in the New York metropolitan area, 57% of participants reported experiencing burnout (Martin & Schinke, 1998). Professionals experiencing dissatisfaction may exert a detrimental impact on their colleagues, thereby harming the overall work environment (M P Salyers et al., 2015). Moreover, they are least interested express empathy or participate in optimistic engagements with clients, which can adversely affect client satisfaction with mental health services (Verhaeghe & Bracke, 2012; M P Salyers et al., 2015; J A Nissly et al., 2001). The consequences of burnout and job dissatisfaction, including absenteeism and staff turnover, extend to the disruption of established therapeutic relationships between professionals and clients (M P Salyers et al., 2015; Webster & Hackett, 1999), ultimately compromising the quality and continuity of service delivery (M P Salyers et al., 2015; Blankertz & Robinson, 1997).
Exploring the nuances of job satisfaction in this profession is essential for designing interventions that address specific stressors, enhance organizational support, and foster professional growth. By investing in research on job satisfaction, we pave the way for a resilient and content clinical psychology workforce, better equipped to provide effective mental health services and navigate the evolving landscape of psychological well-being.
B. Sleep Quality
A cornerstone of overall health remains an underexplored aspect in the professional lives of clinical psychologists. The demanding nature of their work, coupled with exposure to emotionally charged situations, underscores the significance of understanding sleep patterns in this cohort. An analysis of the existing literature suggests that severe insomnia is connected to bodily discomfort, disability, and manifestations of psychological distress ((Leger et al., 2001; Philip et al., 2006; Zammit et al., 1999). Numerous studies have established a link between sleep and behavioral signs of reduced well-being, although fewer have delved into the connection between sleep quality and psychological well-being. Numerous definitions of well-being are succinctly expressed in a comprehensive model, which presents two latent constructs: psychological well-being and subjective well-being (Keyes et al., 2002) There are indications of a connection between sleep and psychological well-being (PWB). A study utilizing polysomnography revealed that certain subscales of PWB were associated with indices of sleep quality (Ryff, Singer, & Love, 2004).
Recent research findings indicate a correlation between sleep duration and different aspects of psychological well-being, based on data collected from a community sample of adult participants (Hamilton, Nelson, Stevens, & Kitzman, 2007).). Research in this area along with satisfaction in job and wellbeing can inform tailored interventions, promote sleep hygiene, and contribute to the development of supportive organizational practices, ultimately fostering a healthier and more resilient clinical psychology workforce ready to meet the challenges of mental health provision.
C. Well-being
Research on psychologists' well-being has predominantly focused on the adverse consequences of caregiving, neglecting the exploration of psychologists' personal growth and satisfaction as they engage in facilitating developmental experiences for their clients.
These unfavorable aspects of caregiving are commonly identified as burnout (Maslach & Jackson, 1982) and compassion fatigue (Figley, 1999) among psychologists in general. For those specifically working with traumatized individuals, terms such as vicarious derangement (McCann & Pearlman, 1990), contact victimization (Courtois, 1988), secondary posttraumatic stress reaction (Dutton & Rubenstein, 1995; Figley, 1995), and secondary traumatic stress (Stamm, 1999) have been used to describe these negative impacts. The nature of their work, dealing with profound human emotions and complex cases, underscores the need to scrutinize the well-being of clinical psychologists. Insights gleaned from such research can inform targeted support systems, mental health interventions, and organizational policies, fostering a work environment that prioritizes the well-being of those dedicated to preserving the mental health of others.
II. RESEARCH QUESTION
Is there any significant relationship between Job satisfaction, Sleep quality, and Well-being?
A. Hypotheses
The study posits a series of hypotheses to comprehensively explore the intricate relationships among job satisfaction, sleep quality, and well-being. Firstly, H1 anticipates a noteworthy impact of job satisfaction on sleep quality, emphasizing the potential for individuals’ content with their work to experience improved sleep patterns. Secondly, H2 posits a dual impact, asserting that both job satisfaction and sleep quality significantly influence overall well-being. This hypothesis underscores the interconnected nature of these factors, suggesting that contentment in one's job and quality of sleep collectively contribute to an individual's overall sense of well-being. Notably, Hypothesis 3 proposes the involvement of sleep quality as a mediator in the connection between job satisfaction and overall well-being. This hypothesis proposes that the influence of job satisfaction on well-being is partially explained by the mediating factor of sleep quality, implying that the impact of job satisfaction on well-being operates, at least in part, through its effects on sleep quality. These hypotheses collectively form a framework for understanding the complex dynamics between job satisfaction, sleep quality, and well-being, offering insights into potential intervention points for fostering holistic well-being among individuals in various professional contexts.
III. METHODOLOGY
A. Participants
The sample population included 60 adolescents (35 men and 25 Women) of age range 35.42 years with no history of mental or physical disability. The average age of the sample was 35.42 years (SD ±2.325). Almost half the sample has experience greater than 5 years (n = 34, 56.6%), 3 had an experience of around 12 months (5%) and 23 students had an experience between 1 to 4 years (38.4%). Only those professionals were included in the study who were RCI licensed and had working experience of at least 10 months.
B. Operational Definition
- Job Satisfaction: Job satisfaction is the emotional inclination a person holds toward their present job, influencing their workplace behavior and manifesting in expressions of either contentment or dissatisfaction at work. (Apridar & Adamy, 2018; Singh & Onahring, 2019)
- Sleep Quality: The personal evaluation of sleep, encompassing factors such as the time it takes to fall asleep, duration of sleep, effectiveness, disruptions, reliance on sleep medications, and daytime impairment. (Buysse et al., 1989).
- Well-Being: A state characterized by experiencing positive emotions and moods, the lack of negative emotions, contentment with one's life, a sense of fulfillment, and overall positive well-being. (M Chutiyami et al., 2022)
C. Measures
Initially, mental health professionals were requested to furnish their demographic details, including age, gender, and professional experience. Subsequently, they were tasked with completing the Job Satisfaction Index, Pittsburgh Sleep Quality Index, and Well-being Assessment Scale.
JSI (Job Satisfaction Index)- to assess job satisfaction in clinical psychologists- by Brayfield and Rothe, 1951- comprises 18 items in a 5-point Likert scale ranging from Strongly Agree to Strongly Disagree as options having a value of 1,2,3,4 and 5 respectively. Items 1, 2, 5, 7, 9, 12, 13, 15, and 17 follow a reversed scoring system. Score ranges from 7-35, higher score pointing to higher gaming addiction. The scoring scale spans from 18 to 90, with higher scores indicating a higher level of job satisfaction, while lower scores correspond to a lower level of job satisfaction.
PSQI (Pittsburgh Sleep Quality Index) - to assess the sleep quality in clinical psychologists- by Buysse et al. (1989)- comprises 19 self-rated questions and an additional 5 questions, if available, assessed by a bed partner or roommate. The scoring focuses solely on the self-rated questions. Seven "component" scores, each ranging from 0 to 3 points, categorize the 19 self-rated items. A score of "0" denotes no difficulty, while "3" signifies significant challenges across all components. The sum of these seven component scores produces a solitary "global" score, with a range of 0 to 21 points. A global score of "0" implies no difficulty, while a score of "21" indicates severe difficulties in all evaluated areas.
WBA (Well-Being Assessment (Adult – 24 items)) – to assess psychological well-being in clinical psychologists – by M. C. Stiefel (2020)- The Well-Being Assessment (WBA) for adults is a 24-item questionnaire crafted to gauge diverse aspects of well-being. This tool is organized to assess an individual's overall well-being across physical, emotional, social, and psychological realms. Participants self-report their ratings on various well-being facets, offering insights into their mental and emotional states. The WBA consists of items on a Likert scale ranging from "0" to "10" having a range of scores between 0 to 240.
D. Procedure and Consent
Clinical psychologists were initially identified based on their possession of an RCI license. Only those holding valid licenses were approached, and participation was voluntary. Selected participants were then briefed about the research objectives, and their informed consent was obtained before inclusion. Emphasis was placed on assuring participants of the confidentiality and anonymity of their responses.
A comprehensive questionnaire encompassing the Job Satisfaction Index, Well-being Assessment, and Pittsburgh Sleep Quality, along with demographic inquiries (such as age, gender, and years of experience), was presented to participants. All questions were in a self-report format, and participants were informed that completing the questionnaire would take approximately 30-40 minutes. Rigorous efforts were made to ensure that all items were appropriately marked during the data collection process.
Data collection commenced with an initial sample of 70 clinical psychologists. Subsequently, the participants underwent a shortlisting process based on their professional experience, with inclusion criteria requiring a minimum of 12 months of relevant work experience for participation in the study.
E. Ethics
The research adhered to stringent ethical guidelines to safeguard the well-being and rights of the participating clinical psychologists. Before their involvement, individuals were identified based on their possession of an RCI license, ensuring a professional and qualified pool.
Participation was entirely voluntary, with only licensed psychologists being approached, and explicit consent was obtained before their inclusion in the study. Throughout the process, participants were extensively briefed on the research objectives, and their informed consent was obtained, emphasizing the voluntary nature of their involvement. Ensuring the utmost confidentiality was a fundamental principle, and participants were guaranteed that their responses would be handled with the highest level of privacy and anonymity.
The comprehensive questionnaire, covering domains such as job satisfaction, well-being, and sleep quality, included demographic inquiries and was presented in a self-report format.
The research team took measures to ensure that the completion of the questionnaire, lasting approximately 30-40 minutes, did not compromise the well-being or comfort of the participants. Rigorous efforts were made during data collection to maintain confidentiality and the ethical integrity of the study.
The study protocol received ethical approval from the relevant institutional review board, underscoring the commitment to ethical standards throughout the research process.
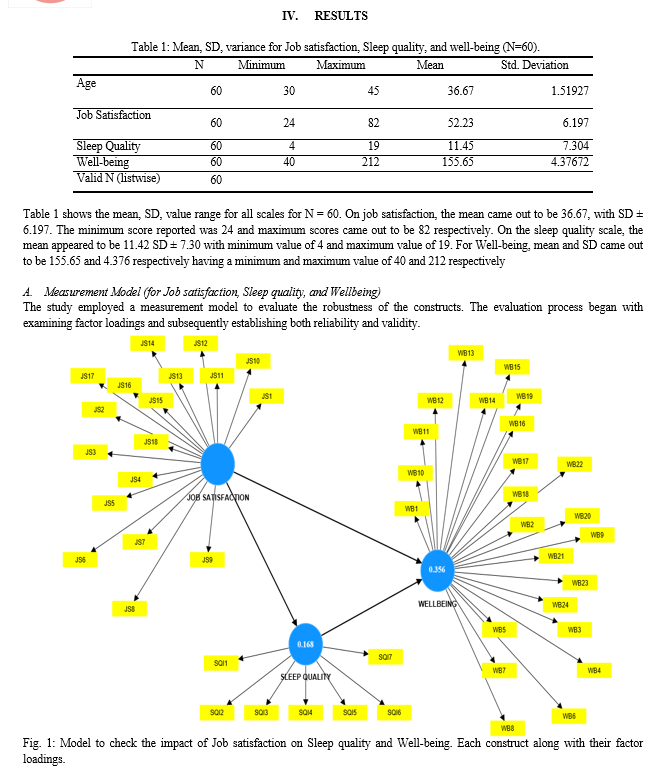
F. Analytical Plan
A partial least squares (PLS) SEM in SmartPLS 4 was employed to validate our model (https://www.smartpls.com/ [accessed 2024-01-01]). This analytical approach was chosen for its suitability, as PLS is not reliant on normal distributions or interval scales (W. W. Chin et al., 2003), aligning well with our research objective. To ensure robust predictions, we conducted 10,000 bootstrap procedures. In the model, we amalgamated Job Satisfaction, Sleep quality, and Well-being to assess the impact of Job satisfaction on Sleep quality and well-being and to assess the indirect effect of job satisfaction on well-being through sleep quality. The model was then checked for psychometric properties to establish reliability and validity. When established, the model was used for hypothesis testing.



Therefore, on the basis of Table 5, it can be inferred that the Q2 value for each endogenous construct exceeded 0, confirming the establishment of predictive relevance.
The SRMR value was computed to enhance prediction relevance. According to Hu and Bentler (1999), a good fit is indicated when the SRMR value is less than 0.10 or 0.08. In the present analysis, the SRMR value for each endogenous construct is 0.072 and 0.079, falling slightly outside the recommended range but still suggesting a reasonably close fit.
C. Structural Model
- Hypotheses Testing
a. H1: There shall be a significant impact of Job Satisfaction on Sleep Quality.
H1 estimates that there shall be a significant impact of Job Satisfaction on Sleep Quality. The findings revealed a significant impact on Sleep Quality by Job satisfaction (β = -.421, t = 4.278, p < .005). Hence, we failed to reject hypothesis H1. The negative correlation (r = -.421, p < .005), implies that with an increase in Job Satisfaction, there shall be a decrease in the Sleep quality index, thus leading to better quality of sleep.
b. H2: There shall be a significant impact of Job Satisfaction and Sleep quality on Well-being.
H2 estimates that there shall be a significant impact of Job Satisfaction and Sleep quality on Well-being. The finding revealed that there is a significant effect of Job Satisfaction (β = -.478, t = 4.278, p < .005) and Sleep quality (β = .404, t = 5.329, p < .005)., thus contributing a collective variance of 37.2% onto Well-being. Hence, we failed to reject H2.
c. H3: Sleep quality will mediate the relationship between Job Satisfaction and Well-being.
H3 estimates the presence of significant mediation through sleep quality. Upon analyzing indirect effects, a notable outcome emerged: significant indirect impact of job satisfaction on well-being mediated by sleep quality was establised. (Indirect effect = .07, SE = .02, CI = [-.14, -.02]). Hence, we fail to reject H3.
|
Hypotheses |
Impact |
Sig. |
Reject/ Failed to reject |
|
H1 |
Job Satisfaction à Sleep Quality |
0.045 |
Failed to reject |
|
H2 |
Job Satisfaction X Sleep Quality à Well-being |
0.034 |
Failed to reject |
|
H3 |
Job Satisfaction à Sleep quality à Well-being |
0.046 |
Failed to reject |
Table 6: Hypotheses table
V. DISCUSSION
The primary objective of this study was to assess the intricate relationship between job satisfaction, sleep quality, and overall well-being within the context of clinical psychologists. The hypotheses formulated were tested to ascertain the significant impact of job satisfaction on sleep quality (H1), the combined influence of job satisfaction and sleep quality on well-being (H2), and the role of sleep quality in mediating the connection between job satisfaction and well-being (Hypothesis 3).
H1: Job Satisfaction's Impact on Sleep Quality
The findings supported H1, revealing a significant impact of job satisfaction on sleep quality (β = -.421, t = 4.278, p < .005). The negative correlation (r = -.421, p < .005) indicated that higher job satisfaction was associated with lower sleep quality scores, suggesting an intriguing inverse relationship. This implies that as job satisfaction increased, there was a corresponding decrease in the sleep quality index, indicative of a potential trade-off between professional contentment and sleep patterns. The study conducted by B.A. Scott and T.A. Judge (2006) reinforced the findings, proposing a negative correlation between job satisfaction and insomnia. Similarly, S. Karagozoglu & N. Bingol (2008) observed comparable results in their research on nurses, revealing a weak negative correlation between sleep quality and job satisfaction.
H2: Combined Impact of Job Satisfaction and Sleep Quality on Well-being
Consistent with H2, the study demonstrated a significant impact of both job satisfaction (β = -.478, t = 4.278, p < .005) and sleep quality (β = .404, t = 5.329, p < .005) on well-being.
Together, job satisfaction and sleep quality accounted for a substantial collective variance of 37.2% in well-being. This suggests that the quality of one's job satisfaction and sleep patterns collectively contribute significantly to overall well-being among clinical psychologists. Supporting this, N.A. Hamilton et al. (2007) in their study on soldiers found that individuals who experienced optimal sleep reported lower levels of depression and anxiety symptoms. Additionally, Individuals who experience optimal sleep reported elevated levels of environmental mastery, personal growth, positive relationships with others, a strong sense of purpose in life, and self-acceptance. In the context of job satisfaction and well-being, Cary L. Cooper et al. (1999) corroborated these findings in their study on anesthetists. They revealed that the key factors influencing well-being were organizational issues, particularly communication within the hospital, and the perceived lack of control.
H3: Mediation of Sleep Quality in the Job Satisfaction-Well-being Relationship
The examination of indirect effects supported H3, indicating a significant indirect effect of job satisfaction on well-being through sleep quality (Indirect effect = .07, SE = .02, CI = [-.14, -.02]). Since job satisfaction and well-being have a significant direct relationship as well, this implies that sleep quality fully mediates the relationship between job satisfaction and well-being, highlighting the importance of considering sleep patterns as a contributing factor to the overall well-being of clinical psychologists.
Several potential reasons may explain the observed mediation of sleep quality in the relationship between job satisfaction and well-being:
Stress Reduction: Higher job satisfaction may lead to reduced workplace stress, contributing to improved sleep quality. A positive work environment and job satisfaction can alleviate stressors that might otherwise interfere with a person's ability to sleep well.
Work-Life Balance: Satisfied employees may find it easier to establish a healthy work-life balance, allowing for adequate time for rest. This balance can positively influence sleep patterns and overall well-being.
Psychological Well-being: Job satisfaction is often linked to positive psychological well-being. Employees who are content with their work may experience fewer negative thoughts and emotions, promoting better sleep quality and overall mental health.
VI. LIMITATIONS
- Sample Size and Generalizability: The sample size of 60 adolescents, though carefully selected, may limit the generalizability of the findings to a broader population. The age range and professional background of clinical psychologists may not represent the diversity within the entire field.
- Cross-Sectional Design: The study's cross-sectional design restricts the ability to establish causation. Longitudinal studies would be more appropriate for understanding the dynamic interplay between job satisfaction, sleep quality, and well-being over time.
- Self-Report Measures: The data heavily relies on self-report measures, including the Job Satisfaction Index, Well-being Assessment, and Pittsburgh Sleep Quality. Self-report measures are subject to biases, and participants may provide socially desirable responses, potentially impacting the accuracy of the results.
- Exclusion Criteria: The exclusion of participants with a history of mental or physical disability might limit the study's applicability to populations with such conditions. Future research should explore these relationships within diverse groups, including individuals with disabilities.
- Single Geographic Location: The study may lack external validity as it focuses on clinical psychologists from a specific geographic location. Cultural and regional variations could influence job satisfaction, sleep quality, and well-being differently in diverse settings.
- Analytical Approach: While the partial least squares (PLS) SEM is suitable for the study's objectives, alternative statistical methods were not explored. Different analytical approaches might yield varying results and interpretations.
- Limited Control Variables: The study primarily focuses on job satisfaction, sleep quality, and well-being, omitting potential confounding variables that could influence the observed relationships. Including additional factors in future studies could provide a more comprehensive understanding.
Conclusion
The study provides valuable insights into the intricate relationships among job satisfaction, sleep quality, and well-being in the context of clinical psychologists. The findings underscore the need for a holistic approach to well-being interventions, considering both job satisfaction and sleep quality as integral components. The identified associations contribute to a nuanced understanding of factors influencing the mental health and overall well-being of professionals in the field of clinical psychology. Furthermore, the study highlights the significance of recognizing the specific dynamics within the realm of clinical psychology when exploring the interplay of job satisfaction, sleep quality, and well-being. Clinical psychologists, who often navigate unique stressors and demands in their profession, may find the identified relationships particularly relevant. The insights gained from this research shed light on the importance of tailored interventions for professionals in clinical psychology. Addressing job satisfaction and sleep quality concurrently in well-being initiatives can potentially yield more effective outcomes, considering the specific challenges and nuances of this occupational group. The study advocates for the integration of workplace strategies that not only enhance job satisfaction but also prioritize sleep hygiene and overall sleep wellness. Moreover, the nuanced understanding provided by this research emphasizes the interconnectedness of mental health components for clinical psychologists. Recognizing the intricate web of factors influencing their well-being is essential for developing comprehensive support systems and fostering a healthier work environment within the field of clinical psychology. These findings contribute to the broader discourse on occupational well-being and provide a foundation for targeted interventions aimed at improving the mental health outcomes of clinical psychologists.
References
[1] Acker GM. The challenges in providing services to clients with mental illness: managed care, burnout and somatic symptoms among social workers. Community Ment Health J. 2010;46:591–600. https://doi.org/10.1007/s10597-009-9269-5 [2] Apridar, and Adamy, M. (2018). The Effect of Job Satisfaction and Work Motivation on Organizational Commitment and Organizational Citizenship Behavior in BNI in the Working Area of Bank Indonesia Lhokseumawe. In Proceedings of MICoMS 2017. Emerald Publishing Limited. https://doi.org/10.1108/978-1-78756-793-1-00063 [3] Bagozzi, R. P., Yi, Y., & Phillips, L. W. (1991). Assessing construct validity in organizational research. Administrative science quarterly, 421-458. https://doi.org/10.2307/2393203 [4] Baker JG, Baker DF. Perceived ideological differences, job satisfaction and organizational commitment among psychiatrists in a community mental health center. Community Ment Health J. 1999;35:85–95. https://doi.org/10.1023/A:1018704327272 [5] Blankertz LE, Robinson SE. Turnover intentions of community mental health workers in psychosocial rehabilitation services. Community Ment Health J. 1997;33:517–29. https://doi.org/10.1023/A:1025000703487 [6] Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989 May;28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4 [7] Chin, W. W., Marcolin, B. L., & Newsted, P. R. (2003). A partial least squares latent variable modeling approach for measuring interaction effects: Results from a Monte Carlo simulation study and an electronic-mail emotion/adoption study. Information systems research, 14(2), 189-217. https://doi.org/10.1287/isre.14.2.189.16018 [8] Chutiyami, M, Cheong, AM, Salihu, D, et al. COVID-19 pandemic and overall mental health of healthcare professionals globally: a meta-review of systematic reviews. Front Psychiatry. 2022;12:2600 https://doi.org/10.3389/fpsyt.2021.804525 [9] Cooper, C. L., Clarke, S., & Rowbottom, A. M. (1999). Occupational stress, job satisfaction and well?being in anaesthetists. Stress Medicine, 15(2), 115-126. https://doi.org/10.1002/(SICI)1099-1700(199904)15:2<115::AID-SMI797>3.0.CO;2-4 [10] Courtois, C. A. (1988). Healing the incest wound: Adult survivors in therapy. New York: Norton. [11] Dutton, M. A., & Rubenstein, F. L. (1995). Trauma workers. In C. R. Figley (Ed.),Trauma and its wake: Secondary traumatic stress disorder (Vol. 3). New York: Brunner/Mazel. https://psycnet.apa.org/record/1995-97891-004 [12] Falk, R. F., & Miller, N. B. (1992). A primer for soft modeling. University of Akron Press. https://psycnet.apa.org/record/1992-98610-000 [13] Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservablevariables and measurement error. Journal of marketing research, 18(1), 39-50. https://doi.org/10.1177/002224378101800104 [14] Figley, C. R. (1995). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner/Mazel. https://psycnet.apa.org/record/1995-97891-000 [15] Figley, C. R. (1999). Compassion fatigue: Toward a new understanding of the costs of caring. In B. H. Stamm (Ed.), Secondary traumatic stress: Self–care issues for clinicians, researchers, and educators (2nd ed., pp. 3–28). Lutherville, MD: Sidran Press. https://psycnet.apa.org/record/1996-97172-001 [16] Hair, Joseph F. and Ringle, Christian M. and Sarstedt, Marko, Editorial - Partial Least Squares Structural Equation Modeling: Rigorous Applications, Better Results and Higher Acceptance (March 14, 2013). Long Range Planning, Volume 46, Issues 1-2, pp. 1-12, https://ssrn.com/abstract=2233795 [17] Hamilton, N. A., Nelson, C. A., Stevens, N., & Kitzman, H. (2007). Sleep and psychological well-being. Social Indicators Research, 82, 147-163. https://www.jstor.org/stable/20734450 [18] Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling, 6(1), 1-55 https://doi.org/10.1080/10705519909540118 [19] Karagozoglu, S., & Bingöl, N. (2008). Sleep quality and job satisfaction of Turkish nurses. Nursing outlook, 56(6), 298-307. https://doi.org/10.1007/s11205-006-9030-1 [20] Keyes, C. L. M., Shmotkin, D., & Ryff, C. D. (2002). Optimizing wellbeing: The empirical encounter of two traditions. Journal of Personality & Social Psychology, 82, 1007–1022 https://doi.org/10.1037/0022-3514.82.6.1007 [21] Krystal, A. D., & Edinger, J. D. (2008). Measuring sleep quality. Sleep medicine, 9, S10-S17. https://doi.org/10.1016/S1389-9457(08)70011-X [22] Leger, D., Scheuermaier, K., Philip, P., Paillard, M., & Guilleminault, C. (2001). SF-36: Evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosomatic Medicine, 63, 49 – 55. https://doi.org/10.1097/00006842-200101000-00006 [23] Martin U, Schinke SP. Organizational and individual factors influencing job satisfaction and burnout of mental health workers. Soc Work Health Care. 1998;28:51–62. https://doi.org/10.1300/J010v28n02_04 [24] Maslach, C., & Jackson, S. E. (1982). Burnout in health professions: A social psychological analysis. In G. Sanders & J. Suls (Eds.), Social psychology of health and illness (pp. 227–251). Hillsdale, NJ: Erlbaum. https://www.researchgate.net/publication/322936969_Burnout_in_Health_Professions_1982 [25] McCann, I. L., & Pearlman, L. A. (1990). Vicarious traumatization: A framework for understanding the psychological effects of working with victims. Journal of Traumatic Stress, 3, 131–149. https://doi.org/10.1007/BF00975140 [26] Mor Barak ME, Nissly JA, Levin A. Antecedents to retention and turnover among child welfare, social work, and other human service employeees: what can we learn form past research? A review and metanalysis. Soc Serv Rev. 2001;75:625–61. https://www.journals.uchicago.edu/doi/abs/10.1086/323166 [27] Philip, P., Leger, D., Taillard, J., Quera-Salva, M. A., Niedhammer, I., Mosqueda, J. G., et al. (2006). Insomniac complaints interfere with quality of life but not with absenteeism: Respective role of depressive and organic comorbidity. Sleep Medicine, 7, 585–591. https://doi.org/10.1016/j.sleep.2006.04.006 [28] Rabin S, Feldman D, Kaplan Z. Stress and intervention strategies in mental health professionals. Br J Med Psychol. 1999;72(Pt 2):159–69. [29] Randall D, McKeown M. Editorial: failure to care: nursing in a state of liquid modernity. J Clin Nurs. 2013;23:766–7. https://doi.org/10.1111/jocn.12441 [30] Rössler W. Stress, burnout, and job dissatisfaction in mental health workers. Eur Arch Psychiatry Clin Neurosci. 2012;262:S65–9. https://doi.org/10.1007/s00406-012-0353-4 [31] Ryff, C. D., Singer, B. H., & Love, G. D. (2004). Positive health: Connecting well-being with biology. Philosophical Transactions of the Royal Society of London B, 359, 1383–1394. https://doi.org/10.1007/s00406-012-0353-4 [32] Salyers, M. P., Fukui, S., Rollins, A. L., Firmin, R., Gearhart, T., Noll, J. P., ... & Davis, C. J. (2015). Burnout and self-reported quality of care in community mental health. Administration and Policy in Mental Health and Mental Health Services Research, 42, 61-69. https://doi.org/10.1007/s10488-014-0544-6 [33] Scott, B. A., & Judge, T. A. (2006). Insomnia, emotions, and job satisfaction: A multilevel study. Journal of Management, 32(5), 622-645. https://doi.org/10.1177/0149206306289762 [34] Senter A, Morgan RD, Serna-McDonald C, Bewley M. correctional psychologist burnout, job satisfaction. Psychol Serv. 2010;7:190–201. https://doi.org/10.1037/a0020433 [35] Singh, K., & Onahring, B. D. (2019). Entrepreneurial intention, job satisfaction and organisation commitment-construct of a research model through literature review. https://doi.org/10.1186/s40497-018-0134-2 [36] Stamm, B. H. (Ed.). (1999). Secondary traumatic stress: Self–care issues for clinicians, researchers, and educators (2nd ed.). Lutherville, MD: Sidran Press https://psycnet.apa.org/record/1996-97172-000 [37] Stiefel, M. C., McNeely, E., Riley, C. L., Roy, B., Straszewski, T., & VanderWeele, T. J. (2020). Well-Being Assessment (Adult - 24 items). 100 Million Healthier Lives, convened by the Institute for Healthcare Improvement. http://www.ihi.org/100MLives [38] Verhaeghe M, Bracke P. Associative stigma among mental health professionals: implications for professional and service user well-being. J Health Soc Behav. 2012;53:17–32. https://doi.org/10.1177/0022146512439453 [39] Volpe U, Luciano M, Palumbo C, Sampogna G, Del Vecchio V, Fiorillo A. Risk of burnout among early career mental health professionals. J Psychiatr Ment Health Nurs. 2014;21:774–81. https://doi.org/10.1111/jpm.12137 [40] Webster L, Hackett RK. Burnout and leadership in community mental health systems. Admin Pol Ment Health. 1999;26:387–99. https://doi.org/10.1023/a:1021382806009 [41] Zammit, G. K., Weiner, J., Damato, N., Sillup, G. P., & McMillan, C. A. (1999). Quality of life in people with insomnia. Sleep, 22, 379 –385. https://psycnet.apa.org/record/1999-03090-005
Copyright
Copyright © 2024 Aarti Kumar Jha , Dr. Vikas Sharma. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET58517
Publish Date : 2024-02-20
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

