Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Review on Alzheimers Disease
Authors: Mahima Anil Nikam , Janhavi Anil Nikam , Dhanshri Sanjay Gaikwad
DOI Link: https://doi.org/10.22214/ijraset.2024.64466
Certificate: View Certificate
Abstract
Loss of Abstract Thinking Someone with Alzheimer’s disease may lose the ability to draw conclusions and solve problems. It may become difficult to balance a checkbook, for example, because the patient has forgotten what to do with the numbers. About 29.8 million people worldwide had been diagnosed with Alzheimer’s disease (AD) in 2015, And the number is projected to triple by 2050. In 2018, AD was the fifth leading cause of death in Americans with 65 years of age or older, but the progress of AD drug research is very limited. It is Helpful to identify the key factors and research trends of AD for guiding further more effective Studies. Alzheimer’s disease is a degenerative disease of the brain, the most common cause of dementia in the geriatric population, and a major cause of death. Alzheimer’s disease is one of the fastest growing risk factors in middle age, which Increases the risk of Alzheimer’s disease in coronary weddings and higher levels of Homocysteine, which can lead to withdrawal due to lifestyle changes. Cigarettes prevent Alzheimer’s disease by recalling memories. Also, despite the fact that there is no Definitive cure for Alzheimer’s, the ability to increase acetylcholine levels and reduce Ameloid beta deposition and your medications such as Donepezil has proven to be very Effective when treating Alzheimer’s disease (AD) is a progressive neurodegenerative disease. It Is characterized by progressive cognitive deterioration together with Declining activities of daily living and behavioral changes. It is the Most common type of pre-senile and senile dementia. Alzheimer disease (AD) is a heterogeneous disease with a complex pathobiology. The presence Extracellular b-amyloid deposition as neuritic plaques and intracellular accumulation of hyperphos . Phorylated tau as neurofibrillary tangles remains the primary neuropathologic criteria for AD diagnosis. However, a number of recent fundamental discoveries highlight important pathological roles For other critical cellular and molecular processes. Despite this, no disease-modifying treatment Currently exists, and numerous phase 3 clinical trials have failed to demonstrate benefits. Here ,We review recent advances in our understanding of AD pathobiology and discuss current treatment Strategies, highlighting recent clinical trials and opportunities for developing future disease modifying therapies.
Introduction
I. INTRODUCTION
Alzheimer’s disease (AD) is the most common cause of dementia and is clinically Characterized by a progression from episodic memory problems to a slow general decline of Cognitive function. In 2013, ~44 million of the world-wide population was estimated to be Affected by dementia and a steep rise to ~136 million has been predicted by 2050 2.To date, There are no treatments with proven disease-modifying effects and AD remains the largest Unmet medical need in neurology. AD pathology presents a complex interplay between Several biochemical alterations, including changes in amyloid precursor protein metabolism, Phosphorylation of the tau protein, oxidative stress, impaired energetics, mitochondrial Dysfunction, inflammation, membrane lipid dysregulation and neurotransmitter pathway Disruption. Dementia has a major negative effect on people’s functioning, Independence, and the need for care. This in turn is placing a heavy Burden on families, communities and society, with the cost of care Often paid for out-of-pocket. The personal, social and economic Consequences of dementia are enormous.
The credit for first time describing a dementing condition, Which later became known as Alzheimer’s disease, goes to German physiatrist and neuropathologist Dr. Alois Alzheimer. Alzheimer disease (AD) an aggressive form of dementia, manifesting in memory, language and behavioral deficits . According To the World Health Organization (WHO) estimates, the over all Projected prevalence in global population will quadruple in the Next decades, reaching 114 million patients by 2050 . Apart From having a great social impact, this would clearly lead to Increased economic burden to healthcare systems worldwide . It is currently estimated that 46.8 million people world-Wide have dementia with an estimated global cost of dementia Care at US$818 billion in 2010 . By 2030 it is estimated that There will be 74.7 million people with dementia, and the cost Of caring for these individuals could rise to some US$2 trillion. There are no effective options available at present for prevention and treatment of Alzheimer disease despite all scientific reports. Alzheimer’s disease progresses gradually and can last for Decades. There are three main stages of the disease, each with Its own challenges and symptoms. By identifying the current Stage of the disease, physicians can predict what symptoms can Be expected in the future and possible courses of treatment.
Each case of AD presents with a unique set of symptoms, varying in severity. Inheritance of certain genes is a risk factor for AD, with both familial and sporadic cases occurring. In sporadic AD, which is the more common form, there is a link with the Apo lipoprotein 4 (APOE4) allele, with the risk being greater in Homozygotic situations . Environmental factors, vascular Factors and psychical factors contribute to the development of Alzheimer’s disease. Currently, no drugs are available to halt The progression of neurodegeneration in Alzheimer disease; The nature of Alzheimer’s disease treatment is symptomatic .For instance, cholinesterase inhibitors (Cis) that promote cholinergic neurotransmission are used in mild to moderate cases Of Alzheimer’s disease. Memantine , an Nmethyl-D-aspartate (NMDA) receptor antagonist, is used in moderate to severe cases to prevent excitotoxicity, and antipsychotics and antidepresants are used in the treatment of neuropsychiatric symptoms . Right now, there’s no proven way to prevent Alzheimer disease. Research into prevention strategies is on going and Is getting developed day by day. The strongest evidence so far Suggests that you may be able to lower your risk of Alzheimer’s Disease by decreasing your risk of heart disease. Many of the Same factors that tend to increase your risk of heart disease Can also increase your risk of Alzheimer’s disease and vascular dementia. Important factors that may be involved include High blood pressure, high blood cholesterol, excess weight and Diabetes. Alzheimer’s disease is complex, and it is unlikely that Any one drug or other intervention can successfully lead to its Proper treatment. Current approaches focus on helping people Maintain mental function, manage behavioral symptoms, and Slow or delay the symptoms of disease. Researchers hope to Develop therapies targeting specific genetic, molecular, and cellular mechanisms so that the actual underlying cause of the disease can be stopped or prevented.
A. Normal Memory
In order to understand the complexities of dementia, it is necessary to describe what happens In normal ageing and understanding what can go wrong and gives rise to abnormal conditions Such as dementia. Ageing can be distinguished in terms of biological, social and Psychological disciplines, but there is often a great overlap and interaction between them. For Example, a physical change such as arthritis can limit mobility, which in turn can reduce involvement in social activities or other previous sources of enjoyment .The Influence of One aspect of ageing on another should also be remembered; this is important when Considering and comparing past and present cognitive functions within the same person.
Defining ‘normal’ is a difficult task and it is surprising how ‘normal’ and ‘abnormal’ activities
And attitudes often overlap. The blurring of boundaries occurs between different cultures, Different environments or even between individuals. A misconception is to consider Normality as distinct and opposite to abnormality when in fact ‘normality’ refers to the ‘range Around the middle of a dimension (eg height) with two extremes at opposite ends (very tall And very short), rather than one extreme’. Different people have their own opinion about Normality and hence expectancies in ageing are perceived differently between individuals. With the advance of medicines and technology, people are generally living longer and so More people are exposed to older people and are witness to the variations in ageing of Relatives and friends. In turn, people’s understanding of normal ageing is being constantly Revised and so too are their expectancies of themselves and others.
B. Memory functioning has been recognized as follows
Short-term and long-term memory
- Short-term memory, now elaborated into the concept of working memory , Is the system Which allows one to remember a new telephone number while one is dialing it, so long as One is not distracted
- Long-term memory allows one to remember a familiar telephone number from day to day and year to year.
- Semantic and episodic memory – Different types of knowledge appear to be stored Differently. A distinction drawn initially between episodic and semantic memories And, More latterly, a contrast between procedural and declarative memories has gained Acceptance . Episodic memories are for particular events, while semantic memories are Context-free facts. For example, knowing what I had for breakfast is an episodic memory; Knowing that the word ‘breakfast’ means a morning meal is a semantic memory
- .Declarative and procedural memory – Both semantic and episodic memories may be Subsumed under this heading (which represent the memory for facts). Procedural memory is For skills and routines and may include some types of sensory stimuli.
C. Problems with Memory
Memory failure is a common and significant problem indementia,Hence it is important to First assess the extent to which it is a problem and for whom the problem is an obstacle.
It is now believed that there are four stages involved in memory : registration, encoding, Storage and retrieval. For information to be stored in memory it must first be attended to or Registered. Encoding is the process whereby this information may be semantically encoded or Phonologically encoded,Ie encoded in terms of meaning or sound, respectively. Storage Is the process by which information is maintained in memory. It is widely accepted that Different types of knowledge appear to be stored differently, so that, for example, Knowing what a person ate for lunch (episodic memory)would be stored differently from Knowing the word ’lunch’ means a mid-day meal (semantic memory
D. Dementia
Dementia is a syndrome characterized by disturbance of multiple brain functions, including Memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgment.
Consciousness is not clouded. The impairments of cognitive function are Commonly accompanied, and occasionally preceded, by deterioration in emotional control, Social behavior, or motivation. Dementia can affect a person in different ways, and Progression of the disease depends upon the impact of the disease itself and the person’s Personality and state of health. Dementia can be divided in three stages:
- early stage – first year or two middle
- stage – second to fourth or fifth year
- late stage – fifth year and after
E. Pathology of Alzheimer’s disease
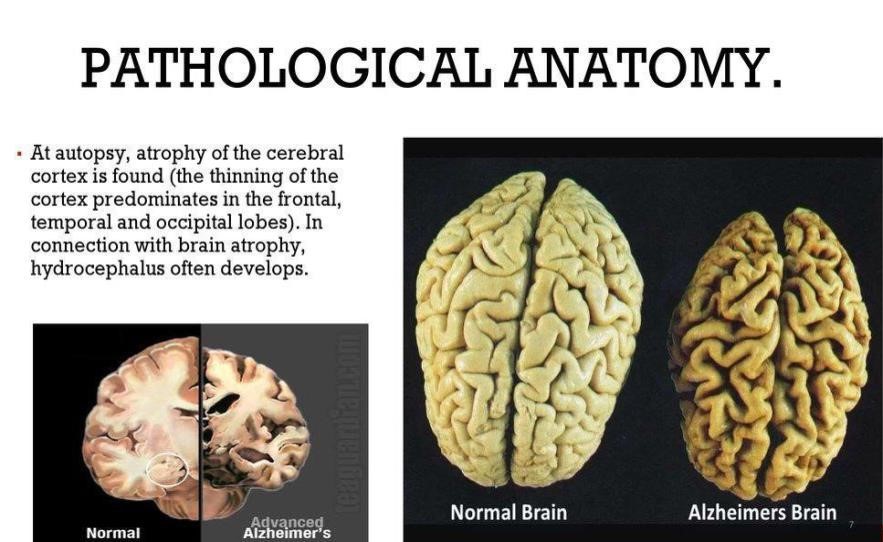
F. Macroscopic Features
The pathologic diagnosis of AD remains the gold standard for diagnosis. While certain features of AD can be Ascertained on macroscopic examination, no single feature or combination of features is specific, but certain Features are highly suggestive of AD. The AD brain often Has at least moderate cortical atrophy that is moss Marked in multimodal association cortices and limbic Lobe structures. The frontal and temporal cortices often Have enlarged sulcal spaces with atrophy of the gyri, While primary motor and somatosensory cortices most Often appear unaffected . There is increasing recognition of atrophy in posterior cortical areas in AD, most notable the precuneus and posterior cingulate gyrus, Driven in part by functional imaging studies As a result of this atrophy, there is often enlargement of the Frontal and temporal horns of the lateral ventricles as Shown in Fig. 1, and decreased brain weight is observe In most affected individuals. None of the macroscopic Features are specific to AD, and unaffected clinically normal people may have moderate cortical atrophy, Especially affecting frontal lobes, with volume loss Mostly affecting white matter . Medial temporal attrophy affecting amygdala and hippocampus, usually accompanied by temporal horn enlargement is typical of AD [18, 22, 23], but can be seen in other agerelated disorders such as hippocampal sclerosis or argyrophilic Grain disease.
Another macroscopic feature commonly Observed in AD is loss of neuromelanin pigmentation in the locus coeruleus as shown in Fig. 1. None of These observations alone are specific to AD, but often They can be highly supportive, especially in the absence of macroscopic changes specific for other neuro de generative diseases.
Table 1: Common symptoms experienced by people with dementia syndrome[
|
Early stage |
Middle stage |
Last stage |
|
The early stage is often overlooked. Relatives and friends (and sometimes professionals as well) see it as "old age", just a normal part of ageing process. Because the onset of the disease is gradual, it is difficult to be sure exactly when it begins. |
As the disease progresses, Limitations become clearer And more restricting. |
The last stage is one of nearly Total dependence and Inactivity. Memory Disturbances are very serious And the physical side of the Disease becomes more Obvious.
|
|
Become forgetful, especially regarding things that just happened |
Become very forgetful, especially of recent eventsand people's names |
Usually unaware of time and Place |
|
May have some difficulty with communication, such as difficulty in finding words |
Have difficulty comprehending time, date, place and events; may become lost at home as well as in the community |
Have difficulty understanding what is happening around them |
|
Become lost in familiar places |
Have increasing difficulty with communication (speech and comprehension) |
Unable to recognize relatives, friends and familiar objects |
|
Lose track of the time, including time of day, month, year, season |
Need help with personal care (i.e. toileting, washing, dressing) |
Unable to eat without assistance, may have difficulty in swallowing |
|
Have difficulty making decisions and handling personal finances |
Unable to successfully prepare food, cook, clean or shop |
Increasing need for assisted self-care (bathing and toileting) |
|
Mood and behaviour: may become less active and motivated and lose interest in activities and hobbies may show mood changes,including depression or anxiety may react unusually angrily or aggressively on occasion. |
Unable to live alone safely without considerable support |
May have bladder and bowel incontinence |
How Alzheimer’s spreads in the brain.
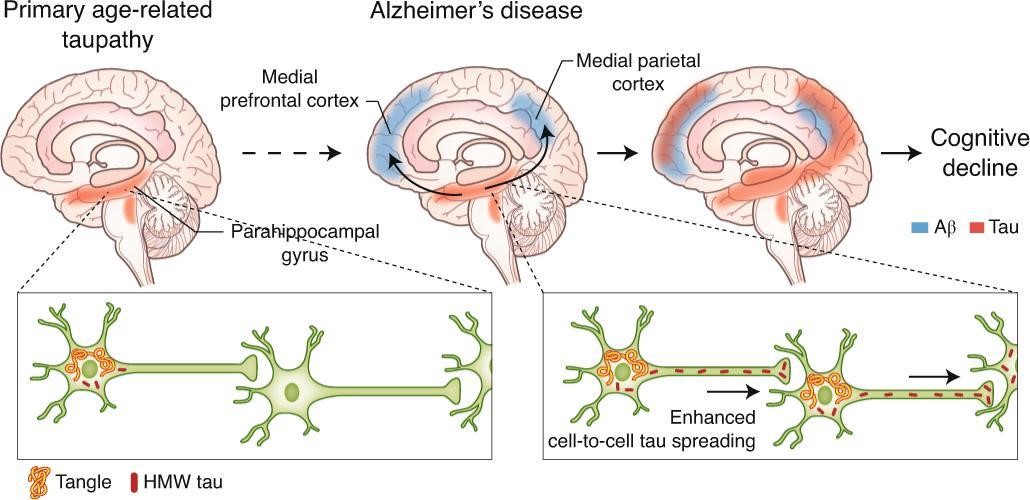
- Start
Alzheimer’s disease begins in the entorhinal cortex (EC) and hippocampus which are brain regions that important for memory.
- Spread
As the disease progresses, it spreads to other parts of the brain, including the parietal cortex, which is involved in spatial orientation and navigation.
- Damage
As more neurons die, additional parts of the brain are affected and begin to shrink. By the final stage of Alzheimer’s, damage is widespread and brain tissue has shrunk significantly.
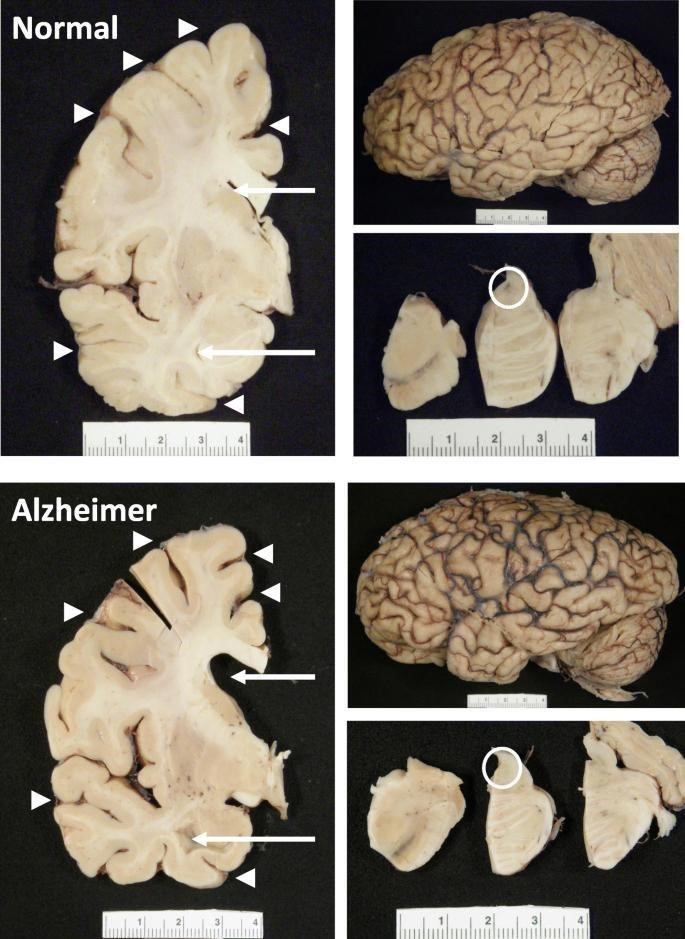
Fig 1: Shows Gross Anatomy of Alzheimer’s disease.
G. Epidemiology of AD
It is estimated that more than 47 million people in the World are affected by dementia, and as of 2018 the cost of These diseases was expected to surpass $1 trillion annually . AD is the most common form of dementia, accounting for 60 to 80% of the cases, with less than half expected to be pure AD and the majority expected to be mixed dementias . The other most common causes of dementia Include vascular dementia, Lewy body dementia and AD is a multi-factorial disease, with no single cause known, and several modifiable and non-Modifiable risk factors are associated with its development and progression.
Age is the Greatest risk factor for the development of AD. The likelihood of developing AD increases Exponentially with age, approximately doubling every 5 years after age 65. The vast Majority of individuals suffering from AD are aged 65 or older and have ‘late-onset’ or ‘sporadic’ AD (95% of all cases).Rare genetic mutations are associated with the Development of AD before age 65, which is known as ‘earlyonset’or ‘familial’ AD (B5% of All cases).People with familial forms of AD have an autosomal dominant mutation in either One of the presenilin genes locate don chromosomes 1 and 14 or in the amyloid precursor protein (APP) gene located on chromosome 21. In addition, individuals with Down’s Syndrome (trisomy 21) have an increased risk of developing early-onset AD. The genetics of Sporadic AD are more complex and less well understood. It is known that the epsilon Four allele of the Apo lipoprotein E (APOE) gene located on chromosome 19 is a risk factor for The development of sporadic AD.The prevalence of AD is higher among females, reflecting The longer life expectancy of women. Lower educational attainment has been Associated with increased risk of AD dementia,10 consistent with the idea that education Serves to increase a person’s cognitive reserve and resilience to AD pathology. A Large body Of evidence suggests that cerebrovascular risk factors play a significant role in both the Development and progression of AD; people with a history of diabetes, hypertension, obesity, And smoking have a substantially elevated risk of AD Family history of AD in first-degree Relatives and a history of head injury with loss of consciousness are also risk factors for The development of A.
H. Pathology
The pathological hallmark of Alzheimer’s disease is the presence of Amyloid plaques and
Neurofibrillary tangles (NFT). There is diffuse atrophy of the cerebral cortex and secondary
Dilatation of the ventricles. The deposits are found more at the hippocampus, temporal cortex
And nucleus basalis of Meyer net. There is loss of neurons due to the pathological changes
Leading on to reduced levels of neurotransmitters especially acetylcholine causing cognitive Deficits in these patients The basic pathological cause of Alzheimer’s disease is not fully understood and a lot of Research is being done to elucidate the basic pathological process. With the current Understanding many hypothesis are put forth for the pathogenesis of AD. The widely
Accepted among them are,
- Amyloid Cascade Hypothesis
- Tau Hypothesis
- Mitochondrial Cascade Hypothesis
I. Diagnosis of AD
In clinical settings, the diagnosis of AD is largely based on medical history, physical and Neurological examinations, and neuropsychological evaluation, as well as the exclusion of Other etiologies using selective ancillary testing. The clinical diagnosis of AD has an Accuracy of 70_90%relative to the pathological diagnosis, with greater accuracies being Achieved in specialty settings such as memory disorder clinics The cornerstone of the Clinical diagnosis is a set of consensus criteria first established in 1984 And last updated in 2011 by the National Institute on Aging _ Alzheimer’s Association (NIA_AA) workgroup.
Making a diagnosis of Alzheimer’s disease on purely Clinical grounds is challenging not only in the prodromal-mal stage in which patients only have subtle cognitive Symptoms but also in the dementia phase. Indeed, 35% Of clinically diagnosed patients with Alzheimer’s dis-Ease in a large clinical trial had negative Aβ PET scans And were misdiagnosed as having Alzheimer’s disease. Co-morbidities such as cerebrovascular disease and Hippocampal sclerosis contribute to this difficulty.
From a diagnostic standpoint, the combination of Low CSF Aβ42 levels and high T-tau and P-tau levels Is often called the ‘Alzheimer’s disease CSF profile’ and is 85–90% sensitive and specific for Alzheimer’s disease, With combined analyses providing better diagnostic
Performance than any of the CSF biomarkers alone100,101These biomarkers help to differentiate Alzheimer’s disease from important differential diagnoses, such as Depression and Parkinson’s disease, with P-tau levels Also providing substantial aid in the differentiation of Other dementias, such as frontotemporal lobar Dementia and Lewy body dementia The diagnostic Performance of these CSF biomarkers has been validated In autopsy-confirmed cohorts with similar or better Discriminatory power than in studies based on clinical Diagnoses alone.
Overall, abnormalities in biomarker measurements Can be detected 15–20 years before the estimated onset Of clinical symptoms. The predicted differences in clinical, cognitive, structural, pathological and biochemical DIAD measures are similar to measures of sporadic Alzheimer’s disease suggesting a common pathophysiology between sporadic Alzheimer’s disease and DIAD. Indeed, treatment trials in patients with DIAD Are likely to be translatable to the much more common Sporadic Alzheimer’s disease, at least the effect on specific pathological changes such as Aβ deposition, while The effect on progression of cognitive symptoms may be More variable in sporadic disease given the higher age Of patients who often have multiple co-morbidities that Contribute to the clinical symptoms. Aβ42 and Aβ40 can also be measured in the plasma, But at much lower levels than in the CSF. However, Results from studies examinine a diagnostic standpoint show consistent change and a broad overlap with cognitively normal elderly. This is probably because a substantial proportion of plasma Aβ comes from peripheral tissues and thus does not accurately reflect brain Aβ metabolism or pathology accurately reflect brain Aβ metabolism or pathology.
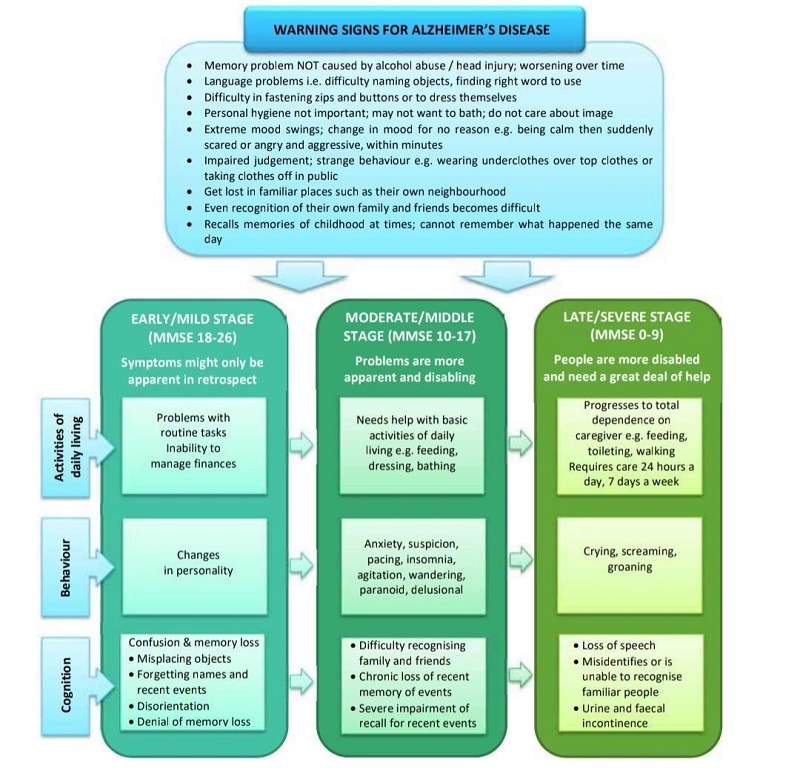
Fig : Warning signs and stages of Alzheimer’s disease .
J. Risk Factors for AD
Table 2: Factors that modify the risk of Alzheimer Disease.
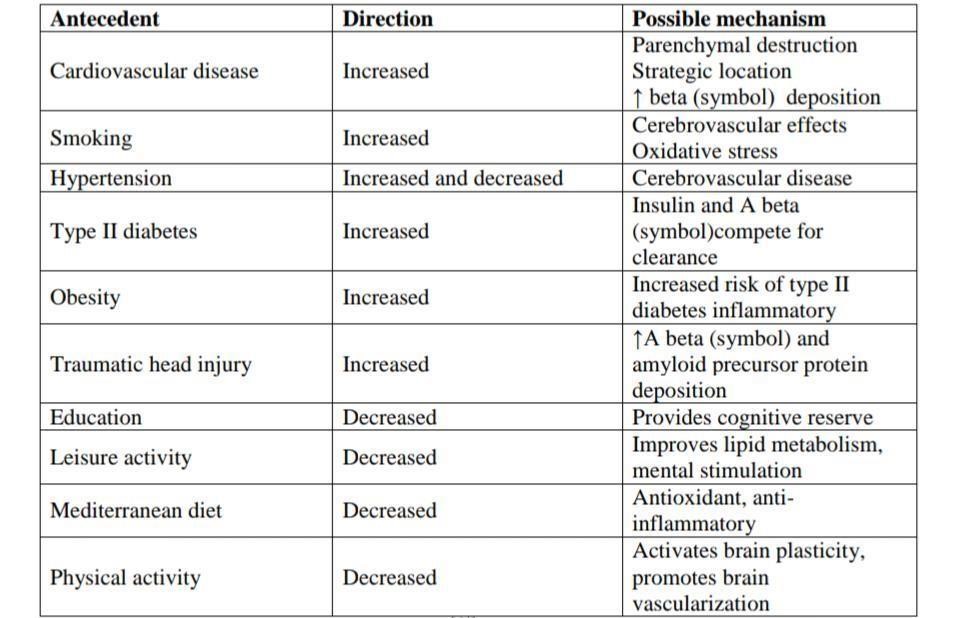
Source: Epidemiology of Alzheimer disease.
Neuropathology and clinical signs of Alzheimer’s disease .
The clinical diagnosis of Alzheimer’s disease is said tobe correct 75% to 90% of the time. According to, Accuracy is highest for neurologists specializing in memory disorders and lowest for general practitioners, who has a tendency to over diagnose Alzheimer’s disease. The clinical accuracy also tends to be lower for older patients’ who often have mixed Pathology rather than a single cause of dementia. The only clinical means of establishing a Definite diagnosis is by microscopic examination of brain tissue as there are no laboratory tests And neither sophisticated imaging techniques nor detailed neuropsychological evaluation can Specify Alzheimer’s disease categorically. Typically, the onset is from 40 years of age Onwards with insidious degeneration until death at about sixty years following onset. The Brain invariably displays a degree of atrophy; however, age-associated atrophy and the normal Variability in brain size preclude a diagnosis based solely on gross examination of the brai Atrophy of the medial portion of the temporal lobe is often disproportionate to other areas of The cortex. In most cases, the primary sensory and motor cortices are relatively spared andon Sectioning the brain, the lateral ventricles are usually dilated and the hippocampus and Amygdale are atrophic. More specific neuronal alterations accompany neuronal and Synaptic loss. The most important of these alterations is paired helical filaments which are Intraneuronalproteinaceous structures that are composed by an abnormal form of tau Protein.
Pharmacological therapy review for AD
The current pharmacologic therapy for AD only provides short-term improvement for a short Period of time, six to eighteen months.The only medicines approved in the US and several Parts of Europe for short term alleviation of symptoms are cholinesterase inhibitors and Meantime These drugs do not affect the pathology of AD, but allows the brain to Compensate for the loss of neurones that communicate via acetylcholine, a Neurotransmitter This section reviews the clinical efficacy of approved and possible Pharmacological therapies for AD.The new Medicines under development for Alzheimer Disease.
Medication such as cholinesterase inhibitors and N-methyl-D-Aspartate (NMDA)-receptor antagonists are quite effective in Managing cognitive symptoms, whereas antipsychotics and Antidepressants are more effective in on cognitive symptoms. Cholinesterase inhibitors, namely donepezil, rivastigmine And galantamine, have been shown to improve cognition. Donepezil is a piperidine derivative which specifically inhibits Acetylcholinesterase, but not butyrylcholinesterase. Rivastigmine .
Acts centrally at acetylcholinesterase and butyrylcholinesterase Sites, but has low activity at these sites in the periphery. Galant amine is a cholinesterase inhibitor that also has activity As a nicotinic receptor agonist. Memantine is an NMDA-receptor Antagonist which blocks glutamatergic neurotransmission, which May prevent excitotoxic reactions. It can be used as monotherapy, Or in combination with a cholinesterase inhibitor. Their synergistic Effect has been shown to improve cognition and activities of daily Living. Antipsychotics, especially atypical antipsychotics, have Been used to treat disruptive behaviours and psychosis in AD Patients. Antidepressants, especially selective serotonin reuptake Inhibitors, have also been used to treat depression and anxiety in AD patients.1 Paroxetine, however, causes more anticholinergic Side effects than the other selective serotonin reuptake inhibitors (SSRIs). Tricyclic antidepressants are usually avoided due to their Severe anticholinergic side effects.
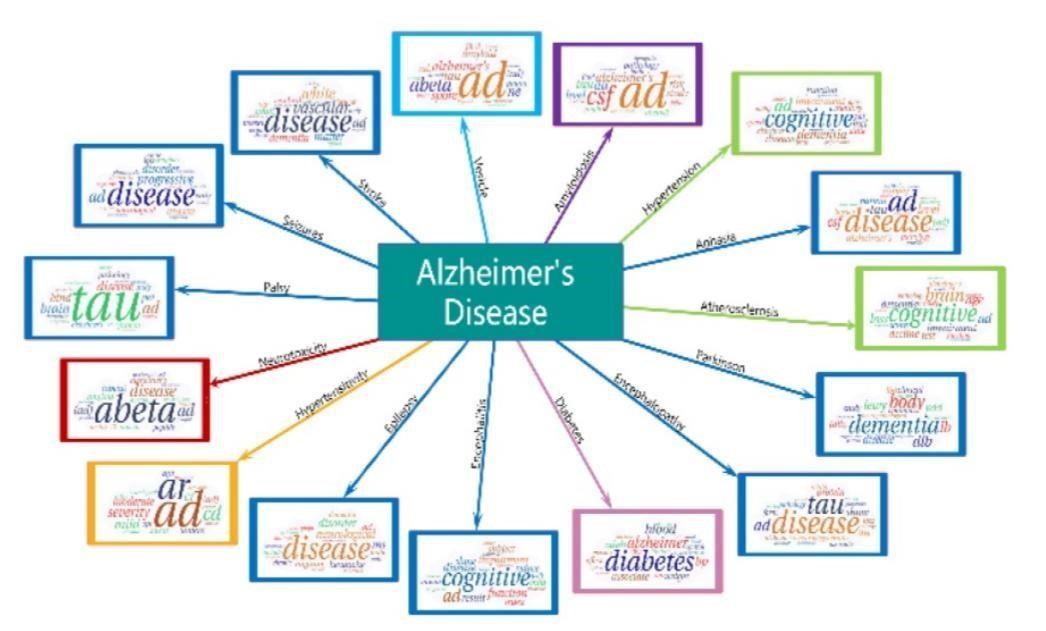
Fig: AD emerges in 15 diseases hotspots.
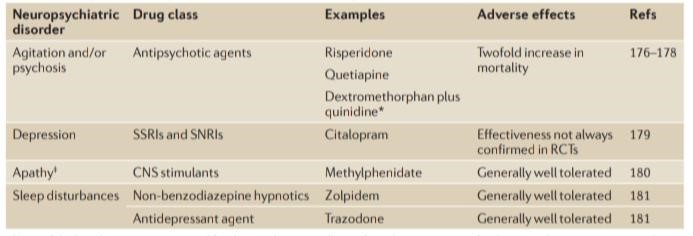
Table 3 : pharmacological management in Alzheimer disease.
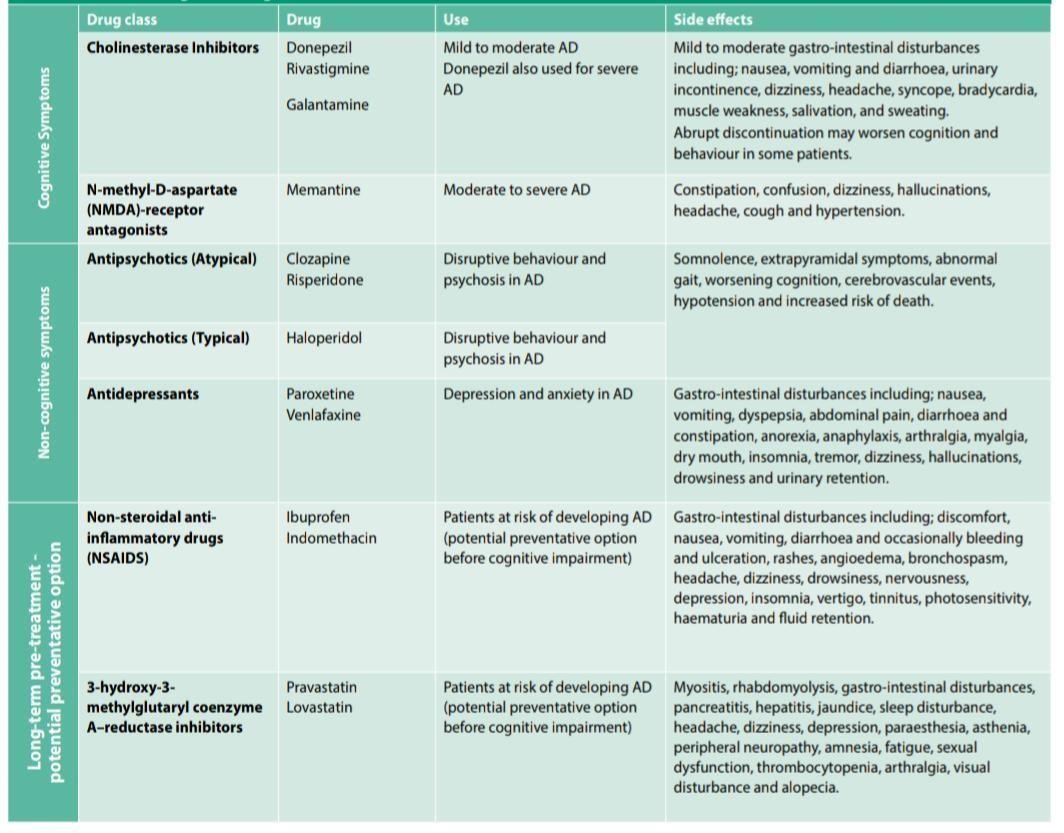
An important consideration in the treatment of AD patients is The fact that they are older patients and therefore may be taking Multiple medicines for other acute or chronic conditions. As the Number of medicines increases, the risk for potential adverse Drug effects and non-adherence also increases.1 Aside from Medicines that temporarily relieve symptoms, there is no curative Treatment available for AD.35 This is due to the complex nature of AD pathogenesis.39 Most of the symptomatic treatment attempts To improve or maintain cognition The discovery that amyloid β protein activates the complement System has indicated that inflammatory pathways somehow Contribute to the pathogenesis of AD.40 This has resulted in studies Exploring the use of anti-inflammatory agents in preventing and In slowing down the progression of AD. Studies showed that Patients who were on non-steroidal anti-inflammatory drugs (NSAIDS) were spared from AD, i.e. had reduced risk of getting AD. The longer the NSAIDS were used prior to clinical diagnosis, The greater the sparing effect.40 The mechanism behind this Effect is not fully understood, however, some hypotheses accredit The regulation of cyclooxygenase-1 (COX-1) and COX-2
as the Driving force behind the effect, since COX-1 and COX-2 levels are Elevated in AD
patients.41 Lipid-lowering agents, especially the 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors, Suapravastatin and lovastatin (but not simvastatin) have been Associated with lower prevalence of AD, and hence they may also be used to prevent on set of AD. The management of Alzheimer’s disease involves a complex interaction between the clinician, the patient, the Patient’s caregiver and the health care system in which The care is delivered. Nonpharmacological management Involves caregiver education or use of behavioural tech- Niques to optimize patient–caregiver interactions and Minimize behavioural disturbances. Pharmacological Management includes cognition-enhancing agents, Treatment of behavioural abnormalities that can arise During the course of Alzheimer’s disease and medical Management of commonly encountered systemic disorders or complications of Alzheimer’s disease. Given That medical foods and nutritional supplements form An important part of social management of patients And their family, we discuss them here as part of a Management strategy. Exercise and lifestyle-related Issues are included in comprehensive recommendation.
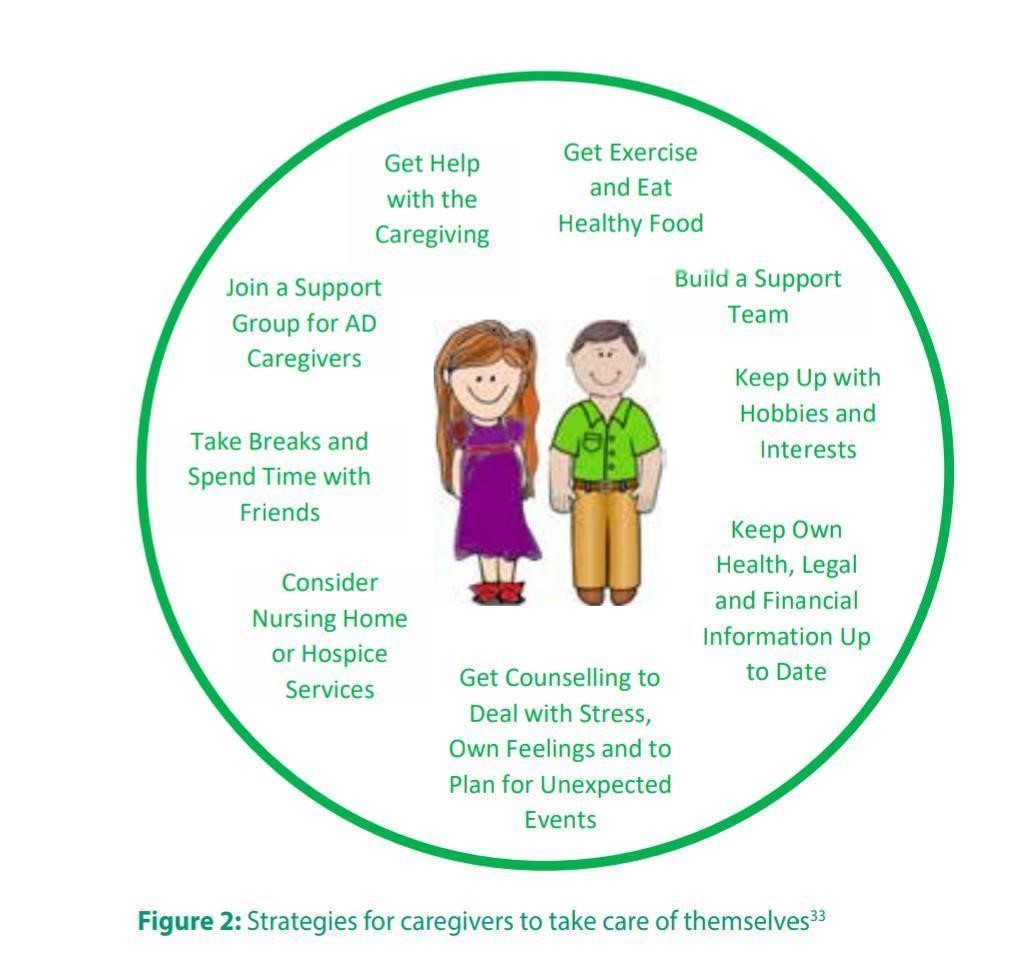
Attending to the needs of the caregiver is a crucial Component of the management of
Alzheimer’s disease. Successful management can help the patient to remain At home for a longer period of time, minimize cognitive And functional decline, optimize behaviour and improve Caregiver quality of life.
Drugs commonly used for behavioural changes in Alzheimer’s disease
|
Drug name |
Indications |
Company |
Development status |
|
ABT-126 acetylcholinesterase inhibitors |
Alzheimer disease |
About |
Phase 2 |
|
ABT-126 |
Alzheimer disease |
About |
Phase 2 |
|
LY2886721 |
Alzheimer disease |
Eli Lilly and Company |
Phase I |
|
AZD3480 |
Alzheimer disease |
Targacept Inc. |
Phase 2 |
|
AVP-923 (dextromethorphan/quinidine) |
Alzheimer disease, mild cognitive impairment |
Avanir Pharmaceuticals
|
Phase 2 |
|
MABT5102A |
Alzheimer disease |
Genentech |
Phase 2 |
|
AZD5213 |
Alzheimer disease |
AstraZeneca |
Phase 2 |
|
Gantenerumab |
Alzheimer disease |
Hoffmann-La Roche |
Phase 3 |
|
AAB-003 (PF-05236812) |
Alzheimer disease |
Pfizer |
Phase I |
|
BMS-241027 |
Alzheimer disease |
Bristol-Myers Squibb |
Phase I |
|
MABT5102A |
Alzheimer disease |
Genentech |
Phase 2 |
|
BIIB037 |
Alzheimer disease prodromal or mild |
Biogen Idec |
Phase I |
|
|
AD |
|
|
|
GSK2647544 |
Alzheimer disease |
GlaxoSmithKline |
Phase I |
Table 4: New Medicines under Development for Alzheimer disease:
Sources: Evaluation of Medicinal Products (EMEA) http://www.ema.europa.eu/ema/[69] and The US Food and Drug Administration (FDA) http://www.fda.gov/.
Conclusion
Alzheimer’s disease is the most common form of dementia in Older adults. The disease is extremely complex, with causes Not fully understood. Patients progress through degenerative, Irreversible phases of the disease, while cognitive functioning (memory, thinking and reasoning) and behavioural abilities Are affected, up to the point where the person must depend Completely on others for basic activities of daily living. To reveal the hotspots and trends of AD, we Proposed a novel LDAP framework which combines Topics model and AP algorithm. From about 100,000 AD papers, we found the spotlights of AD research including 556 genes, 15 diseases, 15 amino acids, Peptides, and proteins, 19 chemicals and compounds, 33 symptoms and phenomena, and 12 related Pathways. We studied the research hotspots via a Visualization method to find the regularities, and Reveal the research hotspots on AD research. It should Be noted that there is no unique criteria to explain the Trends of AD. The use of any measure for the clinical assessment of dementia, whether in people with Learning disabilities or in the ‘normal’ population carries with it limitations. Informed Knowledge of these limitations allows use scientific choices which enable us to tailor our Neuropsychological battery or adopt alternative measures.Ultimately, there may be a compromise because of these limitations; however, scientific Understanding has given us a better picture of the course of dementia than ever before. With The advancement of technology, such as MRI and fMRI, and PET and SPET scans, used in Conjunction with neuropsychological tests administered at key time points including follow-Ups, the clinician is better placed to make a more reliable diagnosis and prognosis than in the Past. It is hope that this will also enlighten service providers in widening access to people With learning disabilities who also have dementia.Current Pharmacological treatment used in the management of AD may Ease the symptoms for a period of time, but do not stop the Persistent downward progression of the disease. Patients may Benefit from nonpharmacological strategies tailored to the needs Of the individual person. Ongoing research indicated that specific Precautionary measures, i.e. higher education and improved heart Health, are most likely to delay the onset of AD. The urgent need For drug development is echoed by the words of Margaret Chan, The Director General, World Health Organization “I can think of no Other disease where innovation, including breakthrough discoveries To develop a cure, is so badly needed.”
References
[1] X. Chen, S.D. Yan, Mitochondrial abeta: a potential cause of metabolic dysfunction in [2] Alzheimer’s disease, IUBMB Life 2006; (58): 686–694. [3] Alzheimer A. UbereineeigenartigeErkrankung der Hirnridne [About a Peculiar Disease of [4] The Cerebral Cortex]. Allg Z Psychiatr 1907; 64: 146-48. [5] Alzheimer A. About a peculiar disease of the cerebral cortex. Alzheimer Dis AssocDisord 1987; 1: 38. [6] Maurer K, Volk S, Gerbaldo H. Auguste D and Alzheimer’s disease. Lancet 1997; 349(9064): 1546-9. [7] Alcott, D. ‘Normal Aging’ in Stokes, G. &Goudie, F. (eds), Working with Dementia,Oxford: Winslow Press, 1993; 9-15. [8] Allen, P.A., Smith, A.F., Jerge, K.A. & Vires-Collins, H. ‘Age differences in mental [9] Multiplication: Evidence for peripheral but not central decrements’, Journal of Gerontology, 1997; 52(2): 81-90 [10] Pardridge WM. Blood Brain Barrier and new approaches to brain drug delivery. Thewesternjournal of medicine. 1992; 156(3): 281 – 286. [11] Freidl, W., Schmidt, R., Stronegger, W.J. & Reinhart, B. ‘The impact of Sociodemographic, environmental, and behavioural factors, and cerebrovascular risk Factors as potential predictors of the Mattis Dementia Rating Scale’, Journal of Gerontology. 1997; 52(2): 111-116. [12] Craik, F.I.M. ‘Memory changes in normal aging’, Current Directions in Psychological Science, 1994; 3(5): 155-158 [13] Nyberg, L., Backman, L., Erngrund, K., Olofsson, U. & Nilsson, L. G. ‘Age differences in Episodic memory, semantic memory, and priming: relationships to demographic, Intellectual, and biological factors’, Journal of Gerontology. 1996; 51(4): 234-40. [14] Morris, R.G. ‘Recent developments in the neuropsychology of dementia’, International Review of Psychiatry. 1994b; 6: 85-107. [15] Mitrushina, M., Uchiyama, C. &Satz, P. ‘Heterogeneity of cognitive profiles in normal Aging: implications for early manifestations of Alzheimer’s disease’, Journal of Clinical And Experimental Neuropsychology. 1995; 17(3): 374-382 [16] American Psychiatric Association; Diagnostic and Statistical Manual of Mental Disorders. 1980; 112. [17] Emilien and Grard, et al. Alzheimer Disease: Neuropsychology And Pharmacology. Basel: Birkhauser. 2004. [18] What Is A PET Scan? How Does A PET Scan Work? Medical News Today: Health News. 2009. [19] Small GW Neuroimaging and Genetic Assessment for Early Diagnosis of Alzheimer’s disease. Journal of Clinical Psychiatry. 1996; 57: 9-13. [20] Nordberg A PET Studies and Cholinergic Therapy in Alzheimer’s Disease. Rev Neurol, National Center for Biotechnology Information. 1999; 4: 53-63. [21] Beyenhof and Lauren. How a CT Scan Works. Helium – Where Knowledge Rules. Web. 2010. [22] Khachaturian, Zaven S, and Teresa SR. Alzheimer’s Dis-Ease: Cause(s), Diagnosis, Treatment, and Care. Boca Raton:CRC.1996. [23] Gould, Todd A, and Molly Edmonds Discovery Health “MRI Mag-MedDocs Publishers Annals of Biotechnology 7 Nets”. Discovery Health. Web. 2010. [24] Gosche KM. et al. Hippocampal Volume as an Index of Alzheimer [25] Neuropathology: Findings from the Nun Study. Neurology. 2012;58: 1476-1482. [26] Mellon EA, Pilkinton DT, Clark CM et al. Sodium MR Imaging Detection of Mild Alzheimer’s Disease: Preliminary Study. American Journal of Neuroradiology. 2009; 30: 978-984. [27] Thies W and Bleiler L Alzheimer’s disease facts and figures. Alzheimer’s Dement.2013; 9: 208-245. [28] Francis PT, Palmer AM, Snape M et al. The cholinergic hypothesis Of Alzheimer’s disease: a review of progress. J NeurolNeurosurg Psychiatry. 1999; 66: 137-147. [29] Corbett A, Williams G and Ballart C. Drug repositioning: an Opportunity to develop novel treatments for Alzheimer’s disease.Pharmaceuticals. 2013; 6: 13041321. [30] Rogawski MA and Wenk GL. The neuropharmacological basis for the use of Memantine in the treatment of Alzheimer’s disease. CN Drug Rev. 2003; 9: 275308. [31] Hsiao K, Chapman P, Nilsen S, Eckman C, et al. Correlative memory deficits, Aß elevation, and Amyloid plaques in transgenic Mice. Science. 1996; 274: 99102. [32] Lacor PN, Buniel MC, Furlow PW, et al. Abeta oligomer-induced Aberrations in synapse composition, shape, and density provide A molecular basis for loss of connectivity in Alzheimer’s disease. J Neurosis. 2007; 27: 796-807. [33] Lambert MP, Barlow AK, Chromy BA, et al. Diffusible, nonfibrillar Ligands derived from Abeta1-42 are potent central nervous system neurotoxins. ProcNatlAcadSci USA. 1998; 95: 6448- 6453. [34] Mudher A, Lovestone S. Alzheimer’s disease-do tauists and Baptist finally shake hands? Trends Neurosis. 2002; 25: 22-26. [35] Trojanowski JQ and Lee VMY. The Alzheimer’s brain: finding outWhat’s broken tells us how to fix it. Rous-Whipple Award Lecture. 2005; 167: 1183-1188. [36] Birks J Cholinesterase inhibitors for Alzheimer’s disease. Co-Chrane Database Syst Rev (1): CD005593. 2006. [37] Courtney C, Farrell D, Gray R, et al. Long-term donepezil treatment in 565 patients with Alzheimer’s disease: randomized double-blind trial. Lancet. 2000; 363: 2105-2115. [38] Cummings J, Froelich L, Black SE, et al. Randomized, double-Blind, parallelgroup, 48-week study for efficacy and safety of A higher-dose rivastigmine patch (15 vs. 10cm2) in Alzheimer’s Disease. Dement GeriatrCognDisord. 2012; 33: 341-353. [39] Maidment ID, Fox CG, Boustani M, et al. Efficacy of Memantine On behavioral and psychological symptoms related to dementia: A systematic metaanalysis. Ann Pharmacother. 2008; 42: 32-38 [40] Zec RF and Burkett NR. Non-pharmacological and pharmacologically treatment of the cognitive and behavioural symptoms of Alzheimer disease.NeuroRehabilitation. 2008; 23: 425-438. [41] Vigen CL, Mack WJ, Keefe RS, Sano M, et al. Cognitive effects of Atypical antipsychotic medications in patients with Alzheimer’s Disease: outcomes from CATIE-AD. Am J Psychiatry. 2011; 168:831-839. [42] Van Marum RJ Current and future therapy in Alzheimer’s disease. FundamClinPharmacol. 2008; 22: 265-274. [43] Weksler ME. The immunotherapy of Alzheimer’s disease. Immune Ageing. 2004; 1: 2. [44] Porsteinsson, A. P. et al. Effect of citalopram on Agitation in Alzheimer disease: the CitAD randomized Clinical trial. JAMA 311, 682–691 (2014). [45] Rosenberg, P. B. et al. Sertraline for the treatment Of depression in Alzheimer disease. Am. J. Geriatr.Psychiatry 18, 136–145 (2010). [46] McCleery, J., Cohen, D. A. & Sharpley, A. L. Pharmacotherapies for sleep disturbances in Alzheimer’s disease. Cochrane Database Syst. Rev. 3, CD009178 (2014). [47] Lanctot, K. L. et al. Effect of methylphenidate on Attention in apathetic AD patients in a randomized,Placebo-controlled trial. Int. Psychogeriatr. 26, 239–246 (2014).
Copyright
Copyright © 2024 Mahima Anil Nikam , Janhavi Anil Nikam , Dhanshri Sanjay Gaikwad . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET64466
Publish Date : 2024-10-05
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

