Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Review on Study of Pharmacovigilance in Diabetes Mellitus
Authors: Arati Kishanrao Landge, Maknikar Sakshi Namdevrao, Kshirsagar Varsha Rudrappa, Prajyot Dipak Manjramkar, Mande Sandip Padmakar, Girishankar Haridas Bhavale
DOI Link: https://doi.org/10.22214/ijraset.2025.66934
Certificate: View Certificate
Abstract
Diabetes mellitus (DM) represents a growing global epidemic, imposing significant socio-economic burdens on countries worldwide. Although treatment options for managing DM are evolving rapidly, conventional therapies have not fully addressed the root causes of the disease and are often associated with serious adverse effects. This narrative review examines various therapeutic strategies for DM management and their associated challenges. A comprehensive literature search was conducted using databases such as Web of Science, PubMed/Medline, and Scopus, employing keywords including \"diabetes mellitus,\" \"DM management,\" and \"gene therapy.\" Our findings reveal significant advancements in DM treatment with encouraging outcomes through diverse approaches, including nanotechnology, gene therapy, stem cell therapy, medical nutrition therapy, and lifestyle modifications. However, these strategies face considerable challenges, such as optimizing glycemic, lipid, and blood pressure control to reduce complications, enhancing patient adherence to lifestyle and pharmacological interventions, addressing safety and ethical concerns, and improving delivery systems. In conclusion, integrating lifestyle modifications with pharmacological therapies and refining these emerging techniques are essential for devising effective and safe clinical treatment plans.
Introduction
I. INTRODUCTION
When you consume food, your body breaks most of it down into sugar (glucose) and releases it into your bloodstream. An increase in blood sugar levels signals the pancreas to release insulin. Insulin acts as a key, enabling blood sugar to enter cells to be used as energy.
In diabetes, the body either does not produce enough insulin or cannot use it effectively. Without sufficient insulin or when cells become resistant to it, excess sugar remains in the bloodstream. Over time, this can lead to severe health complications, such as heart disease, vision loss, and kidney damage[1].
A. There is Currently no Cure for Diabetes
However, managing the condition through lifestyle changes can make a significant difference. Key steps include losing weight, eating a healthy diet, and staying physically active. Additional measures that can help manage diabetes effectively include:
- Taking medications as prescribed by your healthcare provider.
- Participating in diabetes self-management education and support programs.
- Scheduling and keeping regular healthcare appointments.
B. Etiology
The pancreas contains the islets of Langerhans, which house two primary types of endocrine cells: insulin-producing beta cells and glucagon-secreting alpha cells. These cells continuously adjust their hormone secretion in response to glucose levels to maintain balance. When this balance is disrupted, glucose levels become abnormally skewed. In diabetes mellitus (DM), the absence or impaired action of insulin (insulin resistance) leads to hyperglycemia.[2]
Type 1 Diabetes Mellitus (T1DM)
T1DM is characterized by the autoimmune destruction of pancreatic beta cells. This process results in an almost complete loss of beta cells, leading to an absence or extremely low levels of insulin.
Type 2 Diabetes Mellitus (T2DM)
T2DM develops more gradually due to an imbalance between insulin production and insulin sensitivity, resulting in a functional insulin deficiency. Insulin resistance in T2DM often arises from multifactorial causes, such as obesity and aging. Unlike T1DM, T2DM involves a complex interplay of genetic and lifestyle factors, with strong evidence suggesting a higher hereditary component. Most individuals with T2DM have at least one parent with the condition.[3]
C. Gestational Diabetes
Gestational diabetes refers to diabetes that develops during pregnancy. Although the exact cause remains unclear, several hypotheses suggest potential contributors:
- HLA antigens, specifically HLA-DR2, DR3, and DR4, may play a role.
- Excessive proinsulin could lead to beta-cell stress.
- High levels of pregnancy-associated hormones, such as progesterone, cortisol, prolactin, human placental lactogen, and estrogen, may impair beta-cell function and reduce insulin sensitivity.
D. Endocrinopathies and Other Conditions
Various endocrinopathies, such as acromegaly, Cushing syndrome, glucagonoma, hyperthyroidism, hyperaldosteronism, and somatostatinomas, are associated with glucose intolerance and DM due to the glucogenic effects of excessive hormone secretion. Additionally, conditions like idiopathic hemochromatosis can cause DM through excessive iron deposition in the pancreas, leading to beta-cell destruction[4].
E. Epidemiology
Globally, 1 in 11 adults is affected by diabetes, with 90% of cases attributed to T2DM.
- T1DM: The onset of T1DM typically occurs in childhood, with peaks between ages 4–6 and 10–14 years. Around 45% of cases present before the age of 10. The prevalence of T1DM in individuals under 20 is approximately 2.3 per 1000. Although most autoimmune diseases are more common in females, T1DM does not exhibit significant gender differences in childhood. However, in some populations, such as older males of European descent (over 13 years), males are more likely to develop T1DM than females (3:2 male-to-female ratio).
- The global incidence of T1DM is increasing. In Europe, Australia, and the Middle East, rates are rising by 2%–5% annually. In the United States, rates have been increasing by about 2% annually across most age and ethnic groups, with higher rates observed in Hispanic youth.
- T2DM: Data from the U.S. Military Health System suggests that T1DM rates plateaued from 2007 to 2012, with a prevalence of 1.5 per 1000 and an annual incidence of 20.7–21.3 per 1000.
Although the reasons for these trends are not fully understood, the observed patterns highlight the growing public health challenge posed by diabetes.
The onset of T2DM is typically later in life. However, increasing rates of obesity among adolescents have led to a growing prevalence of T2DM in younger populations. In the United States, T2DM affects approximately 9% of the general population, with a prevalence of about 25% among individuals over 65 years of age.
Globally, the International Diabetes Federation (IDF) estimated that in 2015, 1 in 11 adults aged 20–79 years had diabetes mellitus (DM). By 2040, this number is projected to rise from 415 million to 642 million, with the most significant increases occurring in populations transitioning from low- to middle-income countries.
The prevalence of T2DM varies significantly among ethnic groups, being 2–6 times more common in Black, Native American, Pima Indian, and Hispanic populations compared to Whites in the United States[5]. Environmental factors also contribute to this disparity. For example, Pima Indians in Mexico have a lower prevalence of T2DM (6.9%) compared to Pima Indians in the United States (38%).
II. CLINICAL PRESENTATION AND HISTORY
A thorough patient history is essential for diagnosing DM, focusing on family history, autoimmune diseases, and insulin resistance. T2DM often presents asymptomatically but may manifest with the following:
- Classic symptoms: Polyuria, polydipsia, and weight loss.
- Physical signs:
- Poor skin turgor (from dehydration).
- Fruity breath odor in cases of ketosis.
- Kussmaul respirations, fatigue, nausea, and vomiting in diabetic ketoacidosis (DKA).
- Blurry vision, frequent yeast infections, and neuropathic symptoms in long-standing hyperglycemia.
Patients with T2DM are often overweight or obese and may exhibit acanthosis nigricans, characterized by hyperpigmented, velvety skin patches on the neck, axillae, or inguinal folds. Routine diabetic foot exams, including monofilament testing, are critical to assess for neuropathy and skin changes[6].
III. EVALUATION AND DIAGNOSIS
A. Diagnostic Criteria
- T1DM: Diagnosis is based on clinical history and confirmed with elevated glucose levels:
- Fasting glucose ≥ 126 mg/dL
- Random glucose ≥ 200 mg/dL
- HbA1c ≥ 6.5%
- Detection of autoimmune markers, such as antibodies to glutamic acid decarboxylase (GAD).
- T2DM: Fasting glucose and HbA1c are first-line tests. Borderline cases can be further evaluated with an oral glucose tolerance test (OGTT). Prediabetes is diagnosed with:
- Fasting glucose: 100–125 mg/dL
- 2-hour post-OGTT glucose: 140–199 mg/dL
- Gestational Diabetes:
- Screening occurs at 24–28 weeks of gestation with a 1-hour fasting glucose challenge test.
- Glucose ≥ 140 mg/dL warrants a 3-hour fasting OGTT.
- Diagnostic values: Fasting ≥ 95 mg/dL, 1-hour ≥ 180 mg/dL, 2-hour ≥ 155 mg/dL, and 3-hour ≥ 140 mg/dL.
B. Pathophysiology of T2DM
T2DM results from a combination of impaired insulin secretion and insulin resistance. Key mechanisms include:
- Beta-cell dysfunction: Reduced insulin production in response to hyperglycemia.
- Insulin resistance: Caused by elevated free fatty acids and proinflammatory cytokines, leading to impaired glucose transport and increased lipolysis.
- Dysregulated glucagon secretion: Loss of the reciprocal relationship between alpha and beta cells, resulting in hyperglucagonemia and hyperglycemia.
- Metabolic dysregulation: Altered glucose and lipid metabolism contribute to hyperglycemia and dyslipidemia.
The “ominous octet” explains the multifactorial nature of T2DM:
- Reduced insulin secretion by beta cells.
- Increased glucagon secretion by alpha cells.
- Hepatic glucose overproduction.
- Brain insulin resistance.
- Increased lipolysis.
- Reduced incretin effect.
- Increased renal glucose reabsorption.
- Decreased peripheral glucose uptake in muscle, liver, and fat tissues.
IV. THERAPEUTIC APPROACHES FOR T2DM
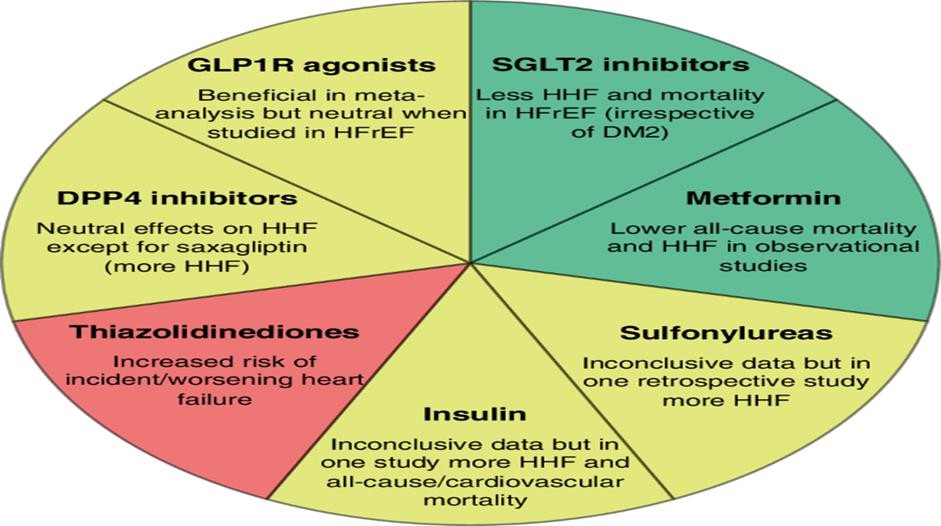
Non-insulin-based treatments focus on addressing the underlying pathophysiology and include:
- Insulin Secretagogues: Stimulate pancreatic beta cells to produce insulin.
- Biguanides (e.g., Metformin): Reduce hepatic glucose production and improve insulin sensitivity.
- Insulin Sensitizers (e.g., Thiazolidinediones): Improve peripheral tissue response to insulin.
- Alpha-glucosidase Inhibitors: Delay carbohydrate absorption in the gut.
- Incretin Mimetics: Enhance insulin secretion and inhibit glucagon.
- Amylin Analogues: Slow gastric emptying and promote satiety.
- SGLT2 Inhibitors: Reduce renal glucose reabsorption, promoting urinary glucose excretion.
A. Global Prevalence Trends
According to the 10th edition of the IDF Diabetes Atlas, diabetes prevalence in 2021 was estimated across 215 countries, covering 7 regions:
- Africa (AFR), Europe (EUR), Middle East and North Africa (MENA), North America and Caribbean (NAC), South and Central America (SACA), South-East Asia (SEA), and the Western Pacific (WP).
- By 2045, the global prevalence of diabetes is projected to rise substantially, highlighting the urgent need for prevention and management strategies.
1) Prevalence Growth
- Ageing and Population Growth: A 16% increase in diabetes prevalence is expected globally by 2045 due to population ageing.
- Income-Based Disparities:
- Middle-Income Countries: These regions are expected to experience the greatest percentage increase in comparative diabetes prevalence, driven primarily by ageing populations.
- Low- and Middle-Income Countries (LMICs): Approximately 94% of the total increase in people living with diabetes by 2045 will occur in LMICs, where population growth is projected to be highest.
2) Age Distribution
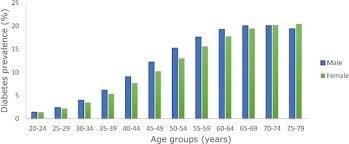
- Diabetes prevalence increases with age, with notable trends:
- Young Adults (20–24 years): The lowest prevalence of 2.2% in 2021.
- Older Adults (75–79 years): The highest prevalence, estimated at 24.0% in 2021, increasing slightly to 24.7% by 2045.
- Ageing Populations: A growing proportion of people with diabetes will be aged 60 years or older, reflecting global demographic shifts.
B. Demographic Insights
Gender Distribution
- In 2021, diabetes prevalence was slightly higher in men (10.8%) than in women (10.2%).
- There were 17.7 million more men living with diabetes compared to women globally.
Urban vs. Rural Distribution
- Urban Areas:
- In 2021, 360 million people with diabetes resided in urban areas, with a prevalence of 12.1%.
- By 2045, this is expected to rise to 596.5 million people and a prevalence of 13.9%, driven by urbanisation and population ageing.
- Rural Areas:
- In 2021, 176.6 million people with diabetes lived in rural areas, with a prevalence of 8.3%.
- Urbanisation trends suggest rural diabetes prevalence will grow more slowly compared to urban areas.
C. Regional and Country-Specific Trends
Regional Distribution
- Middle East and North Africa (MENA):
- Highest comparative prevalence in 2021 (18.1%) and projected to remain highest by 2045 (20.4%).
- Africa (AFR):
- Lowest prevalence in 2021 (5.3%), projected to increase to 5.2% by 2045, though likely an underestimate due to rapid urbanisation and lifestyle changes.
Country Distribution
- Countries with the Largest Number of People with Diabetes:
- 2021 and 2045: China, India, and Pakistan lead in the number of adults (20–79 years) with diabetes.
- However, these countries do not necessarily have the highest prevalence rates.
- Healthcare Expenditure:
- Countries with the lowest diabetes-related health expenditure in 2021:
- Gambia: USD 2.4 million.
- Nauru: USD 1.6 million.
- Countries with the lowest diabetes-related health expenditure in 2021:
V. CAUSES OF DIABETES
Understanding the causes of diabetes requires comprehension of the normal glucose metabolism process:
A. How Insulin Works
- Pancreatic Secretion: Insulin is a hormone produced by the pancreas, located behind and below the stomach.
- Glucose Regulation:
- Insulin allows sugar to enter the body’s cells for energy.
- It lowers blood sugar levels by moving glucose out of the bloodstream.
- Feedback Mechanism:
- As blood sugar levels decrease, insulin secretion slows down.
VI. RISK FACTORS
Type 1 Diabetes
- Family History: Increased risk if a parent, brother, or sister has type 1 diabetes.
- Age: Commonly develops in children, teens, or young adults, but can occur at any age.
Type 2 Diabetes
- Overweight or obesity.
- Age 45 years or older.
- Family history (parent or sibling with type 2 diabetes).
- Physical inactivity (less than three times per week).
- Presence of non-alcoholic fatty liver disease (NAFLD).
- History of gestational diabetes or giving birth to a baby weighing over 9 pounds.
Gestational Diabetes
- History of gestational diabetes in a previous pregnancy.
- Giving birth to a baby over 9 pounds.
- Overweight or obesity.
- Age over 25 years.
- Family history of type 2 diabetes.
Diagnosis of Diabetes
- Hemoglobin A1C (HbA1c) Test:
- Measures average blood sugar levels over the last 2–3 months.
- Diabetes: ≥6.5%.
- Fasting Blood Sugar Test:
- Fasting plasma glucose level of ≥126 mg/dL indicates diabetes.
- Oral Glucose Tolerance Test (OGTT):
- ≥200 mg/dL after a 2-hour plasma glucose test confirms diabetes.
- 140–199 mg/dL indicates impaired glucose tolerance.
- Random Blood Sugar Test:
- A random glucose level of ≥200 mg/dL, along with symptoms of hyperglycemia, confirms diabetes.
VII. TREATMENT APPROACHES
1) Type 1 Diabetes
- Self-care:
- Diabetic diet.
- Nutrition counseling.
- Carbohydrate counting.
- Regular physical exercise.
- Medications:
- Insulin.
- Dietary supplements.
- Hormonal therapies.
2) Type 2 Diabetes
- Self-care:
- Physical exercise.
- Smoking cessation.
- Weight loss.
- High dietary fiber intake.
- Nutrition counseling.
- Diabetic diet.
- Medications:
- Anti-diabetic agents.
- Statins (for cholesterol management).
- Insulin therapy (if needed).
3) Prediabetes
- Self-care:
- Physical activity.
- Weight loss.
- Diet modifications (low-carb, Mediterranean, or low-fat diet).
- Diabetic diet.
- Medications:
- Anti-diabetic drugs for high-risk individuals.
VIII. MECHANISM OF ACTION OF ANTIDIABETIC DRUGS
|
SR .NO |
CLASS |
BRANDS |
DOSAGE FORMS |
MECHANISM OF ACTION |
|
1. |
Sulfonylurea |
Glyburide, Glimepiride Glipizide |
Oral tablets |
Stimulating insulin release by pancreatic beta cells by inhibiting the KATP channel |
|
2. |
Biguanides |
Metformin |
Oral tablets |
Acts on the liver to reduce gluconeogenesis and decrease in insulin resistance via increasing AMPK signaling |
|
3. |
.Alpha- glucosidase inhibitor |
Acarbose, Miglitol, Voglibose |
Oral tablets |
Reduces glucose absorbance by acting on small intestine to cause decrease in production of enzymes needed to digest carbohydrate |
|
4. |
Thiazolidinediones |
Pioglitazone Rosiglitazone |
Oral tablet |
Reduce insulin resistance by activating PPAR-γ in fat and muscle |
|
5. |
Amaryl mimetics |
Pramlintide |
Injectable solution subcutaneous |
Prolong gastric emptying and postprandial glucagon secretion and suppresses appetite |
|
6. |
Dipeptidyl Peptidase4 Inhibitors |
Vildagliptin Sitagliptin Linagliptin Alogliptine |
Oral tablet |
Dipeptidyl peptidase-4 (DPP- 4) inhibitors increase blood concentration of the incretin GLP-1 by inhibiting its degradation by dipeptidyl peptidase-4 |
IX. ANTIDIABETIC DRUGS
A. Oral Hypoglycemic Agents (OHAs)
- Metformin:
- Contraindications: Hypersensitivity, severe renal dysfunction (eGFR <30 mL/min/1.73 m²), metabolic acidosis, and diabetic ketoacidosis.
- Sulfonylureas:
- Contraindications: Hypersensitivity to sulfonamide derivatives, type 1 diabetes mellitus, and diabetic ketoacidosis.
- Pioglitazone:
- Contraindications: Hypersensitivity, NYHA Class III or IV heart failure, severe hepatic impairment, bladder cancer, and pregnancy.
- Alpha-Glucosidase Inhibitors:
- Contraindications: Hypersensitivity, diabetic ketoacidosis, cirrhosis, inflammatory bowel disease, ulcers, intestinal obstruction, and malabsorption disorders.
- SGLT2 Inhibitors:
- Contraindications: Hypersensitivity, end-stage renal disease (ESRD), and dialysis.
- DPP-4 Inhibitors:
- Dose adjustment: Saxagliptin requires dose reduction to 2.5 mg daily for eGFR <45 mL/min/1.73 m².
- Cycloset:
- Contraindications: Allergy, breastfeeding, and syncopal migraines.
X. LITERATURE SURVEY
- Anjan Adikari et al. (2018):
- Finding: Among 250 patients, the highest ADR occurrence (61.6%) was in the age group 46–50 years, with 70.12% being female.
- Javedh Shareef et al. (2019):
- Finding: 102 ADRs were reported from 99 patients, with male predominance (60.6%). Most ADRs occurred in the age group 40–80 years.
- Masoud Mirzaei et al. (2020):
- Finding: Current diabetes care plans are ineffective, with poor control in half of the cases. Lifestyle interventions are recommended.
- Ken Yoshikawa et al. (2020):
- Finding: Among 3,265 patients, 207 (6.3%) reported 270 ADRs, with metabolism disorders and hypoglycemia (0.52%) being common.
- Saajid Hameed et al. (2022):
- Finding: Hypoglycemia is a major concern with sulfonylureas being the primary cause. Long-term use of antidiabetics increases ADR risks.
A. Adverse Drug Reactions (ADRs)
- Insulin recipients have a higher percentage of ADRs compared to OHA users.
- Multidrug regimens may increase ADR risks and negatively impact the quality of life (QOL).
- Periodic assessments of QOL and treatment satisfaction are recommended.
- Postmarketing surveillance is crucial for understanding real-world ADRs.
B. Clinical Trials
Clinical trials for drug development are divided into five phases, each answering specific questions:
- Phase I: Study of pharmacokinetics and pharmacodynamics in humans.
- Phase II: Evaluation of drug efficacy.
- Phase III: Final confirmation of safety and efficacy.
- Phase IV: Post-marketing surveillance.
|
Drug Class |
Drug Example(s) |
Adverse Drug Reactions (ADRs) |
|
Biguanides |
Metformin |
|
|
Sulfonylureas |
Glibenclamide, Glimepiride, Gliclazide |
|
|
Insulin (Basal, Bolus, Premixed) |
Regular insulin, NPH, Glargine, Lispro |
|
|
Glucagon-like Peptide-1 (GLP-1) Agonists |
Exenatide, Liraglutide, Dulaglutide |
|
|
Alpha-glucosidase Inhibitors |
Acarbose, Miglitol |
Gastrointestinal symptoms (flatulence, diarrhea, abdominal pain)
|
XI. ADVERSE DRUG REACTION REPORTING
- ADR analysis is essential for monitoring the safety of medicines.
- Initial safety and efficacy data are derived from clinical trials, but postmarketing studies reveal ADRs in real-world settings.
- ADR reporting improves pharmacovigilance, ensuring better drug safety and efficacy profiles.
XII. TREATMENT
1) Treatment for Type 1 Diabetes
The treatment for type 1 diabetes involves insulin injections or the use of an insulin pump, regular blood sugar monitoring, and carbohydrate counting. In some cases, a pancreas transplant or islet cell transplant may be considered as a treatment option.
2) Treatment for Type 2 Diabetes
The treatment for type 2 diabetes primarily includes lifestyle modifications, blood sugar monitoring, and the use of oral diabetes medications, insulin, or a combination of both.
The four main aspects of managing diabetes are:
- Blood Sugar Monitoring: Monitoring blood sugar (glucose) levels is crucial to assess the effectiveness of the current treatment plan. Regular checks, using a glucose meter and finger stick or a continuous glucose monitor (CGM), provide valuable information to manage diabetes on a daily, sometimes even hourly, basis. You and your healthcare provider will determine the target blood sugar range.
- Oral Diabetes Medications: Oral medications are used to manage blood sugar levels in individuals who still produce some insulin, particularly those with Type 2 diabetes or prediabetes. People with gestational diabetes may also require oral medication. There are various types of oral medications, with metformin being the most commonly prescribed.
- Insulin: Individuals with Type 1 diabetes need to inject synthetic insulin to survive and control their diabetes. Some individuals with Type 2 diabetes may also require insulin. There are different types of synthetic insulin, each with varying speeds of action and durations of effect. Insulin can be administered through injectables, insulin pens, insulin pumps, or rapid-acting inhaled insulin.
- Diet: Proper meal planning and choosing a healthy diet are essential aspects of diabetes management, as food significantly affects blood sugar levels. For individuals taking insulin, carbohydrate counting is vital since the amount of carbs consumed influences insulin needs. Healthy eating habits are also crucial for managing weight and reducing the risk of heart disease.
- Exercise: Physical activity increases insulin sensitivity and helps reduce insulin resistance. Therefore, regular exercise is an important component of diabetes management for all individuals, regardless of the type of diabetes.
3) Tests for Diagnosis of Diabetes
- Fasting Blood Glucose Test: This test requires fasting for at least eight hours before taking the test, with only water allowed. Since food can significantly affect blood sugar levels, fasting helps determine the baseline blood sugar level.
- Random Blood Glucose Test: This test can be performed at any time, regardless of fasting status.
- A1c (HbA1c or Glycated Hemoglobin Test): This test provides an average blood glucose level over the past two to three months.
Conclusion
Diabetes is a progressive disease with no known cure. However, its complications can be minimized through proper awareness and timely treatment. The major complications associated with diabetes include blindness, kidney damage, and heart disease. It is crucial to maintain strict control of blood glucose levels to prevent these complications. One challenge in maintaining tight control of glucose levels is that it may lead to hypoglycemia, which can result in severe complications that are even more dangerous than high blood glucose levels. Researchers are continually exploring alternative treatment options for diabetes. The objective of this paper is to provide an overview of the current state of diabetes research. Diabetes remains a significant area of research, and the author encourages new researchers to take up the challenge and explore innovative solutions.
References
[1] American Diabetes Association. (2022). Standards of medical care in diabetes—2022. Diabetes Care, 45(Suppl 1), S1–S264. https://doi.org/10.2337/dc22-S002 [2] Ashcroft, F. M., & Rorsman, P. (2012). Diabetes mellitus and the ? cell: The last ten years. Cell, 148(6), 1160–1171. https://doi.org/10.1016/j.cell.2012.02.010 [3] DeFronzo, R. A., Ferrannini, E., Zimmet, P., & Alberti, G. (2015). International textbook of diabetes mellitus (4th ed.). Wiley-Blackwell. [4] Holst, J. J., Vilsbøll, T., & Deacon, C. F. (2009). The incretin system and its role in type 2 diabetes mellitus. Molecular and Cellular Endocrinology, 297(1–2), 127–136. https://doi.org/10.1016/j.mce.2008.08.012 [5] International Diabetes Federation. (2021). IDF diabetes atlas (10th ed.). Retrieved from https://www.diabetesatlas.org [6] Nolan, C. J., Damm, P., & Prentki, M. (2011). Type 2 diabetes across generations: From pathophysiology to prevention and management. The Lancet, 378(9786), 169–181. https://doi.org/10.1016/S0140-6736(11)60614-4 [7] Paneni, F., Beckman, J. A., Creager, M. A., & Cosentino, F. (2013). Diabetes and vascular disease: Pathophysiology, clinical consequences, and medical therapy: Part I. European Heart Journal, 34(31), 2436–2443. https://doi.org/10.1093/eurheartj/eht149 [8] Powers, A. C., Niswender, K. D., & Evans-Molina, C. (2018). Diabetes mellitus: Complications. In D. L. Kasper, A. S. Fauci, S. L. Hauser, et al. (Eds.), Harrison\'s principles of internal medicine (20th ed.). McGraw Hill. [9] Zhao, W., Wang, Y., Han, H., et al. (2021). Emerging trends in diabetes prevalence and its risk factors in China. Nature Reviews Endocrinology, 17(7), 395–404. https://doi.org/10.1038/s41574-021-00499-0 [10] Chatterjee, S., Khunti, K., & Davies, M. J. (2017). Type 2 diabetes. The Lancet, 389(10085), 2239–2251. https://doi.org/10.1016/S0140-6736(17)30058-2 [11] Kahn, S. E., Cooper, M. E., & Del Prato, S. (2014). Pathophysiology and treatment of type 2 diabetes: Perspectives on the past, present, and future. The Lancet, 383(9922), 1068–1083. https://doi.org/10.1016/S0140-6736(13)62154-6 [12] Alberti, K. G. M. M., Zimmet, P., & Shaw, J. (2007). International Diabetes Federation: A consensus on type 2 diabetes prevention. Diabetes Medicine, 24(5), 451–463. https://doi.org/10.1111/j.1464-5491.2007.02157.x [13] Nathan, D. M., & Group, D. C. C. T. E. D. (1993). The Diabetes Control and Complications Trial (DCCT): Results and implications. The Journal of Clinical Endocrinology & Metabolism, 77(9), 266–270. [14] Schwartz, S. S., Epstein, S., Corkey, B. E., et al. (2016). The time is right for a new classification system for diabetes: Rationale and implications of the ?-cell–centric classification schema. Diabetes Care, 39(2), 179–186. https://doi.org/10.2337/dc15-1585 [15] Haffner, S. M., Stern, M. P., Hazuda, H. P., et al. (1990). Cardiovascular risk factors in confirmed prediabetic individuals: Does the clock for coronary heart disease start ticking before the onset of clinical diabetes? JAMA, 263(21), 2893–2898. [16] Riddle, M. C., Gerstein, H. C., & Holman, R. R. (2017). A1C targets should be personalized to maximize benefits while limiting risks. Diabetes Care, 40(2), 163–169. https://doi.org/10.2337/dci16-0064 [17] Brownlee, M. (2001). Biochemistry and molecular cell biology of diabetic complications. Nature, 414(6865), 813–820. https://doi.org/10.1038/414813a [18] Wild, S., Roglic, G., Green, A., et al. (2004). Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care, 27(5), 1047–1053. https://doi.org/10.2337/diacare.27.5.1047 [19] Matthews, D. R., Hosker, J. P., Rudenski, A. S., et al. (1985). Homeostasis model assessment: Insulin resistance and ?-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia, 28(7), 412–419. https://doi.org/10.1007/BF00280883 [20] Zimmet, P. Z., Magliano, D. J., Herman, W. H., & Shaw, J. E. (2014). Diabetes: A 21st-century challenge. The Lancet Diabetes & Endocrinology, 2(1), 56–64. https://doi.org/10.1016/S2213-8587(13)70112-8 [21] Taylor, R. (2013). Type 2 diabetes: Etiology and reversibility. Diabetes Care, 36(4), 1047–1055. https://doi.org/10.2337/dc12-1805 [22] Rhee, E. J., & Lee, W. Y. (2021). Diabetes and cardiovascular disease: Pathophysiology and management. Diabetes & Metabolism Journal, 45(6), 737–749. https://doi.org/10.4093/dmj.2021.0300 [23] Stratton, I. M., Adler, A. I., Neil, H. A., et al. (2000). Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ, 321(7258), 405–412. https://doi.org/10.1136/bmj.321.7258.405 [24] Knowler, W. C., Barrett-Connor, E., Fowler, S. E., et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine, 346(6), 393–403. https://doi.org/10.1056/NEJMoa012512 [25] Stumvoll, M., Goldstein, B. J., & van Haeften, T. W. (2005). Type 2 diabetes: Principles of pathogenesis and therapy. The Lancet, 365(9467), 1333–1346. https://doi.org/10.1016/S0140-6736(05)61032-X
Copyright
Copyright © 2025 Arati Kishanrao Landge, Maknikar Sakshi Namdevrao, Kshirsagar Varsha Rudrappa, Prajyot Dipak Manjramkar, Mande Sandip Padmakar, Girishankar Haridas Bhavale. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET66934
Publish Date : 2025-02-12
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

