Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Study of Measles Incidence and its Eradication: A Review
Authors: Mr. Sumedh Narayan Sonkamble, Mr. Prajwal Balaji Phad, Ms. Pooja Prashant Kharosekar, Ms. Pooja Murari Kotmale, Ms. Pranita Waghambar Waghmare, Mr. Pradip Uddhav Waghmare, Mr. Prashant Machhindra Waghmare
DOI Link: https://doi.org/10.22214/ijraset.2023.56085
Certificate: View Certificate
Abstract
Despite a decrease in global incidence, measles outbreaks continue to occur in developed countries as a result of subopti-mal vaccine coverage. Currently, an important mode of measles transmission appears to be nosocomial, especially in coun-tries where measles is largely under control. We therefore conducted a review of the literature by searching PubMed for the term \"measles\" plus either \"nosocomial\" or \"hospital acquired\" between 1997 (the date of the last review in the field) and 2011. The reports indicate that measles is being transmitted from patients to health care workers (HCWs) and from HCWs to patients and colleagues. Here, we explain how outbreaks of measles occurring in healthcare settings differ in some ways from cases of community transmission. We also highlight the need for all HCWs to be immunized against measles.
Introduction
I. INTRODUCTION
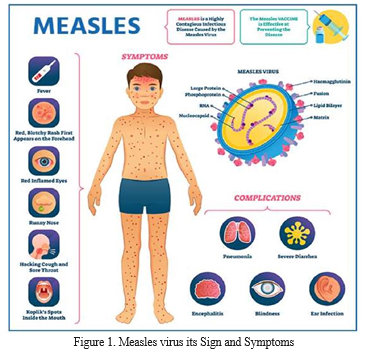
Measles virus (MV) belongs to the genus Morbillivirus of the family Paramyxoviridae. It is an enveloped, non-segmented, single-stranded, negative-sense RNA virus, and its genome encodes at least six structural proteins. MV (also known as rubeola virus) causes measles, an acute highly contagious infection usually seen in children. Recovery from measles is the rule but severe complications may develop in some cases. Measles (Rubeola) is an RNA virus infectious disease mainly seen in children. Despite the availability of an effective vaccine against measles, it remains a health issue in children. Although it is a self-limiting disease, it becomes severe in undernourished and immune-compromised individuals. Measles infection is associated with secondary infections by opportunistic bacteria due to the immunosuppressive effects of the measles virus. Recent reports highlight that measles infection erases the already existing immune memory of various pathogens. This review covers the incidence, pathogenesis, measles variants, clinical presentations, secondary infections, elimination of measles virus on a global scale, and especially the immune responses related to measles infection. Before the development and introduction of the measles vaccine in the 1960s, it was the leading cause of child mortality and morbidity globally.
Before introducing the measles vaccine, measles alone caused more than 2 million childhood deaths. The inclusion of the measles vaccine in routine immunisation programs and government-sponsored awareness programs has resulted in a drastic decline in measles-related morbidity and mortality.
Despite the efforts made by the government and the widespread immunisation programs, measles results in more than 100,000 deaths annually . This review highlights the incidence and epidemiology of measles, the viral pathophysiology, prevention, diagnosis, and management, progress made in the virology of this disease, measles elimination, eradication challenges, and the immunological aspects of measles infection.
Pathophysiology
The measles virus is transmitted through respiratory droplets or aerosol particles. The initial site of infection is the respiratory tract, where they infect the macrophages in the lung alveoli, lymphocytes, and dendritic cells .
The virus proliferates during the incubation period and migrates to the lymphoid tissues, and then gets spread to the bloodstream by the infected lymphocytes, endothelial cells, and epithelial cells . Wild-type measles vectors are known to infect cells by using the nectin-4 receptors and signalling lymphocytic activation molecule 1 (SLAMF1, also known as CD150).
The viral strains are also known for their affinity towards the CD46 receptor molecule expressed in human cell membranes. The measles virus can enter through a pH-independent pathway initiated by endocytosis and facilitated by SLAMF1 in B-lymphoblastoid cells. In addition, the virus was shown to enter breast and cancer cells (MCF7) through the micropinocytosis pathway mediated by the nectin-4 receptors. Nectin-4 receptors that are present on the surface of the epithelial cells in the respiratory tract help the virus transmission from the infected dendritic cells to the epithelial cells of the respiratory tract. The measles virus is transmitted to the susceptible hosts either through budding from the surface of epithelial cells of the respiratory tract or through the damaged epithelial cells. The measles infection starts before the appearance of a rash, which is typical of a measles infection, and lasts for several days after the appearance of the rash. The viral RNA can be detected for at least 3 months in clinical samples after the appearance of the rash. Measles infection is traditionally believed to be an acute infection that lasts for 2–3 weeks. Still, recent studies on the macaque model reported the presence of viral RNA in the peripheral mononuclear cells for 67 days. According to this study, the measles viral RNA remains detectable in the lymphoid tissues even after blood samples disappear.
Clinical Variants of Measles
There are two clinical variants of measles infection: modified measles and atypical measles.
Modified Measles
Modified measles is a milder form of measles that is reported in patients with a history of either wild-type measles infection or vaccination. Modified measles have a longer incubation period, ranging from 17 to 21 days [Modified measles is not highly contagious . Several causes for the inefficient/non-protective immunity for the measles virus result in modified measles. Transplacental acquisition of measles-specific antibodies from mother to infant is one of the reasons for modified measles in infants. The measles-specific antibodies acquired from infected mothers are generally cleared from the bloodstream of infants by 3–9 months of infancy . When the antibody titres reach sub-optimal levels for protection against measles, infants become susceptible to measles infection. Still, the disease is milder due to low levels of protective antibodies. Other causes of modified measles are intravenous antibodies, measles vaccination resulting in lower antibodies than required for measles protection, and a prior history .
Atypical Measles
Atypical measles is now rare in individuals vaccinated with the inactivated measles virus. This form of measles vaccine was used back in 1963 and 1967 in the United States. The inactivated virus vaccine could not produce protective levels of measles-specific antibodies . Symptoms like headache and fever appear within 7 to 14 days of exposure to inactivated measles virus vaccine . Unlike the typical measles infection, atypical measles is associated with the appearance of the rash first in the extremities and then extends to the trunk . Atypical measles results in severe infection, but it is not contagious .
Immunological Aspects of Measles Infection and Host Immunity The measles virus is known to infect different cell types. However, most of the studies that were performed on the virus were performed on tumor cell lines in vitro. A few studies were performed on IFNAR knockout mice and Rhesus monkeys . These in vitro and in vivo studies have allowed us to understand the immunological aspects of the disease and the host’s immune responses to it.
Innate Immunity Response to Measles Infection
The measles virus spreads through its mobility, starting from the site of infection to the respiratory tract, lymphoid organs, and then back to the respiratory tract. It first infects CD150-expressing cells, namely, the dendritic cells (D.C.s) and macrophages (M.P) (Lemon et al., 2011). D.C.s play a central role in developing an immunological response to pathogens by presenting antigens on major histocompatibility complex molecules (MHC), T-cell activation due to costimulation of CD80, and CD86, which ultimately leads to the release of proinflammatory cytokines IL-12 and IL-18. The production of IL-12 by D.C.s is important for the optimal activation of CD4+ and CD8+ T cells. The activation of the CD4+ and CD8+ cells is initiated by interferongamma (IFN). This is crucial as it activates the innate immune response to infection and reactivates during the pathogen reencounter .
Diagnosis
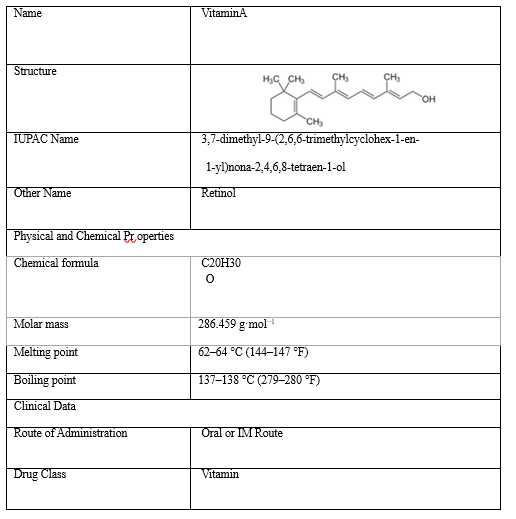
Measles is easily identified by clinical features, such as fever and rashes, especially during outbreaks or in patients travelling from measlesendemic areas. Some other viral infections, such as those caused by the rubella virus, human herpesvirus type 6, parvovirus B19, and dengue viruses, show similar clinical features . While diagnosing a suspected measles patient, clinicians should consider the typical clinical features of measles infection and look for the secondary problems due to measles infection, such as pneumonia, conjunctivitis, otitis media, and diarrhoea. Since malnutrition, especially vitamin A deficiency, immune deficiency (HIV infection), and immunosuppression (individuals undergoing organ transplantation), are major contributors to measles-associated mortality, a thorough clinical examination and a detailed history of patients should be taken. Patients with these risk factors are at a higher risk of mortality. Prompt action by clinicians is warranted in patients with vitamin deficiency, which involves administering vitamin A supplements to these patients.
The hospital administration should take appropriate action to isolate the measles-infected cases to prevent the transmission of the measles virus to healthy individuals It is challenging to clinically diagnose measles infection before the appearance of the rash and in immunocompromised children who might not have the rash. The most widely employed laboratory test detects IgM specific for measles virus antigens by ELISA. The levels of measles-virusspecific IgM are very low or undetectable till 4 days after a rash appears. Therefore, tests within 4 days of rash development give false-negative results Almost all the measles-infected individuals show detectable levels of measles virus-specific IgM after 4 days of rash appearance, and 75% of measles-virus-infected individuals show detectable levels of measles-virusspecific IgM within the first 3 days of rash appearance. IgM levels specific to the measles virus are highest during 1–3 weeks post rash onset and decline to undetectable levels within 4–8 weeks post rash onset Although the commercially available ELISA kits detect antibodies for the measles virus, the standard gold method for diagnosing measles infection is the highly sensitive plaque reduction neutralisation assay Studies showed that individuals who tested seronegative for measles using ELISA were positive for seroconversion when using the plaque reduction neutralisation assay. Therefore, the individuals who test negative with ELISA should be advised for plaque reduction neutralisation assay. DNA-based methods, such as real-time PCR (RT-PCR), are used to confirm a measles virus infection. RT-PCR detects the viral RNA in clinical samples of the suspected individuals even before the measles-specific antibodies reach detectable levels. Different specimens are used to detect measles-specific antibodies and viral RNA, such as oral fluids and serum extracted from dried blood spots. Although oral fluid samples are appropriate for large-scale survey purposes, this method has a low sensitivity
II. AIM AND OBJECTIVE
A. Aim
The main aim to study the Measles Virus is to identify changes in the virus and its eradication from the society.
B. Objectives
- To study the viral disease Measles and its eitiology.
- To find causes of virus, prevention, treatment of Measles.
- To study advances in the vaccinations of Measles.
- To study the eradication methods to decrease the viral spread of disease among small children.
- To study the management of Measles.
III. DETAILED PROJECT REPORT
Measles is a self-limiting acute contagious viral infection. It is characterised by a typical rash, high fever (up to 104°F), cough, coryza, and conjunctivitis. Characteristic white lesions called Koplik’s spots form in the buccal mucosa even 1–2 days before the appearance of the rash; therefore, Koplik’s spots can indicate measles infection, even before the appearance of the rash. A flat red rash appears first on the face and the neck and subsequently advances to the trunk and the extremities in solid and discrete spots within 3–4 days after the onset of fever. Children with previous immunisation history present minimal rash and sometimes do not show the typical characteristics of measles infection, i.e., cough, coryza, and conjunctivitis. Malnourished children present with a prominent, deeply pigmented rash. As a rash is a result of innate/cellmediated immunity, in conditions of compromised cellular immunity, e.g., HIV, a measles infection may not develop a rash, or the appearance of the rash may be delayed. Generally, in uncomplicated cases of measles infection, the recovery takes place within 1 week of rash appearance. Several factors complicate measles infection, affecting most organs. The factors contributing to the complication of measles are young age (infants), age older than 20 years, pregnancy, malnourishment, vitamin A deficiency, and immunocompromised conditions.
Management Measles is a self-limiting viral infection. The management regime involves therapies to control/manage the associated risk factors and complications, such as dehydration, malnutrition, or nutritional deficiencies. The management of measles depends on prompt diagnosis, treatment of bacterial and viral infections secondary to measles infection, and vitamin A supplementation. The United States of America was the first country in the world to abolish endemic transmission of the measles virus in late September 2016; this was also achieved in Venezuela in 2018 and in Brazil in 2019. Several other countries have confirmed measles eradication and countries from all six WHO regions have set measles eradication targets. In 2019, a total of 83 countries were certified as having achieved or maintained measles

Elimination. During the COVID-19 pandemic, there was a significant drop in measles cases worldwide. A few cases of measles have been documented in the European Union countries, including in areas where endemic transmission had previously been abolished or endemic. The number of cases registered on the European continent has dropped from a few hundred each month to sporadic occurrences. No additional fatalities were reported by European Union countries in 2021. Vitamin A supplementation can be given to measles patients in order to reduce the measles-associated complications and mortality rates. Vitamin A deficiency impacts the severity of measles since it slows recovery; it may cause measles-related problems, such as blindness; and may be linked to a higher death rate. The American Academy of Pediatrics (AAP) and the WHO advocated for vitamin A treatment for hospitalised children with measles Compared with a single dose, two doses of vitamin A supplements have been shown to reduce the risk of measles-associated mortality in children younger than 2 years Vitamin A supplements should be given in two doses every 24 h to all children diagnosed with measles. This medication may help to avoid eye damage and blindness by restoring low vitamin A levels during measles infection, which can occur even in wellnourished children.
Advances in the Administration of the Measles Vaccine Currently, none of the WHO’s elimination goals for measles are being met. Despite this, efforts to improve the situation are still ongoing Currently, the measles vaccine is administered as a trivalent vaccine (MMR), along with mumps and rubella. Most of the reasons for the difficulty of eliminating the measles virus are focused on vaccinations. The problems with low coverage of vaccinations start with the vaccine in itself: the price of the vaccine, use of multi-dosage vials leading to loss of vaccine, improper reconstitution of vaccine, the lack of cold storage, and finally, the lack of expert healthcare workers . To overcome such limitations, extensive research was done to formulate the vaccine as microneedle patches. These patches are designed to be placed on the skin to administer the measles and rubella vaccine through a fine array of micronscale needles.
These micron-scale needles contain the active ingredient of the measles and rubella vaccine and other water-soluble excipients and are designed to dissolve when placed on the skin. These patches were shown to maintain their potency, even at elevated temperatures, and can be safely used in extreme temperature conditions, such as in Africa. These patches would not require any experienced healthcare workers and can be safely administered by parents. The neutralisation titters produced with the microneedle vaccine patch and the subcutaneous injections of the vaccine were the same when administered in cotton rats [7]. Similar results were obtained when the vaccine was administered as a patch or through subcutaneous injections in Rhesus monkeys [7]. While these preclinical studies show excellent results, there is a need for further clinical studies to see whether they exhibit similar results in human beings.
Eradication: Goals and Progress
The World Health Assembly (WHA) 2010 set three objectives for worldwide measles control by 2015. The first objective was to increase the measlescontaining vaccine coverage (MCV1) in children aged 1 year to 90% and 80% at national and district levels, respectively. The second objective was to decrease the global annual measles incidence to <5 cases per 1 million individuals. The third objective was to reduce the measles mortality rate by 95% from the 2000 estimate. A recent study reported the progress towards measles elimination worldwide. The MCV1 vaccine coverage increased globally from 72% to 86% during 2000–2018, the measles incidence declined from 145 to 49 cases per 1 million individuals, and there was a 73% decrease in the annual measles-associated mortality Although there was a significant decline in the overall measles-related mortality during 2000–2018, there was a global increase (about 167%) in the incidence of measles in 2018 as compared with 2016. Furthermore, measles-related mortality has increased since 2017 This measles-related mortality can be further magnified because of the current COVID pandemic. Ever since the COVID pandemic struck across the world, the WHO recommended temporarily suspending mass vaccination programs worldwide [10].
This led to lower vaccination rates, and it could be further reduced moving on forward. Due to the COVID pandemic, social distancing, mask mandates, and online education might have contributed to no measles outbreaks. However, there might be a return of measles outbreaks when people start travelling to measles-endemic areas or citizens from these areas travel around the world. A single dose of the Schwartz vaccine was started in 1982 in Saudi Arabia. It took almost a decade to introduce the two-dose measles vaccine in Saudi Arabia.
A twodose Edmonston–Zagreb measles vaccine was introduced in 1991 [10]. The first dose was given at 6 months of age and the second dose at 12 months of age. Implementing a two-dose vaccine shifted the infection age from younger to older age. Moreover, it was observed that even in the vaccinated population, about 50% of measles cases were observed in the 1–4-year-old age group.
The availability of effective vaccines for measles and efforts of the government to implement routine vaccination has reduced the measles incidence worldwide, and measles is now eradicated in some countries.
IV. CASE STUDY 4.1 DRUG
Profile
Treatment of Measles
There is no specific treatment for measles. The virus and symptoms generally disappear within two to three weeks but the doctor might recommend the following treatments:
- Medications that help to improve the immune system.
- Medications to reduce a cough and sore throat.
- Acetaminophen to reduce muscle pains and fever.
- Foods that are rich in vitamin A.
In the case of children, it is advised that they should be closely monitored by a doctor. Children should be placed in isolation until they are fully recovered.
Vaccines ; There are various types of measles vaccines, the monocomponent is used in most African countries and in others, including Russia [7]. The combined mumps, measles, rubella (MMR) vaccine is used instead in the rest of Europe and North America. A combined quadrivalent of mumps, measles, rubella, and varicella (MMRV) is also available in the United States and presents safety and immunogenicity similar to the MMR vaccine [7], although the risk of febrile convulsions is higher compared to the trivalent one. All these vaccines are attenuated viral vaccines that replicate within the host to induce protective immunity.
The World Health Organization recommends the first dose to be given at 12 months and the second dose at 15 to 18 months [8]; the CDC-recommended schedule in the United States is to administer the first dose at age 12 to 15 months and the second dose at age 4 to 6 years [8]. In some special cases, the WHO recommends the first dose of measlescontaining vaccine (MCV1) to be administered at 9 months of age in contexts with endemic measles. In special situations, such as during outbreaks, the first dose can be anticipated at 6 months, the same for displaced populations or children with HIV infection [8]. However, some studies have shown that in the two-dose vaccination program, when the first dose is administered before the age of 15 months, the susceptibility to measles infection is higher at up to 2–4 fold [8]. In this regard, it should be added that there is evidence of how, if the first dose is given before or after the age of 9 months, there is a lower antibody titer but the vaccination efficacy is not inferior, as the T-cell response is independent of vaccination timing. In any case, the WHO recommends two doses of vaccine when the first is administered before 9 months.

Prevention of Measles
The adverse effects of the measles vaccine are extremely infrequent and in most cases with minimal clinical impact and self-resolving. Table 1 compares the incidence of the main complications of measles infection and that of side effects after the measles vaccine.
Table 1. Comparison between main side effects of measles vaccination and main complications of measles infection
As there is no specific treatment, it is advised to follow all necessary precautions which help to prevent measles. Children should be vaccinated within 12 months of their birth and the second dose should be between the ages of 4 and 6. MMR is a vaccine that prevents three diseases like mumps, measles, and rubella. Treating the disease in early stages is also very important, especially for children.
Conclusion
A. Summary Measles virus is an immunosuppressive virus that can cause very severe or life-threatening disease. However, a highly effec-tive vaccine is available and its prudent use could result in the eradication of MV infections whenever appropriate immun-ization strategies are used, such as with endogenous infections in the US. Nevertheless, the virus still causes enough infec-tions throughout the world to be one of the leading causes of death in the world due to infectious disease. This necessitates, even in areas where MV is no longer endemic, massive, prolonged and stringent immunization campaigns to prevent the es-tablishment of endogenous infections where MV has been eliminated (as happened in the UK) and to facilitate eradication of the virus in areas where infection is still endemic. Any generational lapse in protection from immunization could result in the establishment of a cohort of individuals who would be susceptible to morbidity and mortality due to MV, which could be of historical proportions. B. Conclusions The countries claiming complete eradication of measles are still at risk for measles outbreaks until the virus is circulating in other populations. The measles virus can be acquired through travel in these countries. Measles outbreaks result in a finan-cial burden on the economy. Although vaccine coverage has increased drastically in the last decade through awareness and surveillance worldwide, vaccine denial remains the major problem in eradicating measles. Since measles is associated with sequelae of secondary infections, adequate supportive therapy, such as vitamin A supplementation and antibiotics, should be provided by government-sponsored programs to effectively and adequately manage measles-associated mortality. The immune amnesia associated with measles infection is a matter of general concern, especially in undernourished and immun-ocompromised individuals. Therefore, measles patients should be promptly evaluated for other infections and managed ac-cordingly.
References
[1] Gay, N.J. The theory of measles elimination: Implications for the design of elimination strategies. J. Infect. Dis. 2004, 189, S27–S35. [2] Nambulli, S.; Sharp, C.R.; Acciardo, A.S.; Drexler, J.F.; Duprex, W.P. Mapping the evolutionary trajectories of morbilliviruses: What, where and whither. Curr. Opin. Virol. 2016, 16, 95–105. [3] Griffin DE (2003) Measles virus. In Fields Virology, vol. 1, 3rd edition.Edited by DM Knipe & PM Howley. Philadelphia:Lippincott– Raven,401–1440. [4] Dabbagh, A.; Laws, R.L.; Steulet, C.; Dumolard, L.; Mulders, M.N.; Kretsinger, K.; Alexander, J.P.; Rota, P.A.; Goodson, J.L. Progress toward regional measles elimination—Worldwide, 2000–2017. Morb. Mortal. Wkly. Rep. 2018, 67, 1323. [5] Lin CC, Philips L, Xu C & Yeh LT (2004) Pharmacokinetics and safety of viramidine, a prodrug of ribavirin, in healthy volunteers. Journal of Clinical Pharma-cology 44:265–275. [6] Patel, M.K.; Dumolard, L.; Nedelec, Y.; Sodha, S.V.; Steulet, C.; GacicDobo, M.; Kretsinger, K.; McFarland, J.; Rota, P.A.; Goodson, J.L. Progress toward re-gional measles elimination—Worldwide, 2000–2018. Morb. Mortal. Wkly. Rep. 2019, 68, 1105. [7] Wachsman MB, Ramirez JA, Galagovsky LR & Coto CE (2002) Antiviral activity of brassinosteroids derivatives against measles virus in cell cultures. Antivi-ral Chemistry & Chemotherapy 13:61–66. [8] Measles, Mumps, and Rubella (MMR) Vaccination: What Everyone Should Know. Available online https://www.cdc.gov/ vac-cines/vpd/mmr/public/index.html (accessed on 10 December 2022). [9] Venekamp, R.P.; Sanders, S.L.; Glasziou, P.P.; Del Mar, C.B.; Rovers, M.M. Antibiotics for acute otitis media in children. Cochrane Database Syst. Rev.2015, 1, CD000219. [10] Bester, J.C. Measles and measles vaccination: A review. JAMA Pediatr. 2016, 170, 1209–1215.
Copyright
Copyright © 2023 Mr. Sumedh Narayan Sonkamble, Mr. Prajwal Balaji Phad, Ms. Pooja Prashant Kharosekar, Ms. Pooja Murari Kotmale, Ms. Pranita Waghambar Waghmare, Mr. Pradip Uddhav Waghmare, Mr. Prashant Machhindra Waghmare. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET56085
Publish Date : 2023-10-10
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

