Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Radiation Awareness among Nursing Professional
Authors: Tasmiya ., Dhananjay Kumar Mishra
DOI Link: https://doi.org/10.22214/ijraset.2024.62874
Certificate: View Certificate
Abstract
: Introduction: This research aims to investigate the landscape of radiation awareness among nursing professionals through a comprehensive survey analysis. Notably, it explores variations in familiarity with different radiation types, emphasizing the importance of understanding the current state of knowledge and safety practices within this critical healthcare sector. Methodology: The study employs a survey approach to gather insights from nursing professionals regarding their awareness of radiation. The questionnaire covers diverse aspects, including familiarity with radiation types, training levels, safety incidents, knowledge of dose limits, and perceptions of cancer treatment. Recognizing its limitations, such as a modest sample size, the research relies on self-reported data to provide a snapshot of the current awareness landscape. Results: The survey analysis reveals intriguing findings among nursing professionals. X-rays emerge as the most recognized radiation type, while disparities in formal training and self-reported awareness levels become apparent. Varied knowledge concerning permissible radiation dose limits, interpretations of the ALARA principle, and perceptions of cancer treatment highlight the nuances in radiation awareness within this professional group. Despite a high recognition of lead aprons as protective equipment, the study recognizes potential limitations inherent in its design. Conclusion: In conclusion, the research contributes valuable insights into the current state of radiation awareness among nursing professionals. The study acknowledges limitations, including sample size and reliance on self-reported data. However, the findings underscore the need for targeted interventions such as continuous education, standardized safety protocols, and improved communication strategies within healthcare settings to enhance radiation awareness among nursing professionals and ensure safe and informed practices.
Introduction
I. INTRODUCTION
The discovery of X-rays by Wilhelm C. Roentgen on November 8, 1895, sparked great optimism about its potential applications beyond medicine, including in industry, agriculture, and trade. However, it is now considered anecdotal that in the 1950s, X-ray machines were used in the US, such as in shoe shops, to evaluate foot alignment within shoes. During the early days of radiation diagnostics, no one had an inkling that ionizing radiation, despite its unquestionable benefits, could have harmful effects on living organisms.[1] This study aimed to assess the knowledge of radiation protection, various radiation types, medical imaging equipment, and radiation effects among nurses in Sri Lanka for the first time. Given that nurses play a crucial role in diagnostic and therapeutic radiography as well as radiation treatment, it is essential for them to possess a comprehensive understanding of these subjects.[2] Radiation plays a crucial role in the field of medicine, serving both diagnostic and therapeutic purposes. It can be categorized into two main types: ionizing and non-ionizing radiation. Ionizing radiation encompasses electromagnetic photons with sufficient energy to induce ionization.[³'?] Certainly, to put it differently, ionizing radiation disrupts the production of cells and has the potential to damage cell functions.[?'?] According to the study conducted by the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR), approximately 4 billion X-ray examinations are performed annually.[7] Nursing care management seeks to hihlight the interconnectedness of managing, caring, and educating. It emphasizes a synergistic approach, incorporating elements such as:
Implementing and developing public policies. Managing human and material resources effectively.[8] Hence, it's crucial for nurses to be aware of potential stochastic risks associated with ionizing radiation exposure, while patients should be vigilant about both deterministic and stochastic risks.This highlights the significant role nurses play in the healthcare sector, as they are often with patients. Consequently, they may encounter radiation exposure while working behind protective barriers. From an occupational perspective, there are two likely sources of radiation exposure.[9] The maximum allowable level of occupational radiation exposure stands at 0.25 microsieverts per hour (µSv/h) or 20 millisieverts per year (mSv/y) (2). Nevertheless, a prevalent misconception among hospital personnel is the belief that all doses of ionizing radiation pose a risk to human health. Consequently, many harbor concerns regarding portable radiological examinations[10] Nevertheless, many hospital staff hold the misconception that all doses of ionizing radiation are detrimental to human health, which instills a sense of apprehension regarding portable radiological examinations.[11]
As a result, either excessive precaution or insufficient precaution may lead to significant harm for both patients and healthcare providers. Research has indicated that nurses possess limited understanding of radiation safety, exposure, and protective measures[12] Rassin et al. assessed the knowledge and attitudes related to radiation among 68 physicians and 76 nurses working in high-exposure clinical settings. Their findings revealed that over 70% of both physicians and nurses had limited understanding concerning radiation hazards, the extent of environmental radiation associated with various radiological examinations, and strategies for radiation protection.[13] Amiri et al. conducted a study on Iranian radiology technicians to assess their radiation protection strategies. The results revealed that 94.7% of the technicians focused on self-protection strategies, while only 26.3% implemented strategies aimed at safeguarding patients and other healthcare professionals.[14] Certainly, it's evident that there is a deficiency in implementing radiation safety precautions in the workplace, which leads to inadequate protective practices for workers. To address this issue, it has been suggested to establish an assessment system to ensure a reasonable level of awareness, offer appropriate training courses, strictly enforce safety procedures, and ensure the availability of all necessary radiation protective equipment and items.[15] According to a recent study conducted in Malaysia to evaluate the knowledge of radiation protection among healthcare professionals, it was found that Malaysian nurses possess sufficient knowledge about the practical application of radiation and its safety. However, there was a notable deficiency in their understanding of the physics underlying radiation. Consequently, Malaysian healthcare organizations bear a significant responsibility in ensuring that all nursing staff in Malaysia are thoroughly knowledgeable about radiation, particularly by elevating educational standards for those working with or exposed to radiation. Ultimately, these findings underscore the vital role of radiation knowledge, understanding, and education in guaranteeing the safe use of medical radiation.[16] Furthermore, comparable studies conducted in Kuwait,[17] Malawi [18] and South Africa [19] The study reported that the majority of nurses lack awareness and a comprehensive understanding of radiation risks and protection. In contrast, nurses in Saudi Arabia demonstrate a different level of knowledge and awareness regarding these aspects.[20] Shifting our focus to Finland, it's important to note that the situation regarding nurses' knowledge of radiation risks and protection may differ from what was observed in the previous context. Further research or information specific to Finland would be needed to make a comparative assessment.[21] and Nigeria [22] .
II. METHODOLOGY
A. Aim
The aim of the study was knowledge of radiation protection and radiation safety. In this study nurses were working in radiology department.
B. Study Design
A cross-sectional questionnaire survey was conducted in which data from nurses working in random hospitals, clinics, and other healthcare sectors across Punjab were collect was created using a Google Form divided with a total 20 questions.
C. Participants and Setting
A self-administered questionnaire was employed to gather data from ______ nurses employed across various healthcare settings including hospitals, and clinics. The questionnaire including inquiries about participants demographic and their knowledge regarding radiation awareness among nursing professionals equipment radiation types, radiation effects and protection. We computed the average scores for each awareness category based on respondents answers. Furthermore, determine the parentage of participants who scored above _____ and ______ in each awareness category.
III. QUESTIONNAIRE
Questionnaire responses regarding radiation awareness among nursing professionals.
- Which of the following types of radiation are you most familiar with?
-X-rays
-Gamma rays
-Ultraviolet (UV) rays
-Infrared (IR) radiation
-Radioactive particles
2. How would you rate your overall awareness of radiation safety practices in the healthcare setting?
-Very low
-Low
-Moderate
-High
-Very high
3. Have you received formal training on radiation safety during your nursing education or professional development?
-Yes, extensively
-Yes, to some extent
-No, not at all
4. How often do you use protective shielding (e.g., lead aprons) when working with radiation-emitting equipment?
-Always
-often
-Occasionally
-rarely
-never
5. Do you know the permissible radiation dose limits for healthcare workers set by regulatory agencies (e.g., the NCRP or ICRP)?
-Yes, I am aware of the limits
-I have a general idea but not the exact limits
-No, I am not aware of the limits
6. Which type of radiation is commonly used in cancer treatment to destroy cancer cells?
-Alpha radiation
-Beta radiation
-Gamma radiation
-x-rays
7. Have you ever witnessed or been involved in a radiation safety incident or near-miss incident in your workplace?
-Yes, multiple times
-Yes, once or twice
-No, never
8. In radiation safety, what does ALARA stand for?
-Always Look And Reduce Accidents
-As Low As Reasonably Achievable.
-Achieving the Lowest Allowable.
-Avoiding Leaky And Radiating Apparatus
9. What is the unit of measurement for radiation exposure dose?
-Option 1Hertz (Hz)
-Watt (W)
-Gray (Gy)
-Newton (N)
10. Which of the following imaging techniques uses ionizing radiation to create detailed images of the body's internal structures?
-MRI (Magnetic Resonance Imaging)
-CT (Computed Tomography) scan.
-ultrasound
-PET (Positron Emission Tomography) scan
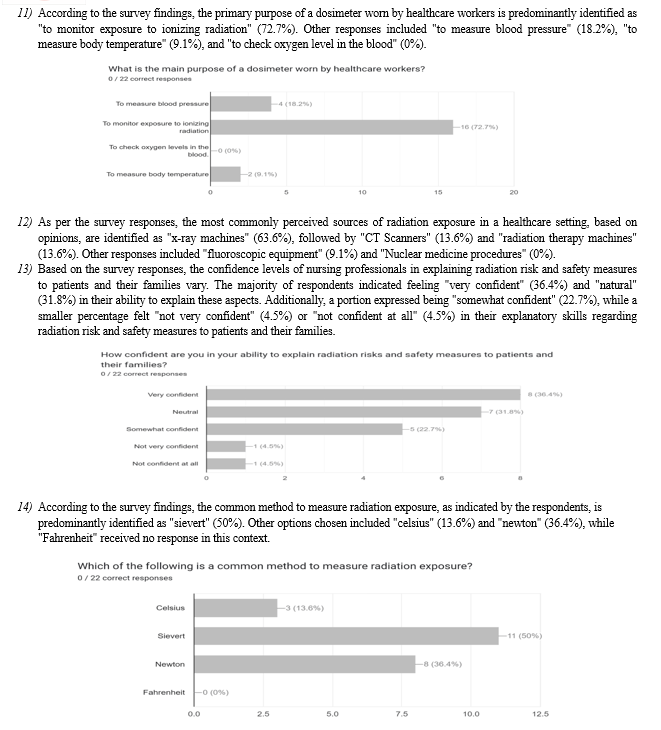
11. What is the main purpose of a dosimeter worn by healthcare workers?
-To measure blood pressure
-To monitor exposure to ionizing radiation
-To check oxygen levels in the blood.
-To measure body temperature
12. In your opinion, what are the most common sources of radiation exposure in a healthcare setting? (Select all that apply)
-X-ray machines
-CT scanners
-Fluoroscopy equipment
-Nuclear medicine procedures
-Radiation therapy machines
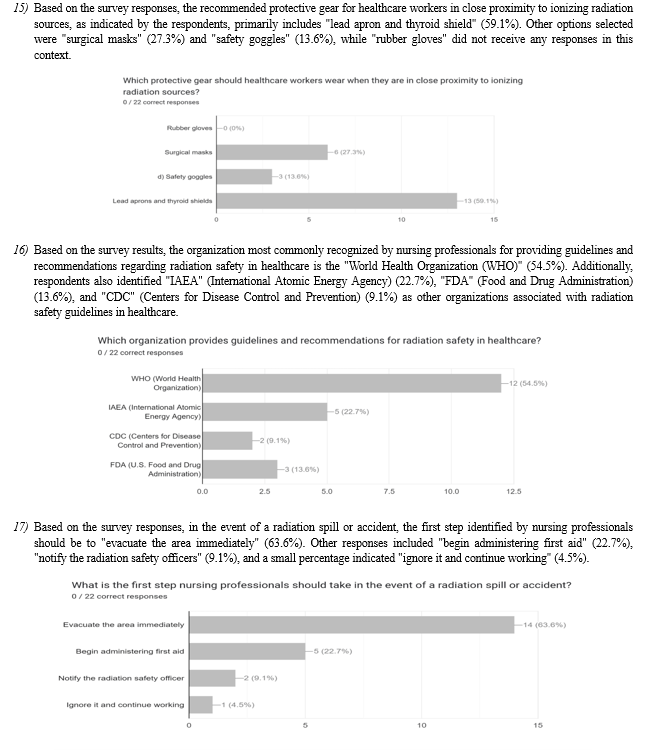
13. How confident are you in your ability to explain radiation risks and safety measures to patients and their families?
- Very confident
- Neutral
-Somewhat confident
-Not very confident
-Not confident at all
14. Which of the following is a common method to measure radiation exposure?
-Celsius
-Sievert
-Newton
-Fahrenheit
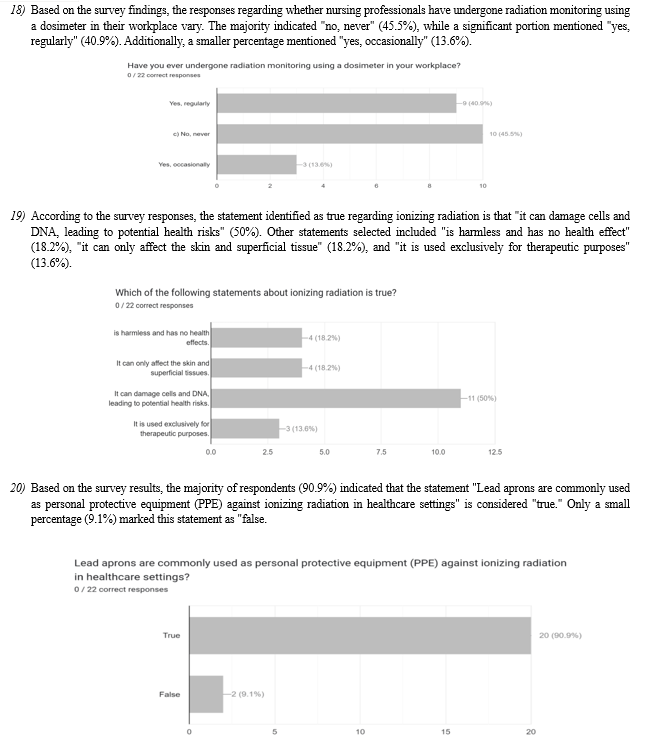
15. Which protective gear should healthcare workers wear when they are in close proximity to ionizing radiation sources?
-Rubber gloves
-Surgical masks
-Safety goggles
-Lead aprons and thyroid shields
16. Which organization provides guidelines and recommendations for radiation safety in healthcare?
-WHO (World Health Organization)
-IAEA (International Atomic Energy Agency)
-CDC (Centers for Disease Control and Prevention
-FDA (U.S. Food and Drug Administration)
17. What is the first step nursing professionals should take in the event of a radiation spill or accident?
-Evacuate the area immediately
-Begin administering first aid
-Notify the radiation safety officer
-Ignore it and continue working
18. Have you ever undergone radiation monitoring using a dosimeter in your workplace?
-Yes regular
-No, never
-Yes, occasionally
19. Which of the following statements about ionizing radiation is true?
-Is harmless and has no health effects.
-It can only affect the skin and superficial tissues.
-It can damage cells and DNA, leading to potential health risks.
-It is used exclusively for therapeutic purposes.
20. Lead aprons are commonly used as personal protective equipment (PPE) against ionizing radiation in healthcare settings?
-True
-False
IV. DATA COLLECTION
The nursing staff from various departments were invited to take part in the study, with _____ of them accepting the invitation. Data collection was conducted using Google Form, accessible to participants through a distributed message link. The responses of participating nurses were anonymous and handled in accordance with the published standards of good research practice.
VI. RESULTS
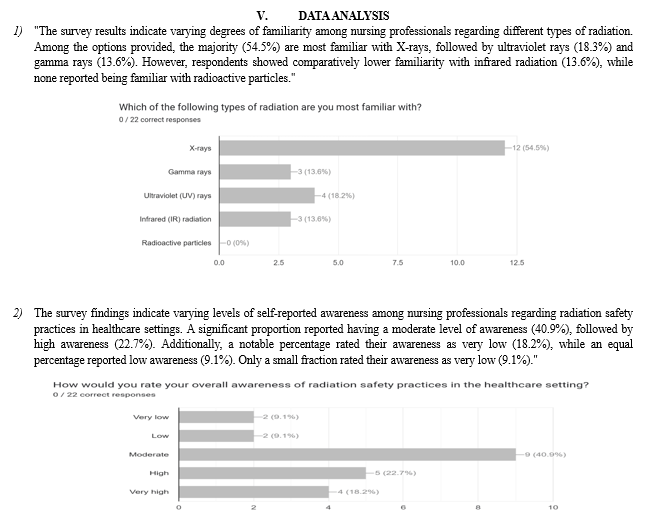
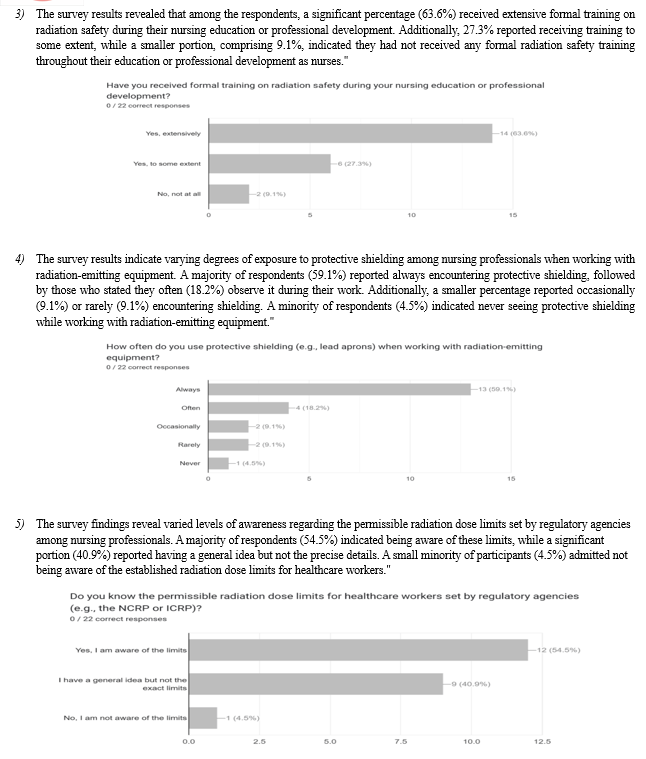
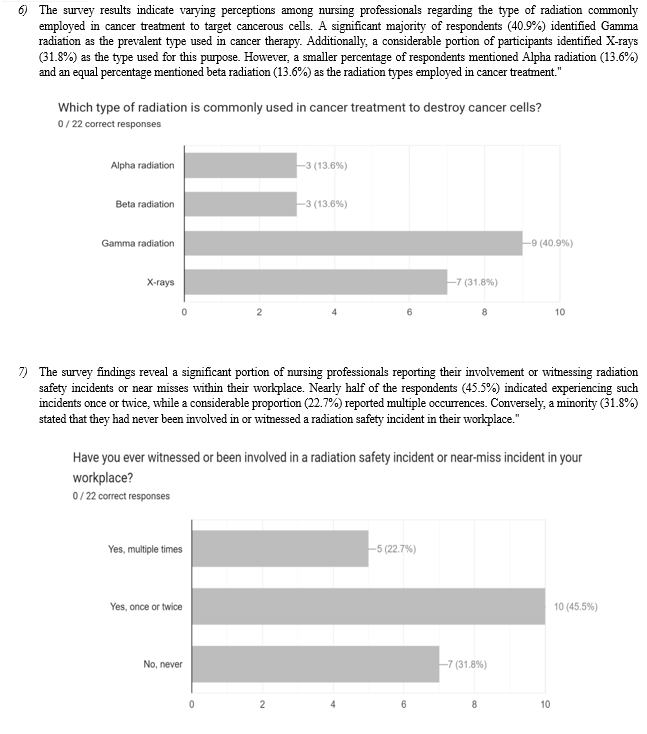
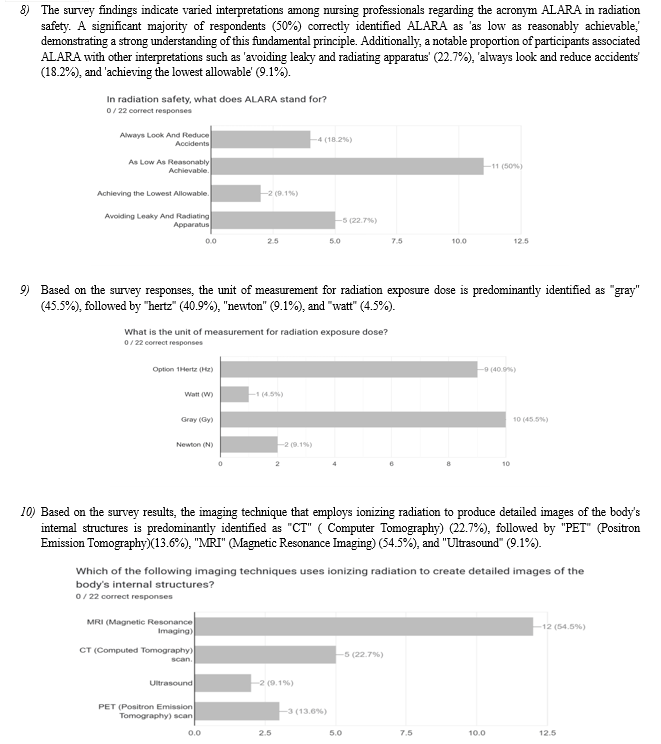
The survey analysis on radiation awareness among nursing professionals showcased varying degrees of familiarity with different types of radiation. X-rays emerged as the most recognized type (54.5%), followed by ultraviolet rays (18.3%) and gamma rays (13.6%). However, respondents demonstrated limited familiarity with infrared radiation (13.6%), and none reported familiarity with radioactive particles. Findings revealed diverse self-reported awareness levels on radiation safety practices, with 63.6% having received extensive formal training, while 27.3% received training to some extent, leaving 9.1% without any formal training. Regarding protective measures, 59.1% always encountered protective shielding when working with radiation-emitting equipment, while 45.5% reported experiencing radiation safety incidents in the workplace. Additionally, survey results unveiled varied awareness levels regarding permissible radiation dose limits set by regulatory agencies, with 54.5% fully aware and 40.9% having a general idea. In cancer treatment perception, 40.9% identified Gamma radiation as the primary type used, followed by X-rays (31.8%), while incidents related to radiation safety were reported by 68.2% of respondents. Interpretations of ALARA varied, with 50% correctly identifying it, while 22.7%, 18.2%, and 9.1% associated it with alternate meanings. Responses showed varied confidence levels in explaining radiation risks to patients, with 36.4% feeling 'very confident' and 31.8% 'natural.' The unit of measurement for radiation exposure dose was predominantly 'gray' (45.5%), and 'CT' (Computer Tomography) was the leading imaging technique using ionizing radiation (54.5%).
Organizations like WHO (World Health Organization) (54.5%) were recognized for providing radiation safety guidelines. Lastly, 90.9% confirmed lead aprons as commonly used PPE against ionizing radiation in healthcare settings."
This encapsulates the broad array of findings elucidated through the comprehensive survey conducted among nursing professionals on the critical topic of radiation awareness within healthcare settings.
VII. DISCUSSION
In discussing the findings of the survey on radiation awareness among nursing professionals, it's evident that there's a crucial need for heightened awareness within this cohort. The survey unveiled a concerning trend, indicating that a significant portion of nursing professionals lack comprehensive knowledge about radiation exposure risks, safety measures, and protocols. This knowledge gap could potentially compromise both patient care and the well-being of healthcare workers themselves. Interestingly, while a portion of respondents displayed a basic understanding of radiation safety, a notable percentage struggled with identifying appropriate protective measures and understanding the potential risks associated with radiation exposure. These findings suggest a clear imperative for improved education and training initiatives tailored specifically to the needs of nursing professionals within healthcare settings.
Moreover, the comparison with existing literature on this subject illuminates consistent patterns: many studies highlight inadequate levels of radiation awareness among healthcare professionals, with nurses often exhibiting lower levels of knowledge compared to their physician counterparts. Factors influencing this knowledge gap were also identified, including variations in educational backgrounds, limited access to ongoing training, and workplace environments that might not prioritize continuous education on radiation safety. Addressing these factors is critical in devising strategies to bridge the existing awareness gap and equip nursing professionals with the necessary knowledge and skills to ensure their safety and enhance the quality of patient care.
The implications of these findings are substantial. Insufficient radiation awareness among nursing professionals not only jeopardizes their occupational safety but also poses potential risks to patient health. With the increasing use of radiological procedures in modern healthcare, enhancing radiation awareness among nursing staff becomes pivotal in ensuring the delivery of safe and effective care. To mitigate these risks, interventions such as targeted educational programs, regular training sessions, and the integration of radiation safety protocols into nursing curricula emerge as fundamental strategies. Strengthening collaboration between healthcare institutions, regulatory bodies, and educational institutions is essential in implementing these initiatives effectively. While this survey sheds light on the current state of radiation awareness among nursing professionals, it is important to acknowledge certain limitations. The sample size and geographical representation might affect the generalizability of the findings. Additionally, self-reporting through surveys could introduce response bias, and further qualitative studies could provide deeper insights into the underlying reasons behind the observed knowledge gaps.
Moving forward, future research should delve into the efficacy of various educational interventions, explore the long-term impact of enhanced radiation awareness on patient outcomes, and investigate potential barriers to the implementation of comprehensive radiation safety programs within healthcare settings. By addressing these areas, the healthcare community can make significant strides toward bolstering radiation awareness among nursing professionals and ultimately improving both patient care and the occupational safety of healthcare workers.
VIII. LIMITATIONS
While this research paper provides valuable insights into radiation awareness among nursing professionals, certain limitations should be acknowledged. Firstly, the study's sample size may impact the generalizability of findings to a broader population. Additionally, the reliance on self-reported data introduces the potential for response bias, as participants may provide answers influenced by social desirability. The cross-sectional nature of the survey captures a snapshot of awareness levels, but a longitudinal approach could offer a more dynamic understanding of changes over time. Furthermore, the survey design may not capture the depth of certain nuanced aspects of radiation awareness. Despite these limitations, the paper contributes significantly to the understanding of the current landscape of radiation knowledge among nursing professionals.
Conclusion
In conclusion, the survey-based research on \"radiation awareness among nursing professionals\" sheds light on critical insights into the levels of knowledge and awareness within this specific cohort. The findings underscore the importance of ongoing education and training initiatives focusing on radiation safety within nursing curricula and professional development programs. Despite the identified gaps in awareness highlighted by this study, there exists a clear opportunity for interventions aimed at enhancing nurses\' understanding of radiation risks, safety protocols, and best practices. Furthermore, this research emphasizes the need for continuous evaluation and improvement of strategies to augment radiation awareness among nursing professionals, ultimately contributing to improved patient safety, enhanced quality of care, and the overall well-being of both healthcare providers and patients alike. Future studies may delve deeper into the effectiveness of tailored educational interventions or explore correlations between enhanced radiation awareness and improved patient outcomes to further support the advancement of nursing practices in this critical area.
References
[1] Ba?turkiewicz Z, Musia?owicz T. Raport CLOR nr 136. Centralne Laboratorium Ochrony Radiologicznej; Warszawa: 1999. 100 lat ochrony przed promieniowaniem jonizuj?cym. [in Polish] [Google Scholar] [2] M. Alotaibi et al. Radiology nurses\' awareness of radiation J Radiol Nurs (2006) [3] Martin CJ. The development of radiation protection. In: Martin CJ and Sutton (ed). Practical radiation protection in healthcare. New York: Oxford University press; 2002: 3-11. [4] World Health Organization. Ionizing radiation, health effects and protective measures. 2016. Available from https://www.who.int/news-room/fact-sheets/detail/ionizing- radiation-health-effects-and-protective-measures (Accessed 20 December 2019). [5] International Commission on Radiation Protection. Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Annals of the ICRP 37 (2-4). London: SAGE Publication Ltd; 2007. [6] World Health Organization. Global Initiative on Radiation Safety in Healthcare Settings. Geneva: WHO; 2008. [7] United Nations Scientific Committee on the Effects of Atomic Radiation, UNSCEAR 2008 Report: Sources and Effects of Ionizing Radiation, United Nations Scientific Committee on the Effects of Atomic Radiation, New York, NY, USA, 2010. [8] Backes M, Ribeiro LN, Amorim TS, Vieira BC, Souza J, Dias H, et al. Desafios da gestão do cuidado de enfermagem para a qualidade da atenção obstétrica e neonatal em maternidades públicas brasileiras. Atas do 6º Congresso Ibero-Americano em Investigação Qualitativa; 2017 jul 2-14; Salamanca, Espanha , 2017, p.411-20. [9] George J, Eatough JP, Mountford PJ, Koller CJ, Oxtoby J, Frain G. Patient dose optimization in plain radiography based on standard exposure factors. Br J Radiol. 2004; 77(922):858-63. [PubMed] [Google Scholar] [10] Siddiqui SS, Jha A, Konar N, Ranganathan P, Deshpande DD, Divatia JV. Radiation exposure among medical professionals working in the Intensive Care Unit. Indian J Crit Care Med. 2014;18(9):591–5. doi: 10.4103/0972-5229.140150. [PMC free article] [PubMed] [CrossRef] [Google Scholar] [11] ES, Jr, Butler PF, Applegate KE, Birnbaum SB, Brateman LF, Hevezi JM, et al. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4(5):272–84. doi: 10.1016/j.jacr.2007.03.002. [PubMed] [CrossRef] [Google Scholar] [12] Rassin M, Granat P, Berger M, Silner D. Attitude and knowledge of physicians and nurses about ionizing radiation. J Radiol Nurs. 2005;24(2):26–30. [Google Scholar] [13] Amiri F, Tohidnia M, Hormozi Z. [Principles of radiation protection in the ICU of Imam Reza Hospital of Kermansha]. . The proceeding of the first annual congress of Kermanshah University of Medical Sciences. 2011;10 [Google Scholar] [14] World Health Organization. Ionizing radiation, health effects and protective measures. World Health Organization. 2016.... [15] W.K. Sinclair Radiation protection recommendations on dose limits: the role on the NCRP and the ICRP and future developments Int J Radiat Oncol Biol Phys (1995) [16] V. Vijayakumar et al. Role of nurses in daily nuclear medicin Soc Nuclear Med (2006) [17] M.K. Badawy et al. An assessment of nursing staffs\' knowledge of radiation protection and practice J Radiol Prot (2016) [18] A.M. Rahimi et al. Malaysian nurses\' knowledge of radiation protection: a cross-sectional study Radiol Res Pract (2021) [19] Research article Investigation of radiation protection and safety measures in Rwandan public hospitals: Readiness for the implementation of the new regulations Journal of Medical Imaging and Radiation Sciences, Volume 51, Issue 4, 2020, pp. 629-638 [20] Research article Radiation Risk Awareness Among Health Care Professionals: An Online Survey Journal of Radiology Nursing, Volume 39, Issue 2, 2020, pp. 132-138 Show abstract [21] Research article Optimisation of the CT pulmonary angiogram (CTPA) protocol using a low kV technique combined with high iterative reconstruction (IR): A phantom study Radiography, Volume 29, Issue 2, 2023, pp. 313-318 Show abstract
Copyright
Copyright © 2024 Tasmiya ., Dhananjay Kumar Mishra. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET62874
Publish Date : 2024-05-28
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

