Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
A Critical Review on Role of 3D-Printer in Cardiology
Authors: Pradumna Kalal
DOI Link: https://doi.org/10.22214/ijraset.2023.56203
Certificate: View Certificate
Abstract
The focus of recent studies has been on 3D printing technologies. Models are manufactured using magnetic resonance imaging, computed tomography, or echocardiography in three dimensions (3D printing) , and the process is also known as additive manufacturing. The debate about 3D printing\\\'s function in cardiology is the main focus of current studies . To decrease the mortality rate due to heart related diseases like cardiac arrest , which has been tremendous in recent times, 3D printed models serve as a savior of life. To illustrate, during COVID-19, the coronavirus created a global pandemic and a huge global demand for medical equipment. The shortage of time and the high level of social distancing make it difficult for the government and medical professionals to face the pandemic. In those critical times, 3D printing models were used to develop medical equipment and explore its potential by addressing the shortage of equipment. The physical models are printed using various methods like Fused Deposition Modeling, Polyjet, Stereolithography, Selective Laser Melting, and Sintering. This also enhances the practical knowledge of students and surgeons and revives confidence in the patients and their families.
Introduction
I. INTRODUCTION
Additive manufacturing is a novel manufacturing technique that uses material-adding technology. Accurate and precise components which are needed in the medical field can be easily manufactured by using 3d printing technique. Sintering, melting, and stereolithography are the three basic subcategories of additive manufacturing. Sintering is a process that uses metal powder to heat a material before it melts in order to make high-intensity objects. Direct metal laser sintering utilizes metal powder, whereas selective laser sintering utilizes thermoplastic powders. Direct energy deposition, powder bed fusion, and electron beam melting are a few examples of melting processes. Electric arcs, electric beams, and lasers are used to melt the materials and print the objects. This is in contrast to stereolithography, which relies on the principle of photopolymerization to cure and solidify the cross-section of objects by using the proper light source to interact with the materials selectively. Globally, 3D printing has brought about significant change as technology has developed beyond producing manufacturing materials for the medical sector and has become more broadly available.
In the manufacturing industry, 3D printing is crucial, and it has been suggested as a quick and affordable approach to replicate patient-specific anatomy for instruction, training, pre-procedural planning, and spatiotemporal mapping (11), (33).

This article primarily focuses on applications in cardiology, but 3D printing offers a wide range of medical applications. Due to the delayed medical help during COVID-19, the complexity of heart-related issues has recently increased. The importance of 3D printed models increases because they provide preoperative visualization and practice, which improves the surgeon's understanding of the disease and anatomical variations(5) (33). Three-dimensional printing has applications in cardiology, particularly when combined with 3D echocardiograms, computed tomography (CT), or magnetic resonance imaging (MRI).CT offers cardiovascular systems great degrees of spatial resolution, high-quality images, and simple image segmentation (5). Due to the lack of realism, it is constrained and is best viewed on a computer screen. It cannot be handled physically (37). AI is most typically utilized in cardiology.
Magnetic-resonance imaging has higher temporal resolution and less radiation, but it takes prolonged time and is contraindicated for some patients. (20). MRI and CT have some cost constraints as they are expensive compared to 3D echocardiography(44) While there are many benefits to echocardiography, such as clearer AV valve imaging, cheaper costs, greater temporal resolution, and less radiation, there is also positive about the potential for 3D printing in the future. Compared to MRI or CT, 3D printing from echo is more difficult due to a number of technological issues (24). After 30 years of testing, this technology is now being used in massive quantities (3). Cardiac 3D printing is a cutting-edge tool that increases patient counseling and student education. Cardiovascular defects, transcatheter aortic valve replacement (TAVR), congenital heart disorders (CHD), hypertrophic cardiomyopathy (HCM), and other conditions related to cardiovascular illness can be addressed with 3D printing technology. When it comes to surgical and interventional planning for CHD, 3D printing not only offers procedural planning with greater vision but also delivers crucial information about the precision of surgical reconstruction and device implantations(2) (40).
II. ROLE OF 3D PRINTING IN CARDIOLOGY
The 3D printed CHD model is used in medical education like cardiac diseases, septal defects , congenital diseases, surgical planning and simulation(17). Cardiology diseases are diaphanous and are mainly analyzed into the following categories:
A. Cardiovascular Diseases
Heart and blood vessel diseases that continue to pose a serious hazard to human health are collectively referred to as cardiovascular diseases (CVD). Heart disease 3D printed models are useful for practical simulation of surgical intervention. This procedure entails employing printers to transform digital signals into physical models (16).
The treatment of cardiovascular disorders uses 3D printing materials like PLA and ABS. These materials are reasonably priced and can depict certain heart architectures while having extremely different levels of hardness and flexibility (20).
Applications for 3D printing in cardiovascular treatment span from the treatment of aortic and persistent vessel disorders to complex pediatric and adult congenital heart ailments and common coronary heart diseases (3). Echocardiography is the most commonly used imaging method for CHD (8). Congenital great artery transpositions (Levo-TGAs), Dextro-TGAs, unbalanced atrioventricular canals, Tetralogy of Fallot (ToF), truncus arteriosus, total anomalous pulmonary venous return (TAPVR), and partial anomalous pulmonary venous returns (PAPVR) are among the conditions that can be treated by 3D printing in CHD patients. In addition to the hemodynamic obstruction of the left ventricular outflow tract (LVOT), as well as the difficulty of the operation due to complex anatomical relationships of hypertrophic cardiomyopathy (HCM) and poor visualization of the left ventricular cavity, 3D printing can be used primarily to treat hypertrophic cardiomyopathy.(18).
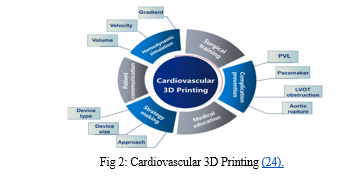
3d-printed models of predominant cardiac neoplasms have been utilized in identifying the cardiac tumor growth and structures which are at risk to determine appropriate surgical methods and, additionally, in valve-in-valve procedures(3). Likewise, it can be used to prevent tricuspid regurgitation (TR) on the right side of the valve. (1).
B. Congenital Heart Disease
Congenital heart disease (CHD) is the term used to describe anomalies in the anatomical structure of the cardiovascular system brought on by aberrant cardiovascular development during the embryonic stage. It is one of the main causes of illness and death in infants. There are currently more adults than children who have CHD. Because of the plaque (fatty substances) that blocks the arteries, it is also known as coronary artery disease (CAD) (17).
When performing transcatheter aortic valve replacement (TAVR) procedures, 3D printed models are used to size the TAVR devices that are helpful for in vitro implantation and replicate the hemodynamic parameters of each patient (19). A 3D-printed model of the coronary arteries is used to place stents in regions with low WSS (Wall Shear Stress) and good hemodynamics. (20). Coronary artery models, like the Nitinol stent, play a big part in creating enough scaffolding forces to keep open channels open. If the stent position were pre-tested in the 3D printed model, it would be simple to place (46). These models are employed in both pre- and post-operative settings (45).
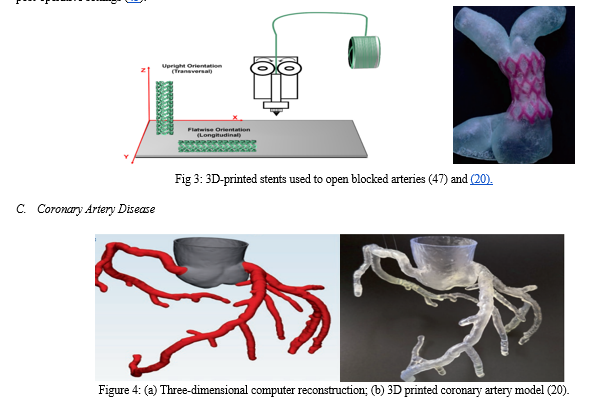
Due to the buildup of plaque, the blood arteries of the heart are where coronary artery disease is most commonly observed. Coronary artery fistula and coronary atherosclerosis are two of the most prevalent coronary artery disorders (20). The primary use is for the treatment of complicated coronary abnormalities using guidance. In both pediatric patients and adults, congenital cardiac disease foreshadows the lifetime accumulation of radiation exposure (39). The 3D printed models of coronary artery illnesses promote interventional coronary operations and are also helpful in better educating patients about their ailments (38).
Polydimethylsiloxane (PDMS) models of coronary arteries are used to evaluate computer simulations of stent implantation and test stenting techniques(15) (43). To see the calcified plaques and coronary stenting, the best coronary CT scanning techniques are evaluated using 3D printed coronary models. CAD is identified with coronary CT angiography. (38).
D. Aortic Aneurysm and Aortic Dissection
Its use in building accurate models of the aorta allows for the modeling of surgical operations like endovascular stent grafting(37) (38). With a mock circulatory system, aneurysms can be treated and diagnosed using 3D printed models(43). I would rather give condolences to the affected patients and their families. 3D printed models assist clinical diagnosis and generate customized prostheses and implants. (37) To visualize the calcified plaques and coronary stenting, the assessment of the best coronary CT scanning Techniques using 3D printed coronary models are carried out. CAD can be diagnosed using coronary CT angiography (25). There are several uses for it, ranging from orthopedics and cancers to cardiovascular disorders such as congenital heart disease, coronary artery disease, pulmonary embolism, aortic aneurysm, aortic dissection, and aortic valvular disease, which all have 3D printed models (3) (8).
E. Pulmonary Artery Disease
The condition known as pulmonary heart disease interferes with the heart's capacity to pump blood to the lungs. Applications include congenital cardiac disease with anomalies such as coronary-pulmonary artery fistula or pulmonary atresia or stenosis (9) (38). Intricate pulmonary valve procedures also employ 3D-printed anatomical models (13).
A creative application of 3D printing to identify pulmonary emboli with the goal of creating the best CT pulmonary angiography (CTPA) procedures (38).
III. OVERVIEW
Current work focuses on cardiology due to the increasing complexity of cardiac conditions and its limitations. A developing technique called three-dimensional printing is essential to the development of improved medical treatments. In order to better comprehend the structure of the heart and to facilitate communication between patients and doctors, 3D printed models are useful. With the cost being the main constraint, the reduction in it,that is the printing materials, will be the acceptable technique for both the patients and clinicians(38). Two different versions of the 3D heart models were sculpted. The replica organs' outer surface is the first consideration. Second, the amount of blood that is replicated inside the heart chambers (14). This technology has been utilized to properly diagnose congenital heart abnormalities as well as vascular coronary heart disease, and to develop treatments and surgical procedures that improve understanding of anatomic linkages (1). In the past, doctors used printed documents, movies, and interactive activities to connect with patients. Only general ailments are addressed by these approaches, not specific situations. By using 3D printers to reconstruct patients' hearts, it is possible to develop transcatheter mitral valve implantation and repair techniques.(2). It enhances interaction with patients and their families and increases patient participation in knowing their own conditions and contributing to their own decision-making (3). Models are initially made using traditional techniques like casting and molding. However, they come at a significant cost to creating a single cast, take a long time to prepare, and have a limited amount of resolution. To address this, 3D printing was created, which uses a low-cost, layer-by-layer construction method (15).

Current literature seems to support high-quality management and training in cardiovascular remedy and surgical treatment (2). The models of 3D printing for cardiac diseases may provide effective educational tools. They provide more information and include sessions for students in medicine, which provides educators with more comprehensive and accurate models than 2D models (42). Decision-making and intraoperative orientation depend heavily on 3D printed models (23). It offers high-quality pre-and post-procedural virtual management and medical education. Additionally, it teaches doctors how to properly handle and manage leads and catheters before doing surgeries (2)(73). Using echocardiographic data, 3D printed heart models can be created that are specific to the patient. (26).
Future 3D printed tissue models must be of the highest caliber in terms of both biological and technological factors if all the objectives are to be met (32)(72). In terms of proof-of-principle, 3D printing has the capacity to create intricate patterns from computer-aided files, making it feasible to create identical replicas of patient tissues. Bioprinting has had a big influence on the cardiac area (28)(71). According to research conducted under standard learning settings, 3D prints are more inclined to be handled than actual cadaveric material since they are colorful, and they do not disadvantage students studying external cardiac anatomy when compared to traditional cadaveric materials (31).
The primary benefit of 3D printing is that it can be used to create small structures from which we can physically see various cell arrangements or the building blocks of tissues in a single step(32). It also reduces complications like blood loss, organ ischaemia time, anesthesia time, and operating room time(3), which lowers medical errors and improves patient safety (33) . The use of 3D printing will enhance the detection and treatment of heart illnesses while continuously changing the conventional therapy approaches (23) (24).
IV. WORKFLOW
Charles Hull initially suggested the concept of three-dimensional printing in 1986. Since then, a broad range of 3D printing techniques have been developed, including Fused Deposition Modeling, Polyjet, Stereolithography, and Selective Laser Melting and Sintering.(20).
Utilizing polymer materials like PCL and PLA, which boost performance by overcoming each material's shortcomings, 3D printed bioresorbable stents are produced to treat heart-related disorders.(38).

Stereolithography produces models by layering a photosensitive epoxy resin layer on top of another layer.(2)(36). It is done by using digitally steered UV light on polymer liquid to harden the surface layer(4). The supports are manually removed in the aftermath and the complex structures and internal cavities are created by forming a transparent model(12). A temperature-controlled nozzle continuously extrudes molten filament as the foundation for fused deposition modeling (FDM).(36)(54). It is an extensively used approach that entails the use of thermoplastic filaments for 3D printing. According to Martin et al's study, its utility is greater in cardiovascular examination than in surgical planning(5) (50). It is a lower-resolution printing modality and produces a rough finish(8). The printer itself and the supplies are primarily inexpensive (15). For example, in the BQ Witbox, the layers are created by the adhesion and solidification of thin thermoplastic lines (36)(52). By employing a powerful laser beam to selectively melt metal or ceramic powder, robust components may be produced (4). However, it is more expensive than alternative procedures (21). Selective laser sintering (SLS) is a technique for joining layers of tiny particles of thermosensitive materials, including metal, ceramic, and nylon, using high-power infrared lasers. It is widely employed not just in cardiovascular applications but also in the manufacturing sector (19)(53). According to a new study, adding additive manufacturing to medical devices, instructional aids, procedural planning, and functional flow models can provide patients with cardiovascular disease with many benefits. Five key steps are involved in creating an artificial 3D heart: picture capture, segmentation, computer-aided design, fast prototyping, and clinical translation. (6). The CHD model for 3D printing is created with CT scans, STL files, and 3D printed models. 3D printed CHD models are highly effective for preoperative planning and simulation in large part due to their precision.(35)(51).
V. CURRENT CHALLENGES AND FUTURE DIRECTIONS
In the process of printing 3D physical models and medical images, the number of errors queued in each step increases the accuracy and reproductivity(30). The current uses of 3D printing models include the development of new devices, instructional materials, procedural planning, and functional flow models(69)(70).
During medical consultations, using 3D models to communicate with patients and doctors is highly helpful. Viewing their own 3D heart models has elicited pleasant reactions, even from those with congenital hearts. (7)(49). By combining the particle image velocimetry technology with printed models made of optically transparent materials, it is possible to directly visualize complicated flow dynamics. 3D printed models are helpful in a way that may extend cardiac tumors into valve structures or myocardial walls, allowing for their radical and full removal during preoperative and intraoperative surgical therapy of cardiac tumor expansions.(46)(48). Medical students, young doctors, and residents might benefit from 3D-printed physical models in their instruction. To be more specific, it enhances the relationship between doctors and patients, and cardiologists and heart surgeons acquire confidence in handling difficult cardiac-related situations.(38)(55). For doctors and other medical professionals who are less experienced in comprehending and interpreting cardiovascular inmates, 3D printing is even more trustworthy. Although juvenile patients may not be able to handle cardiac MRI's lengthy acquisition times and radiation-free benefit, the use of modern multi-detector cardiac CT scans and non-ECG gated acquisition allows for a reduction in radiation exposure.(7) (15).
Plans for surgical and percutaneous procedures can be made using patient-specific 3D printed models. According to case reports and small automobile series, 3D printed models help with decision-making in complicated circumstances and have also been successfully used for percutaneous operations (skin treatments).(7)(56). The left atrial appendage 3D printed models enhance procedure planning. The use of 3D printouts for procedure planning can enhance the training of new operators for device insertion.(27). Anatomic 3D printed models can be used to understand many cardiac diseases like congenital heart lesions (10). (22). Surgeons' first experience with the 3D printed models is very positive. They say that it reduces the complexity of the surgery(41)(57). The most popular use of 3D printing in the thoracic region is the direct fabrication of both permanent and bioresorbable implants. (8)(60).
Bioprinting has a wide range of applications. It was previously possible to maintain the construct shape during 3D bioprinting by using extrusion-based methods. 3D bioprinting now also includes inkjet printing and electrospinning, which do not require extraction. The use of 3D bioprinting for numerous cardiovascular applications has demonstrated its capacity to enable the vascularization of larger structures. With cardiovascular 3D printing, the ultimate goal is to replace damaged tissues with synthetic ones.(29)(68).
Within the framework of experimental settings for research applications, patient-specific 3D models can be created.(7)(59). Cardiac basic models of 3D printed anatomy offer a special way to investigate intricate hemodynamic function. A 3D printed model is used in several research methodologies to examine cardiac hemodynamics (13)(58).
The quality of the material was observed to be slightly different from that of the genuine cardiac tissue. However, 3D models printed with flexible materials have been utilized for rehearsing procedures, and the models were found to be beneficial. When displaying specimens, 3D printed models are more useful, which enhances learning about congenital cardiac anatomy and lowers the cost (23)(65). For surgical planning and training, a 3D-printed phantom of the mitral valve and left atrial appendage occlusion was employed (15)(67). These models create porous structures to preserve the viability of cells (34)(66).
Medical students, young doctors, and residents can benefit from the instruction provided by 3D printed physical models. To be more specific, it enhances the doctor-patient relationship and gives cardiologists and cardiac surgeons the confidence to handle difficult cardiac-related problems (38)(61). The use of these models in CHD instruction improves the students' learning (42)(63). Despite its early stages of development, several papers have already been published, explaining the advantages of this sector. (41)(62). Clinical treatment is simplified by 3D printing, and using these models might result in the creation of new tools and procedures (7)(64).
Conclusion
Higher temporal resolution, simplicity of use, and radiation avoidance are all benefits of 3D echocardiography. The 3D cardiovascular models provide a wide range of opportunities for modeling sophisticated structural catheterization operations that are patient-specific. Heart failure can have a wide Heart failure has a range of underlying reasons and is often treated with medical therapy prior to a successful heart transplant. Despite receiving the best medical treatment, patients with end-stage heart failure that is symptomatic may benefit from cardiac transplantation. Virtual imaging methods have an advantage over three-dimensional printing since they rely on human visual spatial abilities and three-dimensional mental conceptualization, which can differ greatly across people. The physical 3D printed models can only accurately portray dynamic heart activity during one portion of the cardiac cycle. Similar to how a coin has two faces, 3D printed models, which are detailed in this article, also have drawbacks. Heart valve modeling using 3D printing has limitations due to the absence of clinical valve validation and the hard printing of the valve location. There is still work to be done to speed up and lower the cost of creating 3D models utilizing 3D printing technology. There is still a significant barrier to printing the atrioventricular valve\\\'s anatomy. To address these issues, the ideal cardiac cycle phase is selected in order to optimize replication and produce novel printing materials. Research projects should primarily concentrate on these difficulties while also realizing the true potential of the 3D printing process, which may create an organ on a chip.
References
[1] El Sabbagh, A., Eleid, M. F., Al-Hijji, M., Anavekar, N. S., Holmes, D. R., Nkomo, V. T.,... Foley, T. A. (2018). The Various Applications of 3D Printing in Cardiovascular Diseases Current Cardiology Reports, 20(6), 1–9. https://doi.org/10.1007/s11886-018-0992-9 [2] Bartel, T., Rivard, A., Jimenez, A., Mestres, C. A., & Müller, S. (2018). Medical three-dimensional printing opens up new opportunities in cardiology and cardiac surgery. European Heart Journal, 39(15), 1246–1254. https://doi.org/10.1093/eurheartj/ehx016 [3] Giannopoulos, A. A., Mitsouras, D., Yoo, S. J., Liu, P. P., Chatzizis, Y. S., & Rybicki, F. J. (2016). Applications of 3D printing in cardiovascular diseases. Nature Reviews Cardiology, 13(12), 701–718. https://doi.org/10.1038/nrcardio.2016.170 [4] Vukicevic, M., Mosadegh, B., Min, J. K., and Little, S. H. (2017). Cardiac 3D Printing and its Future Directions. JACC: Cardiovascular Imaging, 10(2), 171–184. https://doi.org/10.1016/j.jcmg.2016.12.001 [5] Lindquist, E. M., Gosnell, J. M., Khan, S. K., Byl, J. L., Zhou, W., Jiang, J., & Vettukattil, J. J. (2021). 3D Printing in Cardiology: A Review of Applications and Roles for Advanced Cardiac Imaging. Annals of 3D Printed Medicine, 4 (100034). https://doi.org/10.1016/j.stlm.2021.100034 [6] Haleem, A., Javaid, M., & Saxena, A. (2018). Additive manufacturing applications in cardiology: A review. https://doi.org/10.1016/j.ehj.2018.09.008 [7] Milano, E. G., Capelli, C., Wray, J., Biffi, B., Layton, S., Lee, M., … Biglino, G. (2019). current and future applications of 3D printing in congenital cardiology and cardiac surgery. British Journal of Radiology, 92(1094). https://doi.org/10.1259/bjr.20180389 [8] Giannopoulos, A. A., Steigner, M. L., George, E., Barile, M., Hunsaker, A. R., Rybicki, F. J., & Mitsouras, D. (2016). Cardiothoracic applications of 3-dimensional printing Journal of Thoracic Imaging, 31(5), 253–272. https://doi.org/10.1097/RTI.0000000000000217 [9] Valverde, I. (2017). Three-dimensional Printed Cardiac Models: Applications in the Field of Medical Education, Cardiovascular Surgery, and Structural Heart Interventions. 70(4), 282-291 in Revista Espaola de Cardiologa (English Edition). https://doi.org/10.1016/j.rec.2017.01.012 [10] Odeh, M., Levin, D., Inziello, J., Lobo Fenoglietto, F., Mathur, M., Hermsen, J.,... Ripley, B. (2019). Methods for verifying the accuracy of 3D printed anatomic models using cardiac models as an example 3D Printing in Medicine, 5(1), 1–12. https://doi.org/10.1186/s41205-019-0043-1 [11] Qian, Z., Wang, K., Liu, S., Zhou, X., Rajagopal, V., Meduri, C., et al.,... Vannan, M. A. (2017). Quantitative Prediction of Paravalvular Leak in Transcatheter Aortic Valve Replacement Based on Tissue-Mimicking 3D Printing. JACC: Cardiovascular Imaging, 10(7), 719–731. https://doi.org/10.1016/j.jcmg.2017.04.005 [12] Wang, J., Coles-Black, J., Matalanis, G., & Chuen, J. (2018). Innovations in cardiac surgery: techniques and applications of 3D printing The Journal of 3D Printing in Medicine, 2(4), 179–186. https://doi.org/10.2217/3dp-2018-0013 [13] Ali, A., Ballard, D. H., Althobaity, W., Christensen, A., Geritano, M.,... Sheikh, A. (2020). Clinical situations for which 3D printing is considered an appropriate representation or extension of data contained in a medical imaging examination include: adult cardiac conditions. 3D Printing in Medicine, 6(1), 1–9. https://doi.org/10.1186/s41205-020-00078-1 [14] Borracci, R. A., Ferreira, L. M., Gallesio, J. M. A., Osvaldo, M., Núñez, T., David, M., … Eyheremendy, E. P. (2020). Three-dimensional virtual and printed models for planning adult cardiovascular surgery 1-10 in Acta Cardiologica. https://doi.org/10.1080/00015385.2020.1852754 [15] Gharleghi, R., Dessalles, C. A., Lal, R., McCraith, S., Sarathy, K., Jepson, N.,... Beier, S. (2021). 3D Printing for Cardiovascular Applications: From End-to-End Processes to Emerging Developments. Annals of Biomedical Engineering, 49(7), 1598–1618. https://doi.org/10.1007/s10439-021-02784-1 [16] Domínguez-Robles, J., Shen, T., Cornelius, V. A., Corduas, F., Mancuso, E., Donnelly, R. F., Larraeta, E. (2021). 3D printing enables the development of drug-loaded cardiovascular prostheses for thrombosis prevention. Materials Science and Engineering C, 129(June). https://doi.org/10.1016/j.msec.2021.112375 [17] Forte, M. N. V., Hussain, T., Roest, A., Gomez, G., Jongbloed, M., Simpson, J.,... Valverde, I. (2019). 3D printing applications in CHD Cardiology in the Young, 29(6), 733–743. https://doi.org/10.1017/S1047951119000398 [18] Wang, X., Liang, J., Mu, C., Zhang, W., Xue, C., He, Y.,... Li, D. (2022). Effects of 3D-Printed Hearts Used in Left Ventricular Outflow Tract Obstruction: A Multicenter Study, 1–13. Retrieved from http://europepmc.org/abstract/PPR/PPR440191%0A https://doi.org/10.21203/rs.3.rs-1206928/v1 [19] Wang, D. D., Qian, Z., Vukicevic, M., Engelhardt, S., Kheradvar, A., Zhang, C., … Vannan, M. A. (2021). 3D Printing, Computational Modeling, and Artificial Intelligence for Structural Heart Disease. Cardiovascular Imaging, 14 (1), pp. 41-60. https://doi.org/10.1016/j.jcmg.2019.12.022 [20] Lee, A. P., & Vida, V. L. (2021). Cardiovascular 3D printing. Cardiovascular 3D printing. https://doi.org/10.1007/978-981-15-6957-9 [21] Uccheddu, F., Carfagni, M., Governi, L., Furferi, R., Volpe, Y., & Nocerino, E. (2018). 3D printing of cardiac structures from medical images: an overview of methods and interactive tools International Journal on Interactive Design and Manufacturing, 12(2), 597–609. https://doi.org/10.1007/s12008-017-0415-y [22] Smerling, J., Marboe, C. C., Lefkowitch, J. H., Pavlicova, M., Bacha, E., Einstein, A. J., et al. Farooqi, K. M. (2019). Utilization of 3D Printed Cardiac Models for Medical Student Education in Congenital Heart Disease: Across a Spectrum of Disease Severity. Children\\\'s Cardiology, 40(6), 1258–1265. https://doi.org/10.1007/s00246-019-02146-8 [23] Ma, Y., Ding, P., Li, L., Liu, Y., Jin, P., Tang, J., & Yang, J. (2021). Three-dimensional printing for heart diseases: clinical application review. https://doi.org/10.1007/s42242-021-00125-8: Bio-Design and Manufacturing, 4(3), 675–687. https://doi.org/10.1007/s42242-021-00125-8 [24] Mowers, K. L., Fullerton, J. B., Hicks, D., Singh, G. K., Johnson, M. C., & Anwar, S. (2021). 3D Echocardiography Provides Highly Accurate 3D Printed Models of Congenital Heart Disease. Children\\\'s Cardiology, 42(1), 131–141. https://doi.org/10.1007/s00246-020-02462-4 [25] Mashari, A., Montealegre-Gallegos, M., Knio, Z., Yeh, L., Jeganathan, J., Matyal, R.,... Mahmood, F. (2016). Making three-dimensional echocardiography more tangible A workflow for three-dimensional printing with echocardiographic data. Echo Research and Practice, 3(4), R57–R64. https://doi.org/10.1530/ERP-16-0036 [26] Mashari, A., Montealegre-Gallegos, M., Knio, Z., Yeh, L., Jeganathan, J., Matyal, R.,... Mahmood, F. (2016). Making three-dimensional echocardiography more tangible A workflow for three-dimensional printing with echocardiographic data Echo Research and Practice, 3(4), R57–R64. https://doi.org/10.1530/ERP-16-0036 [27] Mashari, A., Montealegre-Gallegos, M., Knio, Z., Yeh, L., Jeganathan, J., Matyal, R.,... Mahmood, F. (2016). Making three-dimensional echocardiography more tangible A workflow for three-dimensional printing with echocardiographic data Echo Research and Practice, 3(4), R57–R64. https://doi.org/10.1530/ERP-16-0036 [28] Ameri, K., Samurkashian, R., & Yeghiazarians, Y. (2017). three-dimensional bioprinting Circulation, 135(14), 1281–1283. https://doi.org/10.1161/CIRCULATIONAHA.116.024945 [29] Sung, K., Patel, N. R., Ashammakhi, N., & Nguyen, K. L. (2021). 3-Dimensional Bioprinting of Cardiovascular Tissues: An Emerging Technology. https://doi.org/10.1016/j.jacbts.2020.12.006 [30] George, E., Liacouras, P., Rybicki, F. J., & Mitsouras, D. (2017). Measuring and establishing the accuracy and reproducibility of 3D printed medical models is challenging. Radiographics, 37(5), 1424–1450. https://doi.org/10.1148/rg.2017160165 [31] Lim, K. H. A., Loo, Z. Y., Goldie, S. J., Adams, J. W., & McMenamin, P. G. (2016). Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anatomical Sciences Education, 9(3), 213–221. https://doi.org/10.1002/ase.1573b [32] Jang, J., Yi, H. G., & Cho, D. W. (2016). Present and Future 3D Printed Tissue Models ACS Biomaterials Science and Engineering, 2(10), 1722–1731. https://doi.org/10.1021/acsbiomaterials.6b00129 [33] Qiu, K., Haghiashtiani, G., & McAlpine, M. C. (2018). 3D-Printed Organ Models for Surgical Applications Annual Review of Analytical Chemistry, 11(March), 287–306. https://doi.org/10.1146/annurev-anchem-061417-125935 [34] Mosadegh, B., Xiong, G., Dunham, S., & Min, J. K. (2015). current progress in 3D printing for cardiovascular tissue engineering. https://doi.org/10.1088/1748-6041/10/3/034002 [35] Lee, S., Squelch, A., & Sun, Z. (2021). Quantitative assessment of 3D printed model accuracy in delineating congenital heart disease. Biomolecules, 11(2), 1–11. https://doi.org/10.3390/biom11020270 [36] Gómez-Ciriza, G., Gómez-Ca, T., Rivas-González, J. A., Velasco Forte, M. N., and Valverde, I. (2021). Affordable Three-Dimensional Printed Heart Models. Frontiers in Cardiovascular Medicine, 8(June), 3–10. https://doi.org/10.3389/fcvm.2021.642011 [37] Ho, D., Squelch, A., & Sun, Z. (2017). Aortic aneurysm and aortic dissection through 3D printing. Journal of Medical Radiation Sciences, 64(1), 10–17. https://doi.org/10.1002/jmrs.212 [38] Sun, Z. (2020). Clinical applications of patient-specific 3D printed models in cardiovascular disease: current status and future directions. Biomolecules, 10(11), 1–34. https://doi.org/10.3390/biom10111577 [39] Mowers, K. L., Fullerton, J. B., Hicks, D., Singh, G. K., Johnson, M. C., & Anwar, S. (2021). 3D Echocardiography Provides Highly Accurate 3D Printed Models of Congenital Heart Disease. Children\\\'s Cardiology, 42(1), 131–141. https://doi.org/10.1007/s00246-020-02462-4 [40] Byl, J. L., Sholler, R., Gosnell, J. M., Samuel, B. P., & Vettukattil, J. J. (2020). Moving beyond two-dimensional screens to interactive three-dimensional visualization in congenital heart disease International Journal of Cardiovascular Imaging, 36(8), 1567–1573. https://doi.org/10.1007/s10554-020-01853-1 [41] Liddy, S., McQuade, C., Walsh, K. P., Loo, B., & Buckley, O. (2019). The Assessment of Cardiac Masses by Cardiac CT and CMR, Including Pre-op 3D Reconstruction and Planning. Current Cardiology Reports, 21(9). https://doi.org/10.1007/s11886-019-1196-7 [42] Smerling, J., Marboe, C. C., Lefkowitch, J. H., Pavlicova, M., Bacha, E., Einstein, A. J., et al. Farooqi, K. M. (2019). Utilization of 3D Printed Cardiac Models for Medical Student Education in Congenital Heart Disease: Across a Spectrum of Disease Severity. Children\\\'s Cardiology, 40(6), 1258–1265. https://doi.org/10.1007/s00246-019-02146-8 [43] Wang, H., Song, H., Yang, Y., Cao, Q., Hu, Y., Chen, J.,... Zhou, Q. (2020). Three-dimensional printing for cardiovascular diseases: From anatomical modeling to dynamic functionality. BioMedical Engineering Online, 19(1), 1–16. https://doi.org/10.1186/s12938-020-00822-y [44] Veerubhotla, K., Lee, Y., and Lee, C. H. (2021). Parametric Optimization of 3D Printed Hydrogel-Based Cardiovascular Stent. Pharmaceutical Research, 38(5), 885–900. https://doi.org/10.1007/s11095-021-03049-1 [45] Shin, J., & Truong, Q. A. (2018). Manufacturing Better Outcomes in Cardiovascular Intervention: 3D Printing in Clinical Practice Today. Current Treatment Options in Cardiovascular Medicine, 20(12), 1–13. https://doi.org/10.1007/s11936-018-0692-1 [46] Valverde, I., Gomez, G., Coserria, J. F., Suarez-Mejias, C., Uribe, S., Sotelo, J., … Gomez-Cia, T. (2015). 3D printed models for planning endovascular stenting in transverse aortic arch hypoplasia. https://doi.org/10.1002/ccd.25810 [47] Sousa, A. M., Amaro, A. M., & Piedade, A. P. (2022). 3D Printing of Polymeric Bioresorbable Stents: A Strategy to Improve Both Cellular Compatibility and Mechanical Properties. Polymers, 14(6). https://doi.org/10.3390/polym14061099 [48] Shivaprakash, Y. M., Gurumurthy, B. M., Siddhartha, M. A., Kumar, N. M. S., & Dutta, A. (n.d.). STUDIES ON MILD STEEL PARTICULATES REINFORCED DURALUMIN COMPOSITE FABRICATED THROUGH POWDER METALLURGY ROUTE. In www.tjprc.org SCOPUS Indexed Journal editor@tjprc.org. www.tjprc.org [49] Kurbet, R., Kumar M, S. N., & Addamani, R. (n.d.). A Review on Friction Stir Welding over other Welding Techniques of Aluminium Alloys. www.solidstatetechnology.us [50] Kumar M, S. N., & Bawge, G. (n.d.). Comparitive Study on Methods used to Improve the Corrosion Resistance Property of Aluminium Alloys-A Review. www.solidstatetechnology.us [51] N. M., S. K., Shashank, T. N., & Dhruthi. (2021). Review—Different Ceramic Reinforcements In Aluminium Metal Matrix Composites. ECS Journal of Solid State Science and Technology, 10(5), 053003. https://doi.org/10.1149/2162-8777/ac0114 [52] Siddesh Kumar, N. M., Shashank, T. N., Khan, N., Mahendra Babu, K. J., & Ajit Prasad, S. L. (2021). Modal and Harmonic Analysis of Spur Gear using FEA. Journal of Failure Analysis and Prevention, 21(5), 1855–1865. https://doi.org/10.1007/s11668-021-01243-2 [53] Siddesh Kumar, N. M., Sadashiva, M., & Monica, J. (2022). Speculative Testament of Corrosive Behaviour of Aluminium Composite Welded by FSW (pp. 429–440). https://doi.org/10.1007/978-981-16-4321-7_36 [54] Siddesh Kumar, N. M., Chethan, S., Nikhil, T., & Dhruthi. (2022). A review on friction stir processing over other surface modification processing techniques of magnesium alloys. In Functional Composites and Structures (Vol. 4, Issue 1). IOP Publishing Ltd. https://doi.org/10.1088/2631-6331/ac49f3 [55] Siddesh Kumar, N. M., Sadashiva, M., Monica, J., & Praveen Kumar, S. (2021). Investigation on Corrosion Behaviour of Hybrid Aluminium Metal Matrix Composite Welded by Friction Stir Welding. Materials Today: Proceedings, 52, 2339–2344. https://doi.org/10.1016/j.matpr.2022.01.362 [56] Sadashiva, M., Siddeshkumar, N. M., Monica, J., Srinivasa, M. R., Santhosh, N., & Praveenkumar, S. (2022). Hardness and Impact Strength Characteristics of Al based Hybrid Composite FSW Joints. International Journal of Vehicle Structures and Systems, 14(1), 13–17. https://doi.org/10.4273/ijvss.14.1.04 [57] Siddesh Kumar, N. M. (2022). Effect on wear property of aluminium metal matrix composite reinforced with different solid lubricants: a review. In International Journal of System Assurance Engineering and Management. Springer. https://doi.org/10.1007/s13198-022-01654-w [58] Kumar, N. M. S., Kerur, M. R. H., Khan, N., & Shashank, T. N. (2022). Vibration analysis of healthy and faulty gear of parallel shaft drive system. AIP Conference Proceedings, 2463. https://doi.org/10.1063/5.0080184 [59] Siddesh Kumar, N. M., Dhruthi, Pramod, G. K., Samrat, P., & Sadashiva, M. (2022). A Critical Review on Heat Treatment of Aluminium Alloys. Materials Today: Proceedings, 58, 71–79. https://doi.org/10.1016/j.matpr.2021.12.586 [60] Murthy, L. N. H. R., Kurbet, R., Kumar, S. N. M., Jashwanth, K., & Bhargav, P. (2022). Parametric Based Influence of Silicon Carbide Particulates on Tensile and Hardness Characteristics of Graphitic Aluminium Copper Alloy. AIP Conference Proceedings, 2648. https://doi.org/10.1063/5.0118021 [61] Kumar, N. M. S., Shashank, T. N., Dheeraj, N. U., Dhruthi, Kordijazi, A., Rohatgi, P. K., & Sadashiva, M. (2023). Coatings on Reinforcements in Aluminum Metal Matrix Composites. International Journal of Metalcasting, 17(2), 1049–1064. https://doi.org/10.1007/s40962-022-00831-8 [62] Shankar C, G. M., Shivaprakash, Y. M., Kumar M, S. N., A, S. M., Dutta, A., & Professor, A. (2019). EXPERIMENTAL INVESTIGATION ON SILICON CARBIDE REINFORCED DURALUMIN BASED MMC PRODUCED BY COLD COMPACTING. In www.tjprc.org SCOPUS Indexed Journal editor@tjprc.org. www.tjprc.org [63] G, R. H., Byregowda, H. v, & Kumar M, S. N. (n.d.). Optimization of ZnO Thin Films using Sol-Gel Dip Coating by Taguchi Method Section A-Research paper ISSN. In Eur. Chem. Bull. 2023 (Vol. 12, Issue 8). [64] G, R. H., Byregowda, H. v, & Kumar M, S. N. (n.d.). Optimization of ZnO Thin Films using Sol-Gel Dip Coating by Taguchi Method Section A-Research paper ISSN. In Eur. Chem. Bull. 2023 (Vol. 12, Issue 8). [65] G, R. H., Byregowda, H. v, & Kumar M, S. N. (n.d.). Optimization of ZnO Thin Films using Sol-Gel Dip Coating by Taguchi Method Section A-Research paper ISSN. In Eur. Chem. Bull. 2023 (Vol. 12, Issue 8). [66] S. M, M.Y. Sheikh, N. Khan, R. Kurbet, T.M.D. Gowda [67] M, S., Sheikh, M. Y., Khan, N., Kurbet, R., & Gowda, T. M. D. (2021). A Review on Application of Shape Memory Alloys. The International Journal of Recent Technology and Engineering (IJRTE), 9(6), 111–120. https://doi.org/10.35940/ijrte.F5438.039621 [68] Kiran Kumar N R, Dharmaraj H S, Sayeed Ahamed K I, Ramesh Kurbet, & Ajit Prasad S. (2020). Vibration and Noise Signal Analysis of Al-SiC MMC Gears. Research and Development in Machine Design, 3(2), 1–9. https://doi.org/10.5281/zenodo.4010469 [69] Kurbet, Ramesh; H. R., Ankitha; Holagi, Shraddha; Anvika; K. S., Veeresh; P., Pradyumna Bharadwaj, \\\"Applications of Robotic in Industry - A Review\\\", Journal of Mines, Metals & Fuels, Volume 71, Issue 6, 2023/6/1 [70] H. R. Lakshmi Narasimha Murthy, Ramesh Kurbet, N. M. Siddesh Kumar, K. Jashwanth, P. Bhargav; Parametric based influence of silicon carbide particulates on tensile and hardness characteristics of graphitic aluminium copper alloy. AIP Conf. Proc. 29 November 2022; 2648 (1): 030023. [71] Kurbet, R., Basavaraj, Amruth, C.M., Jayasimha, S.L.N. (2022). Effect of Ceramic Particles on AMMC Through Stir Casting Method—A Review. In: Bindhu, V., R. S. Tavares, J.M., ??lu, ?. (eds) Proceedings of Fourth International Conference on Inventive Material Science Applications. Advances in Sustainability Science and Technology. Springer, Singapore. https://doi.org/10.1007/978-981-16-4321-7_32 [72] T, G., Kalal, P., N, P., M K, A., H, G., Dharawadmath, S. I., C M, V., & V, N. (2023). Modern Smart Street Light Monitoring Systems. International Journal for Research in Applied Science and Engineering Technology, 11(9), 1075–1084. https://doi.org/10.22214/ijraset.2023.55782 [73] T, G., Kalal, P., N, P., M K, A., H, G., Dharawadmath, S. I., C M, V., & V, N. (2023). Modern Smart Street Light Monitoring Systems. International Journal for Research in Applied Science and Engineering Technology, 11(9), 1075–1084. https://doi.org/10.22214/ijraset.2023.55782
Copyright
Copyright © 2023 Pradumna Kalal. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET56203
Publish Date : 2023-10-18
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

