Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Role of Kidney and Circulatory System during Exercise: A Review Article
Authors: Kizito Praise-God D, Modestus Nwogu C, Nwokoleme Vincent, Ojih Jennifer Onyemowo
DOI Link: https://doi.org/10.22214/ijraset.2023.54943
Certificate: View Certificate
Abstract
The kidneys’ integrative responses to exercise helps in the cardiovascular control, thermoregulation, water and electrolyte regulation, The aim of this study is to review current literatures to understand how the kidney and the circulatory system respond to moderate and intensive exercise, literature search was carried out on Googlescholar with results limited to 5 year old studies and revisions. Studies regarding the effects of renal and cardiovascular responses to exercise were investigated. Outcomes regarding heart rate(HR), blood pressure(BP), Mean Arterial Pressure (MAP), Serum Creatinine (sCr) and Glomerular Filtration Rate (GFR) and the effects of each these outcome were analyzed, A total of 12 studies were considered, and groups were also stratified according to renal and cardiovascular responses to moderate and intense exercises. Findings suggest that there were moderate increase in heart rate, blood pressure except for subject with circulatory condition who had marked decrease in diastolic pressure to improve both systemic and central arterial stiffness. Also increase in kidney flow and glomerular filtration to compensate for different levels of hydration and dehydration, the review also highlights the lack of sufficient research work on kidney functions on different forms of exercise.
Introduction
I. INTRODUCTION
When challenged with any physical task, the human body responds through a series of integrated changes in function that involve most of its physiologic systems. Physical activities requires activation and control of the musculoskeletal system, the cardiovascular, renal and respiratory systems provide the ability to sustain this movement over extended periods. When the body engages in exercise training several times a week or more frequently, each of these physiologic systems undergoes specific adaptations that increase the body’s efficiency and capacity. The magnitude of these changes depends largely on the intensity and duration of the sessions, the force or load used in training, and how optimal these systems operate (Center for Disease Control and Prevention [CDC], 2023). The function of the kidneys in vertebrates is not limited to the plasma filtration process. Since the final result of renal function, urine, is practically water, electrolytes and waste substances, which implies that the kidney plays a major role in the regulation of body fluids. The kidney intervenes with great precision on the extracellular fluid both quantitatively and qualitatively. For this there are two possibilities. First, the kidney is able to concentrate or dilute urine through complex mechanisms. Secondly, the kidney is the “target organ” of hormonal systems that play a decisive role in the formation of a concentrated or diluted urine. (Montero, 2019). The kidneys’ integrative responses to exercise and heat stress aids thermoregulation, cardiovascular control, water, and electrolyte regulation. The kidneys are highly vascularized organs that receive approximately 20% of cardiac output at rest and are central to many homeostatic functions including the regulation of blood pressure, water, electrolytes, and acid/base balance (Christopheret al., 2021). There is a great interest in accurately quantifying changes in renal blood flow because it is a highly controlled variable that has implications for the regulation of blood pressure, water and electrolytes. Thus, it is also important to note that the kidneys have an intrinsic ability to maintain blood flow at varying arterial pressures i.e., auto regulation. Renal blood flow auto regulation is mediated by actions of the afferent arterioles and interlobular arteries and their myogenic response to constrict or relax in response to changes in perfusion pressure (Christopher et al., 2021) The cardiovascular system, responds predictably to the increased demands of exercise. With few exceptions, the cardiovascular response to exercise is directly proportional to the skeletal muscle oxygen demands for any given rate of work, and oxygen uptake increases linearly with increasing rates of work (Center for Disease Control and Prevention [CDC], 2023). To some extent or another, all the body’s organs are interdependent—the function of one organ relies to at least some degree on the ability of all the other organs to do their jobs. This interdependency is particularly striking between the heart and the kidneys. Heart and kidneys are two important organs in the body. They work together to keep us healthy. When one is affected, the other too is. In other words, the heart can affect the health of the kidneys, and the kidneys can affect the health of the heart. (Richard.N, 2022). The heart pumps blood filled with oxygen through all parts of the body, including the kidneys. The kidneys clean the blood, removing waste products and extra water. Without the kidneys, the blood would have too much waste and water.
Without the heart, the kidneys would not have the oxygen filled blood needed to do its many important jobs. Without the help of the kidneys, the heart would be working too hard or would not function at all. A healthy functioning cardiovascular system is important for the kidneys to do their job (National kidney foundation, 2023). There has been very little research on the role of kidney during exercise, generic keyword search on “role of kidney in exercise” didn’t yield the desired search result except for search words including “physiological response of kidney to exercise”. Kenney. (2015) stated reasons why this subject matter has not been studied extensively, the reasons to include that:
- The kidney is a “silent” organ during physical exercise that does not intervene in the supply of oxygen and obtaining energy. This may determine why most researchers do not see enough need to study the kidney function during exercise.
- The complexity of the study of renal function during exercise, which is limited to the analysis of urine and inferring renal function.
The aim of this write up is to review studies on the roles played by the kidney and the circulatory system during exercise. Using few research studies on renal response to exercise and also cardiovascular response to exercise.
II. METHODOLOGY
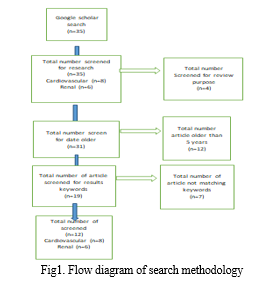
The study was carried out using research literatures search from Google scholar using the following keywords: Roles, function, response, adjustments, kidney, renal, circulatory, cardiovascular, and exercise. these keywords were identified after initial search on the “role of kidney and circulatory system on exercise” yielded non corresponding study titles, the selected keywords were used in separate search on circulatory and renal with combination of exercise, related title selections were limited only from page 1 to 6 of the Google scholar search results, producing 35 related articles of which 14 were of renal response and 21 were of cardiovascular response. 4 Review article were excluded leaving 31 research studies older than 5 years (<2019) were excluded leaving 19 papers, 6 renal response and 13 cardiovascular, a total of 12 related research were required for the review according to the issued guideline, for the selection, abstracts, results and conclusions of the materials were considered for the selection and keywords used in making the selection based on results were:
For Cardiovascular
- Heart rate (HR)
- Systolic Blood Pressure (SBP)
- Diastolic Blood Pressure (DBP)
- Mean Arterial Pressure (MAP)
For the Renal Response
a. Serum Creatinine (sCr)
b. Glomerular Filtration Rate (GFR)
A total of 8 research article on cardiovascular and 4 articles on renal response on exercise were used for the review (fig.1) illustrates the flow diagram of the process by which the articles were selected.
III. RESULT
A. Cardiovascular
|
S/N |
ARTICLE |
YEAR |
NO. OF SUBJECTS |
AGE |
M |
F |
BMI |
PC |
|
|
1 |
Beaumontet al. [2] |
2020 |
15 |
- |
9 |
6 |
35 ± 10 |
hypertension |
|
|
2 |
Ratchfordet al. [23] |
2020 |
25 |
53 ± 7 |
15 |
10 |
30 ± 6 |
- |
|
|
3 |
Ferreira et al. [7] |
2020 |
30 |
21 ± 0.4 |
- |
- |
24 ± 3.4 |
- |
|
|
4 |
De Oliveira et al[4] |
2020 |
15 |
57 ± 4 |
- |
- |
25 ± 3 |
Coronary artery disease |
|
|
5 |
Silva et al. [26] |
2019 |
23 |
21 ± 0.4 |
23 |
- |
- |
- |
|
|
6 |
Valentinoet al. [28] |
2022 |
9 |
61 ± 9 |
- |
- |
29.7 ± 4 |
- |
|
|
7 |
Huang, et al.[11] |
2023 |
11 |
21 ± 12 |
- |
- |
- |
- |
|
|
8 |
Shokri, et al.[27] |
2022 |
36 |
30 ± 10 |
17 |
19 |
- |
- |
|
|
The values included In the table are presented as M= Male; F= Female, BMI= Body Mass Index Physiological conditions = PC; Hypertension = HTN; Coronary Artery Disease = CAD; Moderate Exercise = ME Intensive Exercise =IE |
|
||||||||
Table 1
- Cardiovascular Responses Report: In the review of the cardiovascular response to exercise 8 [2, 23, 7, 4, 26, 28, 11, 27] studies were reviewed base on the evaluation considering (HR, SDP, DBP, BMI, CO, ) the articles were drawn based on publications made from 2019 to 2023, a total of 164 subjects were evaluated, with age range of 21 ± 0.4 to 61 ± 9, having 64 male[2, 23, 26, 27] and 35 females [2, 23, 27] respectively 65 subjects’ [7, 4, 26, 28,11,27] gender was unknown, 30 subjects [2, 4] were reported by 2 studies to present physiological conditions 15 [1]with HTN and 15 CAD [4], 5 studies [2, 23, 7, 4, 28,] recorded the BMI of their subjects ranging from 24 ± 3.4 to 35 ± 10 .all 8[2,23, 7, 4, 26, 28, 11, 27] studies were conducted for passive/ moderate exercise and 4[2, 23,7,26] for active/intensive exercise .
- Heart Rate: HR for ME was measured in 7 studies [2,23, 7, 4, 28, 11, 27], all evaluating HR from before exercise BHR and post exercise PHR the range of BHR 63 ± 6 to 133 ± 1 and PHR 67 ± 8 to 174 recorded in response to ME. HR for IE was evaluated by 3 [2, 23, 7] studies with BHR 119 ± 1 to 66.9 and PHR 129 ± 2 to 71 ± 2
- Blood Pressure: BP for ME was measured in 8 studies [2,23, 7, 4, 26, 28, 11, 27]the BP comprise of SDP and DBP, 8 studies evaluated for ME and 4 studies evaluated for IE.
- Diastolic Blood Pressure: Reporting for Moderate Exercise (ME) BDBP ranged from 61.1 ± 6 to 81 ± 4 and PDBP 69 ± 4 to 83± 9recorded in response to ME. BDBP for Intensive Exercise (IE) was evaluated by 4[1, 23, 26] studies with BDBP 62 ± 1 to 73 ± 13 and PDBP 145 ± 13 to 116 ± 2
- Systolic Blood Pressure: Reporting for ME,BSBP ranged from 117.3 ± 6 to 146 ± 4 and PSBP119 ± 3 to 160 ± 5 were recorded in response to ME. BSBP for IE was evaluated by 4 [2, 23, 7, 26] studies with BSBP116 ± 2 to 145 ± 13 and PSBP119 ± 2 to 171 ± 6
- Mean Arterial Pressure: MAP for ME was measured in 1 study [4], reporting for ME BMAP ranged from 91 ± 12 and PMAP89 ± 9 were recorded in response to ME. No study was carried on the IE.
- Cardiac Output: Co was evaluated in 2 studies [23, 4] for ME and 1 study[23]for IE Reporting for ME BCO ranged from 6.6. ± 0.3 to 7.4 ± 8 and PCO 119 ± 3 to 160 ± 5 were recorded in response to ME. BCO for IE was evaluated by 1 [23] study with BCO 6.6 ± 0.3 and PSBP 78 ± 0.4
Moderate Exercise
|
S/N |
ARTICLE |
BHR |
PHR |
BDBP |
PDBP |
BSBP |
PSBP |
BMAP |
PMAP |
BCO |
PCO |
|
|
1 |
Beaumontet al. [2] |
119 ± 17 |
121 ± 16 |
72(10) |
72(18) |
143 ± 15 |
139 ± 15 |
- |
- |
- |
- |
|
|
2 |
Ratchfordet al.[23] |
64± 2 |
67 ± 2 |
68 ± 3 |
74 ± 3 |
146 ± 4 |
160± 5 |
- |
- |
6.6 ± 0.3 |
7.2 ± 0.4 |
|
|
3 |
Ferreira et al. [7] |
67.9± 8.5 |
112.7(15.6) |
72.6(7.9) |
83( 99) |
116.6± 9 |
140± 9 |
- |
- |
- |
- |
|
|
4 |
De Oliveira et al[4] |
63± 6 |
67± 8 |
67± 8 |
69± 7 |
132± 19 |
125 ± 16 |
91± 12 |
89± 9 |
7.4± 8 |
6.8± 1.2 |
|
|
5
|
Silva et al. [26] |
- |
- |
61± 1 |
64± 2 |
117± 3 |
119± 2 |
- |
- |
- |
- |
|
|
6 |
Valentinoet al.[28] |
68± 1 |
174± 12 |
71± 10 |
78± 7 |
116±18 |
113± 17 |
- |
- |
- |
- |
|
|
7
|
Huang, et al.[11] |
133± 10 |
182± 14 |
76± 9 |
77 |
126± 10 |
130± 13 |
- |
- |
- |
- |
|
|
8 |
Shokri, et al.[27] |
88± 10 |
82± 9 |
81± 4 |
77± 2 |
121± 1 |
119± 3 |
- |
- |
- |
- |
|
|
The values included in the table are presented as Before exercise Heart Rate = BHR; Post Exercise Heart Rate = PHR; Before Exercise Diastolic Blood Pressure = BDBP; Post Exercise Diastolic Blood Pressure = PDBP; Before Exercise Systolic Blood Pressure = SDBP; = Post Exercise Systolic Blood Pressure = PDBP; Before Exercise Mean Arterial Pressure = BMAP; Post Exercise Mean Arterial Pressure = BMAP; Before Exercise Cardiac Output= BCO; Post Exercise Cardiac Output= PCO |
||||||||||||
Table 2.
Intense Exercise
|
S/N |
ARTICLE |
BHR |
PHR |
BDBP |
PDBP |
BSBP |
PSBP |
BMAP |
PMAP |
BCO |
PCO |
|
|
1 |
Beaumontet al. [2] |
119 ± 17 |
129 ± 20 |
73(13) |
70(20) |
145 ± 13 |
145 ± 14 |
- |
- |
- |
- |
|
|
2 |
Ratchfordet al. [23] |
64± 2 |
71 ± 2 |
68 ± 3 |
78 ± 3 |
146 ± 4 |
171± 6 |
- |
- |
6.6 ± 0.3 |
7.8 ± 0.4 |
|
|
3 |
Ferreira et al.[7] |
66.9± 8.5 |
123.5± 9.0 |
72.6± 7.9 |
83± 99 |
116.6± 9 |
148± 10 |
- |
- |
- |
- |
|
|
4 |
De Oliveira et al [4] |
- |
- |
- |
- |
- |
- |
- |
- |
- |
- |
|
|
5 |
Silva et al. [26] |
- |
- |
62± 1 |
65± 1 |
116± 2 |
119± 2 |
- |
- |
- |
- |
|
|
6 |
Valentinoet al. [28] |
- |
- |
- |
- |
- |
- |
- |
- |
- |
- |
|
|
7 |
Huang, et al.[11] |
- |
- |
- |
- |
- |
- |
- |
- |
- |
- |
|
|
8 |
Shokri, et al.[27] |
- |
- |
- |
- |
- |
- |
- |
- |
- |
- |
|
|
The values included in the table are presented as Before exercise Heart Rate = BHR; Post Exercise Heart Rate = PHR; Before Exercise Diastolic Blood Pressure = BDBP; Post Exercise Diastolic Blood Pressure = PDBP; Before Exercise Systolic Blood Pressure = SDBP; = Post Exercise Systolic Blood Pressure = PDBP; Before Exercise Mean Arterial Pressure = BMAP; Post Exercise Mean Arterial Pressure = BMAP; Before Exercise Cardiac Output= BCO; Post Exercise Cardiac Output= PCO |
|
|||||||||||
Table 3
Renal Response
|
S/N |
ARTICLE |
YEAR |
NO. OF SUBJECTS |
AGE |
M |
F |
BMI (kgm²) |
|
1 |
Hernandoet al.[10] |
2022 |
76 |
38 ± 39 |
62 |
14 |
22.73 ± 1.74 |
|
2 |
Pousselet al.[21] |
2020 |
54 |
24 ± 68 |
58 |
1 |
19.4 ± 26.5 |
|
3 |
Pryor et al.[22] |
2020 |
20 |
- |
20 |
- |
- |
|
4 |
Omassoli et al.[20] |
2019 |
20 |
25 ±3 |
20 |
- |
25 ± 26 |
|
The values included In the table are presented as M= Male; F= Female, BMI= Body Mass Index |
|||||||
Table 4
B. Renal Responses
In the review of the renal response to exercise 4 [10, 21, 22, 20] studies were reviewed base on the evaluation considering (sCr, and eGRF) the articles were drawn based on publications made from 2019 to 2022, a total of 170 subjects were evaluated, with age range of 25.3 ± 3 to 38 ± 39, with 1 study [22]not stating the age of its subjects parameter included 155 male[10, 21, 22, 20] and 15 females[10, 21], 3 studies [10, 21, 20] recorded the BMIof their subjects ranging from 19.26 ± 26.5 to 25 ± 26 .there was no focus on variation in exercise type sine most of the study were done on subjects partaking in marathon race which is an endurance exercise. There was no comprehensive report on the baseline evaluation from the studies.
- Serum Creatinine: sCr was evaluated in 4 studies [10, 19, 22, 20] for both Moderate Exercise(ME) and intensive(IE)Evaluation for ranged sCr was evaluated in 4 studies [10, 19, 22, 20] for ME and 3 study[10, 21, 20]for IE evaluating for ME sCr Ranged from [78 ±98] µmol?¹ to 85 [78 ±98] µmol?¹ 1[24]reported in value in percentage (0.94 ±0.09) %and for IE was evaluated by 4 [10, 19, 22, 20] studies with sCr 120 [102 ± 139]µmoll?¹ to 1.34[1.15 – 1.1] (mg/dl) 1 study [] reported in value in percentage (26.4 ± 12.4) %
- Estimated Glomerular Filtration (eGRF): eGRF was evaluated in 4 studies [10, 19, 22, 20] for ME and 3 study for IE evaluating for ME eGRFRangedfrom 31.4[24.3 ± 37.5] (ml/min/1.73m²) to 133 (ml/min/1.73m²) 1 [22] reported in value in percentage (30.2 ± 9.7) %and for IE was evaluated by 3[10, 21, 20] studies with eGRF 51.69[44.17-61.03](ml/min/1.73m²) to 135 (ml/min/1.73m²)eGRF 78 ± 0.4 1 [22] reported in value in percentage (26.4 ± 12.4) %
Moderate Exercise
|
S/N |
ARTICLE |
sCr |
eGRF |
|
1 |
Hernandoet al., [10] |
1.00 [0.88 – 1.10] (mg/dl) |
72.91 [66.24-99.25](ml/min/1.73m²) |
|
2 |
Pousselet al.,[21] |
12.1 (mg/l) |
133 (ml/min/1.73m²) |
|
3 |
Pryor et al.,[22] |
(0.94 ± 0.09 )% |
(30.2 ± 9.7)% |
|
4 |
Omassoli et al.,[20] |
85 [78 ± 98 ]µmol?¹ |
31.4[24.3 ± 37.5] (ml/min/1.73m²) |
|
The values included In the table are presented as Serum Creatinine = sCr; Estimated Glomerular Filtration Rate = eGFR |
|||
Table 5.
Intense Exercise
|
S/N |
ARTICLE |
(sCr) |
eGRF |
|
1 |
Hernandoet al.,[10] |
1.34 [1.15 – 1.1] (mg/dl) |
51.69 [44.17-61.03](ml/min/1.73m²) |
|
2 |
Pousselet al.,[21] |
13.7 (mg/l) |
135 (ml/min/1.73m²) |
|
3 |
Pryor et al., [22] |
(0.96 ± 0.11)% |
(26.4 ± 12.4)% |
|
4 |
Omassoli et al.,[20] |
120 [102 ± 139]µmoll?¹ |
- |
|
The values included In the table are presented as Serum Creatinine = sCr; Estimated Glomerular Filtration Rate = eGRF |
|||
Table 6,
C. Study Summaries
|
S/N |
Article |
Summary of finding |
|||
|
1 |
Beaumontet al., [2] |
Implied that there were some accountability for reduced myocardial work and superior efficiency during low-moderate - intensity exercise during left-lateral lift cycling ergometer, also that cardiovascular advantages were lost when exercising with left-lateral tilt SBPincreased to a greater extent from rest to exercise which suggested some sustained isometric work, HRresponse was variable in some individuals during the positioning despite a considerable lowering of power out. |
|||
|
2 |
Ratchfordet al., [23] |
Subjects with HTNhad higher DBPat rest HRincreased slightly in both with the onset of exercise, MAPwas ˜11mmhg higher at rest and ˜12mmhg higher during exercise, supporting the concept that the observed decrement in for arm blood flow and vascular conductance during exercise is most likely not due to chronotropic incompetence but due to impairment in the redistribution of blood flow from inactive tissue to the exercising muscles. |
|||
|
3 |
Ferreira et al., [7] |
Found increase in vascular response to resistance exercise protocols with different volumes and intensity and no differences were observed in cardiovascular overload, and that the increase response of cardiovascular parameters were promoted by the intensity of the exercise |
|||
|
4 |
De Oliveira et al., [4] |
Concluded that posture during isometric handgrip exercise influences the cardiovascular response with standing leading to higher cardiovascular stress, CAD promoted higher arterial pressure response however these responses were physiological and expected due to the presence of disease and type of exercise. The findings of this study conclude that standing position provides higher cardiovascular stress during isometric handgrip exercise. CAD promotes higher arterial pressure responses (systolic and mean arterial pressure) however these responses were physiological and expected due to the clinical dysfunctions provided by disease. Thus, low intensity isometric handgrip exercise can be prescribed in cardiac rehabilitation safely with cardiovascular monitoring, without performing Valsalva maneuver and considering the patient’s clinical condition and CAD stability. |
|||
|
5 |
Silva et al., [26] |
The pilot study analyzed BPacute responses and cardiac autonomic modulation after isometric handgrip exercise performed at different intensity. The result show that isometric handgrip exercise executed at 15% increased sympathetic modulation and reduced parasympathetic modulation after 20 minute of exercise there was 6mmhg for SBPand 4mmhg for DBPin hypertensive or non-hypertensive subjects. It was observed that there was reduced SBP in senior subjects 5 minutes after isometric handgrip exercise at 30% increased the difference explained at least in part by the BPassessment protocol suggesting that the hypotensive effect is fast which is perhaps only temporary and could return after 15 minutes, and shows that subjects with HBP levels are more responsive. |
|||
|
6 |
Valentinoet al., [28] |
The study observed increased cardiorespiratory stress and apical left ventricular rotation in response to both exercise programs, there were no conditional improvement in cardiac or endothelial function with training, results suggesting apical left ventricular rotation may indicate early cardiac adaptation to conditional improvement in cardiac or endothelial function with training, results suggesting apical left ventricular rotation may indicate early cardiac adaptation to exercise training in individual with CAD completing exercise based cardiac rehabilitation both TRAand HIITresult resulted in an increase in apical left ventricle in apical left ventricular rotation in response to exercise training, however, there is no evidence that either training program elicited any change in either clinical or additional measures of cardiovascular function in individuals with CAD |
|
||
|
7 |
Huang, et al., [11] |
The study showed PEevoked significant safe magnitude metabolic and cardiovascular responses, the stress may be greater in CPE, the response were not significant until 40% of the CPE duration, also illustrate that PEs require higher levels of neuromuscular activation to meet the increasing demand for muscle oxygenation and energy supply, proving consistency in previous reports that increase in HR and BP during small and large intensive exercise. |
|
||
|
8 |
Shokri, et al., [27] |
The study which was carried out for 4 weeks stating reduction in resisting HR was due to acceleration of development in parasympathetic nervous system activity regular aerobic exercise can affect the parasympathetic nerve thus increasing stroke volume and lowering RHR which has a positive effect on reducing cardiovascular diseases, the total changes in the reduction of SBP in the study was 4 weeks, the mechanism that caused the reduction after exercise are related to cardiac output reduction after exercise are related to cardiac output reduction which was controlled by 2 control systems, the exercise may reduce sympathetic activity in sedentary students the possible factor that caused no gender difference on DBP after 4 weeks of exercise of intensity was level of physical activity, since subject were sedentary students who lacked physical activity |
|
||
|
9 |
Hernandoet al.,[10] |
The study was carried on acute kidney failure and recovery after running marathon, one of the most physical demanding activity, helping to define the best strategy for recovering from renal injury, using renal function biomarkers (sCr) the depression of GFR seemed to be biphasic which could be influenced by the evolution of muscle biomarkers, the biomarkers are relevant to access kidney damage caused by high intensity physical activity. The biphasic depression of GFR observed in the study apart from being correlated with muscle damage level also could be related with the hydration status, the result of the study suggest that full resting is better strategy than using an elliptical machine and also show the beneficial impact of light intensity continuous running on marathon induced physiological damage recovery. |
|
||
|
10 |
Pousselet al.,[21] |
Sample of 24 included finishers depending on the methodology used to calculate GFR, the prevalence of AKI was observed from 0 to 12% urinary biomarkers of kidney damage were increased following the race but no significant decrease in the study showed a very low prevalence of AKI and no evidence that ultra-endurance running can cause important kidney damage in properly hydrated subjects |
|
||
|
11 |
Pryor et al., [22] |
The study on the impact of HA on changes in clinical biomarkers of AKI during high intensity exercise in hot environment, carried out, duration of 6 days which showed that HA was not protective against the reduction in kidney function when exercising in the heat the finding also support the notion that HA can mitigate decrement in renal function in individuals who work in hot environments e.g. military and athletes. Renal blood flow reduced in a hot environment compared to the cool environment. with further reduction during exercise in the heat GRF was preserved during light and moderate intensity work in cool environment with 15-19% reduction in GFR by up to 51%, increasing the risk of developing AKI |
|
||
|
12 |
Omassoli et al., 20] |
The research showed the potential benefits of adequate HA in preventing rise in (sCr consistent with AKI also showing an association between these excussion and neurohumeral inflammation and RPE makers which could have practical utility in surveillance for and prevention of AKI, results also showed that AKI prevented in unaclimatised volunteers performing standardized bouts of exercise /heat stress at baseline but is almost entirely absent after the first week of HA has been achieved as defined by sCr rise with later CKD |
|
||
|
The values included In the table are presented as Coronary Artery Disease = CAD; Heart Rate = HR; Diastolic Blood Pressure = DBP; Systolic Blood Pressure = SBP; Blood Pressure = BP; Hypertension= HTN; High Blood Pressure = HBP; Glomerular Filtration Rate = GFR ; Mean Arterial Pressure = MAP; Acute Kidney Injury = AKI; Heart Attack = HA ; Chronic Kidney Disorder = CKD; high-intensity interval training =HIIT ; s traditional exercise-based cardiac rehabilitation = TRAD ; Cardiac Plank Exercise = CPE; Plank Exercise = PEs |
|
||||
Table 7.
IV. DISCUSSION
During exercise and physical activity a large portion of cardiac output is delivered to the kidneys via the renal artery, which branches into a series of smaller arteries and arterioles and is ultimately filtered by the functional unit of the kidneys, the nephron. The control of renal blood flow and glomerular filtration rate (GFR) are important functions of the kidneys to regulate homeostatic processes that are stressed during intensive exercise, such as blood pressure, water, and electrolyte regulation. (Christopher et al., 2021). Most of the kidney studies were focused on exploring acute kidney failure and its recovery after running a marathon, one of the most physically demanding activities and the intensity of the recovery activity was defined and thus not selected by the individual him/herself so that all participants performed workouts at an equivalent relative intensity. From the data previewed it showed that there was considerable increase in renal function from moderate to intensive exercise these could be as a result of the roles the played by the kidney during physical activity which include as stated by Montero. (2019):
A. Restoration of the acid base state to the resting situation
The situation of metabolic acidosis triggered by the release of acids into the bloodstream during intense exercise must be compensated in an elementary manner with the replacement of the “spent base” as a result of the plasma buffer. The restitution of spent bicarbonate determines the elimination of acids by urine. This elimination is done in a controlled manner by the kidney, mainly through the elimination of an acid, the ammonium ion (NH4 +).
B. Maintenance of Hydro-Electrolytic Balance
Since there is loss of water and electrolytes by the mechanism of heat removal, sweating reduction of urine volume (oliguria), preserves it from a loss of fluid that would lead to dehydration in a short time, due to loss of water and electrolytes due to sweating
C. Renal flow Redirection
During exercise of increasing intensity, the renal circulation is one of the circulatory zones where there is a restriction of the blood flow, allowing a derivation of the renal flow towards the active territories. This results in decrease in renal blood flow(RBF), renal plasma flow (RPF), glomerular filtration rate (GFR) and filtration fraction (FF). This reduction is an “intelligent” response to the mechanisms of cardiac output regulation. Indeed, not only is the increase in cardiac output is sufficient to supply the muscles during the exercise of increasing intensity. Redistribution of the largest volume of blood expelled in one minute is necessary.
D. Increase in Oliguria
The most important form of heat removal in human is sweating or equivalent forms of water loss by evaporation. The loss of water through sweating can reach 70% of the losses. Thus, during an exercise such as the ultra-marathon the kidney can produce oliguria (low urine output) of about 15 to 50%, although there may even be an increase in diuresis, due to multiple causes such as intensity, previous hydration, temperature, etc.
Stress oliguria necessarily suggests an increase in the reabsorption of water and osmotically active electrolytes
Findings also showed increase in cardiovascular variables. The behavior of all cardiovascular variables reviewed showed significant increases with a large effect in relation to the rest condition (before exercise), similar to that observed in other studies except for subject with physiological conditions,where the possible mechanism for reduction of resultant heart rate was due to acceleration of development in the parasympathetic nervous system activity. Regular aerobic exercise can affect the parasympathetic nerve, thus increasing stroke volume and lowering the resultant heart rate RHR which has a positive effect on the reduction cardiovascular disease
Next, elevated heart rate associated with increased mechanical stress, which eventually increased the stiffening of the arterial wall. The increased arterial wall may increase pulse, blood flow and shear stress resulting reduced resultant heart rate. Reduction in resultant heart rate occurs when the stroke volume with prolonged diastole raises the shear stress (Shokri, et al., 2022).
Isea et al.,1994 explained that where the diastolic pressure decreases for subject with circulatory conditions, that eventhough there is tachycardia (which would be normally expected to produce a higher diastolic pressure), mainly because of the drop in the peripheral vascular resistance, mean arterial pressure is generally much higher in these patients, likely owing to a lesser reduction in total peripheral resistance. For the first 2 to 3 hours following exercise, blood pressure drops below pre-exercise resting levels, a phenomenon referred to as post-exercise hypotension.
A possible explanation to this increase could be the compression of blood vessels by the muscles involved in the exercise (MacDougall, et al.,1985). Activation of both chemoreceptors and muscle and joint mechanoreceptors promote the increased sympathetic and decreased parasympathetic cardiovascular modulation (Ichinose, Watanabe, Fujii, Kondo, & Nishiyasu, 2013).
Other researchers have also given possible reasons for increase in circulatory activity during exercise for example
E. Blood Flow pattern
Rowell 1986 explained that the pattern of bloodflow changes dramatically when a person goes from resting to exercising. At rest, the skin and skeletal muscles receive about 20 percent of the cardiac output. During exercise, more blood is sent to the active skeletal muscles, and, as body temperature increases, more blood is sent to the skin. This process is accomplished both by the increase in cardiac output and by the redistribution of blood flow away from areas of low demand. This process allows about 80 percent of the cardiac output to go to active skeletal muscles and skin at maximal rates of work.
With exercise of longer duration, particularly in a hot and humid environment, progressively more of the cardiac output will be redistributed to the skin to counter the increasing body temperature, thus limiting both the amount going to skeletal muscle and the exercise endurance (Rowell 1986).
Apart from the noticeable increase in myocardial blood flow, one can see that skin blood flow is also increased. This is not normally expected from a sympathetically mediated redistribution of blood flow, i.e. usually skin is viewed as a non-essential tissue. However, in the context of exercise, blood flow to the skin increases in order to improve the removal of metabolic heat. Only when the limits of endurance are reached does skin blood flow begin to diminish again, probably as a measure to reserve every last drop of blood for the muscle fibers. (Deranged physiology, 2023).
F. Regional Muscle Vasodilation
Increased muscle activity results in increased oxygen demand, this increased demand is met by increasing blood flow to exercising muscle the increase in blood flow is mediated mainly by a regional decrease in vascular resistance
Other organ systems which are not essential to exercise end up being sacrificed for the greater good; their blood flow diminished significantly as the autonomic nervous system redirects all power (blood) to the active engines (muscles) (Deranged physiology, 2023).
G. Increase in Cardiac output Associated with Exercise
Cardiac output thus plays an important role in meeting the oxygen demands for work. As the rate of work increases, the cardiac output increases in a nearly linear manner to meet the increasing oxygen demand, but only up to the point where it reaches its maximal capacity (Scruggs et al., 1991). The differences in individuals is the amount of oxygen delivery their cardiovascular systems can sustain. To supply active muscle, athletic individuals can expect their cardiac output to increase up to 30L/min or so, compared to non-athletics (Deranged physiology, 2023). Cardiac output can increase massively during exercise, up to 30L/min the increase in cardiac output is due to both an increase in heart rate and in stroke volume with increasing workload, the heart rate continues to increase but stroke volume decreases because of diminishing diastolic time.
H. Mean Arterial Blood Pressure
Increases in response to dynamic exercise, largely owing to an increase in systolic blood pressure, because diastolic blood pressure remains at near-resting levels. Systolic blood pressure increases linearly with increasing rates of work, reaching peak values of between 200 and 240 millimeters of mercury in normotensive persons. Because mean arterial pressure is equal to cardiac output by the total peripheral resistance, the observed increase in mean arterial pressure results from an increase in cardiac output that outweighs a concomitant decrease in total peripheral resistance. This increase in mean arterial pressure is a normal and desirable response, Hypertensive patients typically reach much higher systolic blood pressures for a given rate of work, and they can also experience increases in diastolic blood pressure.
I. Coronary Circulation
The coronary arteries supply the myocardium with blood and nutrients. During vigorous exercise, all three major determinants of myocardial oxygen requirements increase above their resting levels. The increase in coronary blood flow during exercise results from an increase in perfusion pressure of the coronary artery and from coronary vasodilation. Most important, an increase in sympathetic nervous system stimulation leads to an increase in circulating catecholamine. This response triggers metabolic processes that increase both perfusion pressure of the coronary artery and coronary vasodilation to meet the increased need for blood flow required by the increase in myocardial oxygen use ventilation rates can reach more than 200 liters per minute at maximal rates of work.
Conclusion
The present review highlights current evidence regarding the role played by the kidney and the circulatory system on exercise. Findings suggest that there are moderateincrease in heart rate,blood pressure except for subject with circulatory condition who had marked decrease in diastolic pressure to improve both systemic and central arterial stiffness. Also increase kidney flow and glomerular filtration to compensate for different levels of hydration and dehydration the review also highlights the lack of sufficient research work on kidney functions during different forms of exercise.
References
[1] M. Agarwal, S. Singh, J. Narayan, S. Pandey, S. Tiwari and P. Sharma \"Cardiovascular Response and Serum Interleukin-6 Level in Concentric Vs. Eccentric Exercise\", Journal of clinical and diagnostic research: JCDR, 11(4), 2017, CC04-CC08. [2] A.J, Beaumont, L.J, Forrest, V., Unnithan and N, Sculthorpe \"Cardiovascular responses during submaximal cycling with and without left-lateral tilting: insights for practical applications of stress echocardiography\". Applied Physiology, Nutrition, and Metabolism, 46(2), 2021, 178-181. [3] CDC (2023) center for disease control and prevention: chapter 3 physical activity and health, a Report of the surgeon generalhttps://www.cdc.gov/ncc/dphp/sgr/intro3. [4] M. De Oliveira Gois, R.P., Simões, A., Porta, V.C., Kunz, C.M., Pastr and A.M., Catai \"Cardiovascular responses to low-intensity isometric handgrip exercise in coronary artery disease: effects of posture\". Brazilian journal of physical therapy, 24(5), 2020, 449-457. [5] Deranged physiology (2023) cardiovascular response to exercisehttps://www.derangedphysiology.com/main/CICM-primary-exam/required-reading/cardiovascular-system/chapter504/cardiovascular-response-exercise [6] Experience life junarary 17 2017 pumped up how exercise affects circulation (and vice versa)Htttps:// www.experiencelife.com/how-exercise-affect-circulation-&-vice-versa [7] L.P., Ferreir, O.C., Moreira, R.L., dos Reis Caldas, L.M.T., de Rezende, K., Hughes, E., Souza and M.A., Carneiro-Júnior. \"Cardiovascular responses of beginner and advanced practitioners to different volume and intensity resistance exercise protocols\". European Journal of Human Movement, 44, 2020, 80-94. [8] Glanville .N (November, 20, 2022) what is exerciseWeightloss resouces co.uk https://www.weightlossresources.co.uk/exercise/questions-answer/what-is-exercise.html [9] Havard Health Publishing (June, 12 2019) Harvard medical schoolhttps://www.harvardandhealthpublishing/exercise-and-year-artery-harvard-health [10] C., Hernando, C., Hernando, N., Panizo, E., Collado-Boira, A., Folch-Ayora, Martínez- I., Navarro, and B., Hernando. \"Renal function recovery strategies following marathon in amateur runners\". Frontiers in Physiology, 192, 2020 [11] Z., Huang, B.,Wang, K., Song, S., Wu, H., Kong, L., Guo, and Q., Liang. \"Metabolic and cardiovascular responses to continuous and intermittent plank exercises\". BMC Sports Science, Medicine and Rehabilitation, 15(1), 2023,1. [12] J,E., Isea, M., Piepoli, Adamopoulosis, G., pannarcle, P., Sleight and A., Coat. \"Time course ofhaemodynamics changes after maximal exercise\". European journal of clinical, 24, 2004, 824-829 [13] W.L., Kenney, J., Wilmore, D., Costill. \"Physiology of sport and exercise 6th edition. Human kinetics\". 2015; 648. Ref.: https://goo.gl/fUKyPp [14] Kidney physiology and heart physiology during heat stress and modification by exercise, dehydration, heat acclimatization, aging and temperature 8 : 2 108 – 159 DOI : 100/080/23328940.2020.182684 [15] J.D., MacDougall, D., Tuxen, D.G., Sale, J.R., Moroz and J.R., Sutton. \"Arterial blood pressure response to heavy resistance exercise\". J Appl Physiol, 58(3), 1985, 785-790. [16] W.D., McArdl, F.I., Katch, and V.L., Katch. \"Exercise physiology: nutrition, energy, and human performance\". Lippincott Williams & Wilkins. 2010; Ref.: https://goo.gl/Yrcw8P [17] J.C., Montero. \" Renal function during exercise and recovery\". Journal Sport med . 2019: 4: 008-015 DOI: 10.29328/journal.jsmt.1001037 [18] National kidney foundation, 2023 the heart and kidney connection. www.kidney.org/atol/content/heart-and-kidney-connection [19] J., Omassoli, E,A., Hill, D.R., Woods, S.K., Delves, J.L., Fallowfield, S.J., Brett, M.J., Stacey. \"Variation in renal responses to exercise in the heat with progressive acclimatisation\". Journal of Science and Medicine in Sport, 22(9), 2019, 1004-1009. [20] M., Poussel, C., Touzé, E., Allado, L., Frimat, O., Hily, N., Thilly, and B., Chenuel. Ultramarathon and renal function: does exercise-induced acute kidney injury really exist in common conditions?. Frontiers in Sports and Active Living, 71. 2020 [21] R.R., Pryor, J.L., Pryor, L,W., Vandermark, E.L., Adams, R.M., Brodeur, Z.J., Schlader and D.J., Casa. \"Acute kidney injury biomarker responses to short-term heat acclimation\". International journal of environmental research and public health, 17(4) 2020, 1325. [22] S.M., Ratchford, H.L., Clifton, D.T., La Salle, R.M., Broxterman, J.F., Lee, J.J., Ryan, and D.W., Wray. \" Cardiovascular responses to rhythmic handgrip exercise in heart failure with preserved ejection fraction\". Journal of Applied Physiology, 129(6), 2020, 1267-1276. [23] N.F., Richard (may 16 2022) very well health examining the link between the heart andkidney Disease Https://www.verywellhealth.com/examinig-the-link-between-heart-&-kidney-disease [24] B., Scruggs, N.B., Martin, C.E., Broeder, Z., Hofman, E.L., Thomas, K.C., Wambsgens et. al. \"Stroke volume during submaximal exercise in endurance-trained, non-intensive subjects with beta blockade (propranolol and pindolol)\". American Journal of cardiology , 67: 2020, 416-421 [25] I.M.D., Silva, M.F., Leonardo, R.M., Ritti-Dias, B.P.V.P., Sobral, Pirauá, A. L. T., Oliveira, L. M. F. T. D., and B.Q., Farah. \"Cardiovascular responses after isometric handgrip exercise at different intensities in healthy men\". Journal of Physical Education, 30, 2019 [26] I.S.M., Shokri, N.S.M., Suhaimi, N.F., Illias, R., Adnan and H., Ismail. The effect of cardiovascular responses on aerobic exercise and relationship between pulmonary function and body composition among sedentary students. Journal of Physical Education & Sport, 22(9) 2022. [27] S.E., Valentino, E.C., Dunford, J., Dubberley, E.M., Lonn, M.J., Gibala, S.M., Phillips and M.J., MacDonald. Cardiovascular responses to high?intensity stair climbing in individuals with coronary artery disease. Physiological Reports, 10(10), 2020 e15308. [28] Wikipedia (2023) circulatory system Wikipedia foundationLast modified February 19 2023, 9:50
Copyright
Copyright © 2023 Kizito Praise-God D, Modestus Nwogu C, Nwokoleme Vincent, Ojih Jennifer Onyemowo. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET54943
Publish Date : 2023-07-23
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

