Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- References
- Copyright
Parkinson Disease
Authors: Mr. Rode Karan Ganesh, Miss. Vaishnavi Jadhav, Dr. Gajanan Sanap
DOI Link: https://doi.org/10.22214/ijraset.2024.57956
Certificate: View Certificate
Abstract
Parkinson\'s disease is a common neurodegenerative condition that affects millions of people globally. Considerable advancements have been made in our knowledge of Parkinson\'s disease\'s pathophysiology, etiology and treatment over the last fifty years. This article reviews our current understanding of Parkinson disease, including its phenomenology, epidemiology, and treatments that are available.
Introduction
I. NEW FOUNDATIONS
Parkinson's disease is now recognized to be a diverse illness with both motor and nonmotor symptoms. Its composition consists of prodromal, preclinical, and clinical phases. New, more easily administered drugs have been approved for its treatment.
Novel surgical therapies may be used to treat Parkinson disease when the best medical care is insufficient to relieve motor symptoms.
II. PATHOPHYSIOLOGY OF PARKINSON DISEASE(PD)
The main pathological features of PD are the loss of dopaminergic neurons with subsequent depigmentation of the SNpc and the presence of LBs.
LBs are intraneuronal, round, eosinophilic inclusions with a hyaline core and a pale peripheral halo that are composed of more than 90 proteins [1]; their main components are α -synuclein and ubiquitin[2].
α-synuclein has the propensity to misfold, become insoluble and form b-sheet-rich amyloid aggregates that accumulate and form intracellular inclusions. The intermediates in this aggregation process are the toxic oligomeric and proto-fibrillar forms that impair mitochondrial [3], lysosomal and proteasomal [4] function, damage biological membranes [5] and the cytoskeleton [6], alter synaptic function [7] and cause neuronal degeneration. It has been estimated that at the time of the diagnosis up to 60% of dopaminergic neurons have already been lost [8].
III. EPIDEMIOLOGY
Parkinson's disease is an aging-related condition, with a steady rise in incidence and prevalence as people age.in [9]But it's important to dispel the myth that Parkinson's disease only strikes the elderly. About 25% of those affected had their onset before the age of 65, and 5–10% had their onset before the age of 50.
When referring to affected individuals whose age of onset is younger than 40 years old (or possibly even younger than 50 years old), the term "young-onset Parkinson's disease" has been introduced. The disease is present throughout the world, with the exception of two notable epidemiological differences: a disproportionately rapid rise in new cases in China [10] and a rapid increase in high-income European countries.11]
In the last two decades, the number of deaths and disabilities from Parkinson's disease worldwide has more than doubled. Although Parkinson’s disease affects both sexes, women might have several advantages over men: their incidence of the disease is lower, particularly for individuals aged 50-59 years.[12] Mortality does not decrease over the first ten years of the illness; rather, it increases and eventually doubles when compared to the overall population. Improved health care leads to longer survival, and a 20-year study revealed an increase in the prevalence of Parkinson disease over time. The number of individuals with Parkinson's disease will double between 2005 and 2030.
From 1990 to 2010, Parkinson disease increased years lived with disability and disability adjusted life years; the personal, societal, and financial costs associated with the condition are expected to continue rising as the world's population ages.[26] In most populations, men are twice as likely to get Parkinson's disease as women are yet in a few, like the Japanese study, there was no difference or even an excess of women. A safeguarding impact of female sex hormones, a genetic marker linked to sex process or variations in exposure to the This male preponderance could be explained by environmental risk factors, but health care inequities could also play a part.[27]

IV. INTRODUCTION
(PD) is a common neurodegenerative disease that affects synucleins; in Western Europe, its prevalence is 160/100,000. increasing to 4% of people over the age of 80.13] The management of Parkinson's disease (PD) is expected to become a more significant and difficult component of neurology and general practice for physicians as the population ages. Over the past ten years, a number of gene mutations have been identified that may provide insight into the pathogenesis of sporadic cases of Parkinson's disease (PD). These mutations have advanced our understanding of the disease's pathogenesis. Parkinson's disease (PD) is still primarily diagnosed clinically, so it's critical to identify early symptoms as well as signs that point to alternative causes of parkinsonism. Additionally, the range of available treatments has rapidly expanded, with both In. Guidelines for the diagnosis And management of patients with PD have been published from the National Institute for Health and Clinical Excellence (NICE) in the UK.[14]
The impact of Parkinson's disease on society is significant. Regarding the quantity of individuals afflicted, this illness is widespread, with roughly 61 million cases reported globally in 2016.In [15] The effects of Parkinson's disease on an individual are profound. A degenerative disease's unique feature is that it can last for decades. For those who are affected, the usual pre sentence entails a gradual progression with increasing disability. Parkinson's disease has serious effects on caregivers as well; the majority experience extreme stress. In [16] Parkinson's disease represents an increasing socioeconomic burden on society.(17)
V. BRIEF HISTORY OF PARKINSON DISEASE
The English physician, James Parkinson, first characterized Parkinson disease in his 1817 monograph “An Essay on the Shaking Palsy.”[19] Parkinson reported a number of patients who had constipation, sleep issues, stooped posture, shuffling gait, and resting tremor. He dubbed the condition paralysis agitans after observing how the illness progressed and the severe impairment it caused. Later, Charcot[20] elaborated on the illness, renaming it Parkinson disease and adding bradykinesia and rigidity to the list of symptoms. Carlsson [21] discovered in the 1950s that levodopa could reverse the akinesia caused by reserpine, which opened the door for its use in treating Parkinson's disease. When Cotzias and colleagues[22] gave DLdihydroxyphenylalanine (DOPA) to patients with parkinsonism and saw positive outcomes, they found that levodopa alleviated Parkinson disease symptoms Levodopa, when paired with carbidopa, became the mainstay of medical therapy and remains so to this day.
VI. SYMPTOMS
Although the pathogenesis of Parkinson's disease (PD) is still not well understood, the disease's symptoms were first documented almost two centuries ago, and the disease's distinctive pathology was discovered almost a century ago. One of the most common neurodegenerative movements is Parkinson's disease. The discovery of several causative genetic mutations has recently led to an acceleration of research into the pathogenesis of the disorder. The ubiquitin-proteosome system is disrupted by the mutant gene products, indicating that protein modification and degradation are essential for pathogenesis. In all forms of the disease, modified non-degraded intracellular proteins accumulate in specific neuronal populations.
disease, we highlight the cell to Cell interactions and immune regulation critical for neuronal homeostasis and survival in Parkinson’s disease.[18]
On the other hand, neuronal degeneration is more specifically focused and is linked to a significant activation of the brain's inflammatory cells called microglia. We examine the recent shift in understanding of the function of microglia in the brain in relation to Parkinson's disease. and disease models based on animals. A consistent pattern is found when comparing the cellular tissue changes in several animal models of Parkinson's disease using different stimuli. These models implicate microglia as the effector for the selective degeneration of dopaminergic neurons. While earlier reviews have focused on the alterations in intracellular neurons in Parkinson's

VII. TREATMENT OF PD
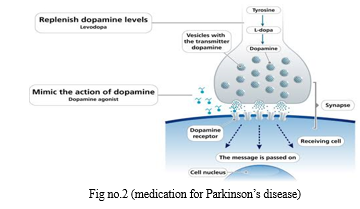
Dopamine-based pharmaceuticals are the mainstay of treatment for Parkinson disease's motor symptoms Initial therapy such as dopamine agonists, monoamine oxidase-B (MAO-B) inhibitors, and levodopa preparations are helpful For young people who exhibit a noticeable tremor, anticholinergic substances (such as trihexyphenidyl) are helpful, but use cautious due to the possibility of unfavourable outcomes, especially those connected to the mind.[23]
While levodopa was once avoided by many doctors while treating Parkinson's disease in its early stages, new data contradicts this recommendation. In one study (PD MED), participants who were randomized to start levodopa medication had minor but enduring advantages for mobility After seven years (1.8-point improvement in the average score .on the movement subscale of the Parkinson Disease Questionnaire-39 in contrast to people first given either MAO-B inhibitors or dopamine agonists.in Additionally, ADL performance improved in the 1.9-point improvement in the levodopa starting group over a 7-year period in the mean score on the 6-item, 0-to 24-point Parkinson Disease Questionnaire-39 ADL subscale [24]
A. Pharmacologic Treatment
When symptoms result in disability, pharmacotherapy is started. The age of the patient and the symptoms they are trying to manage determine the medication treatment plan . Some PD patients seek treatment for tremor early on, which can be alleviated by betablockers, primarily propranolol. As an alternative, benztropine or trihexyphenidyl, which are anticholinergics, or clozapine, an antipsychotic drug, have been shown to effectively reduce tremor. Since a dopamine deficit causes major motor symptoms, pharmacologic treatments for Parkinson's disease (PD) involve either blocking dopamine breakdown or substituting dopamine by stimulating the brain to release dopamine via an agonist .
VIII. MANAGEMENT OF OTHER MEDICINE
Adverse effect
Nausea
One common, usually brief side effect of dopaminergic treatment is nausea. Medication administration with food and a slow titration of dopaminergic therapy can both help to minimize nausea. Over time, however, meals may postpone stomach emptying and dietary protein may obstruct the absorption of levodopa.Benserazide and carbidopa, which are dopa decarboxylase inhibitors, stop peripheral conversion of dopamine to levodopa. Levodopa-induced nausea may be eliminated by an extra dose of carbidopa taken half an hour before the usual levodopa preparation, but not dopamine agonist-induced nausea.Peripheral dopamine D2-receptor antagonist Domperidone (not available in the United States), numerous modest CIII and CIV studies found that dopaminergic medicines decreased nausea. tetrahexanamide has also served the same function.Phenolodipine,Promethazine and prochlorperazine should be avoided since they can exacerbate symptoms of parkinsonian disease[25].
Prevention
- Regular physical checkup by physicians.
- Performing simple mental and aerobic exercises
- High fibre nutrition diet
- Use caffeine and Tea in diet
- Antioxidant such as Vitamin .C, Vitamin.D
- Non steroid anti inflammatory drugs (NSAID’S)
References
[1] Wakabayashi K, Tanji K, Odagiri S, et al. The Lewy body in Parkinson’s disease and related neurodegenerative disorders. Mol Neurobiol 2013; 47: 495–508. [2] Spillantini MG, Schmidt ML, Lee VM, et al. Alphasynuclein in Lewy bodies. Nature 1997; 388: 839– 40. [3] Hsu LJ, Sagara Y, Arroyo A, et al. Alpha-synuclein promotes mitochondrial deficit and oxidative stress. Am J Pathol 2000; 157: 401–10. [4] Snyder H, Mensah K, Theisler C, et al. Aggregated and monomeric a-synuclein bind to the S60 proteasomal protein and inhibit proteasomal function. J Biol Chem 2003; 278: 11753–9. [5] Danzer KM, Haasen D, Karow AR, et al. Different species of alpha-synuclein oligomers induce calcium influx and seeding. J Neurosci 2007; 27: 9220–32. [6] Alim MA, Ma Q-L, Takeda K, et al. Demonstration of a role for alpha-synuclein as a functional microtubuleassociated protein. J Alzheimers Dis 2004; 6: 435–42; discussion 443–449 [7] Scott DA, Tabarean I, Tang Y, et al. A pathologic cascade leading to synaptic dysfunction in alphasynuclein-induced neurodegeneration. J Neurosci 2010; 30: 8083–95. [8] Marsden CD. Parkinson’s disease. Lancet 1990; 335: 948–9. [9] Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 2014; 29: 1583–90. [10] Dorsey ER, Sherer T, Okun MS, Bloem BR. The emerging evidence of the Parkinson pandemic. J Parkinsons Dis 2018; 8: S3–8. [11] Deuschl G, Beghi E, Fazekas F, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020; 5: e551–67. [12] Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 2014; 29: 1583–90. [13] Mutch WJ, Dingwall-Fordyce I, Downie AW et al. (1986) Parkinson’s disease in a Scottish City. BMJ, 292, 534–536. [14] National Institute for Health and Clinical Excellence (2006) Parkinson’s Disease: Diagnosis And Management in Primary and Secondary Care. London: NICE (http://guidance.nice.org. Uk/CG35 [15] GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990– 2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 459–80. [16] Macchi ZA, Koljack CE, Miyasaki JM, et al. Patient and caregiver characteristics associated with caregiver burden in Parkinson’s disease: a palliative care approach. Ann Palliat Med 2020; 9 (suppl 1): S24–33. [17] GBD 2016 Parkinson‘s Disease Collaborators. Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2018; 17: 939– 53. [18] Bas, . J., Calopa, M., Mestre, M., Mollevi, D.G., Cutillas, B., Ambrosio,S., Buendia, E., 2001. Lymphocyte populations in Parkinson’s disease and in rat models of Parkinsonism. J. Neuroimmunol. 113, 146– 152.Parkinson disease [19] Parkinson J. An essay on the shaking palsy. London: Whittingham and Rowland Sherwood, Neely and Jones, 1817 [20] Charcot JM. Lectures on the diseases of the nervous system, delivered at La Salpetriere. London:The New Sydenham Society, 1877. [21] Carlsson A, Lindqvist M, Magnusson T. 3,4Dihydroxyphenylalanine and 5-hydroxytryptophan as reserpine antagonists. Nature 1957;180(4596):1200. Doi:10.1038/1801200a0. [22] Cotzias GC, Van Woert MH,Schiffer LM. Aromatic amino acids and modification of Parkinsonism. N Engl J Med 1967;282(7):31–33. Doi:10.1056/NEJM196702162760703. Doi:10.1056/ NEJM196702162760703. [23] Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord.2015;30(12):1591-1601. doi:10.1002/mds.2642 [24] Burciu RG, Ofori E, Archer DB, et al.Progression marker of Parkinson’s disease: a 4-year multi-site imaging study. Brain. 2017;140(8):2183-2192. doi:10.1093/brain/awx146 [25] Evans AH, Katzenschlager R, Paviour D, et al.Punding in Parkinson’s disease: its relation to the dopamine dysregulation syndrome. Mov Disord.2004;19(4):397-405 [26] Halliday, G. M., Holton, J. L., Revesz, T. & Dickson, D. W. Neuropathology underlying clinical variability in patients with synucleinopathies. Acta Neuropathol. 122, 187–204 (2011) [27] Iacono, D. et al. Parkinson disease and incidental Lewy body disease: just a question of time? Neurology 85,1670–1679 (2015).
Copyright
Copyright © 2024 Mr. Rode Karan Ganesh, Miss. Vaishnavi Jadhav, Dr. Gajanan Sanap. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET57956
Publish Date : 2024-01-09
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

