Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Revolutionizing Healthcare: The Transformative Power of Artificial Intelligence
Authors: C. Santhosh
DOI Link: https://doi.org/10.22214/ijraset.2024.61755
Certificate: View Certificate
Abstract
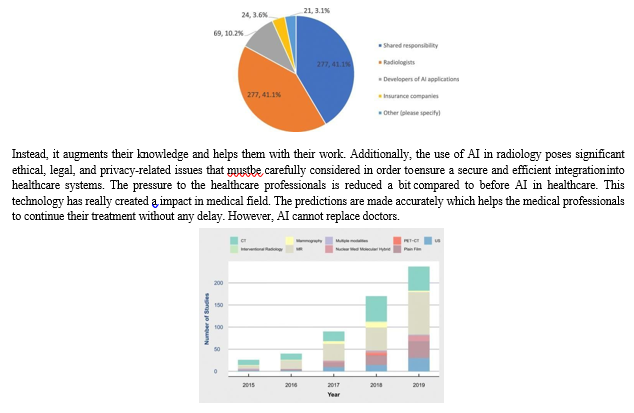
The field of radiology is changing due to artificial intelligence (AI), which presents hitherto unheard-of chances to improve diagnostic efficiency and accuracy. The transformational potential of AI in radiology is examined in this research, with particular attention to how it might expedite clinical workflows and completely change picture interpretation. The first section of the abstract emphasizes the rising need for radiological services as well as the difficulties radiologists have in organizing massive amounts of patient data while maintaining prompt and precise diagnosis. The article goes on to discuss AI as a potent tool that radiologists may use to analyze pictures more confidently, spot abnormalities, and make clinical choices more quickly. The transformational potential of artificial intelligence (AI) in radiology is examined in this research, with a focus on how AI might enhance diagnostic efficiency and accuracy. It presents the potential of artificial intelligence (AI) to transform radiological practice by highlighting its strengths in image interpretation, anomaly detection, and clinical decision assistance. But there are drawbacks to using AI in radiology, including concerns about data privacy and algorithm transparency. In order to guarantee patient safety and confidence in AI-enabled radiological techniques, the study highlights the significance of responsible AI implementation. The study concludes by highlighting the revolutionary effects of AI on radiology and highlighting its potential as a tool to improve healthcare delivery and diagnostic accuracy. General Terms: Medical Imaging, Healthcare Technology, Diagnostic Innovation
Introduction
I. INTRODUCTION
In a time of constant technical advancement, Artificial Intelligence (AI) stands out as the innovation that will usher in a revolution in healthcare. AI has the ability to bring in a previously unheard-of era of accuracy, efficiency, and innovation in healthcare, revolutionizing medical diagnoses, patient care, and treatment paradigms. This abstract extends an invitation to you to embark on an insightful journey into the future of medicine, one in which AI assumes a prominent role. Our investigation will show the various ways that AI is transforming healthcare, empowering medical practitioners to make better informed decisions, create individualized treatment plans, and maximize the use of limited resources. Let's highlight the outstanding progress that AI has made in the field of radiology as we explore this transformational terrain.
Radiology, a foundational area of contemporary healthcare, has seen a significant transformation as a result of the use of AI. We will show how artificial intelligence-driven predictive analytics are promoting the early detection of medical disorders, thereby improving the effectiveness of interventions and concurrently lowering the skyrocketing healthcare costs that burden individuals and governments alike. We'll also show how AI is advancing the area of radiology, improving the analysis of diagnostic images, and accelerating the detection of anomalies.
This speeding up leads into more efficient, quicker patient treatment, which ultimately improves health outcomes. But without addressing the crucial ethical issues that surround the application of AI in healthcare, our exploration of this synergy would be lacking. As we consider the great potential of AI to improve healthcare, the proper use of AI and the protection of patient data assume critical importance. We will explore the most recent developments, case studies, and practical uses of AI in healthcare together. In our future vision, AI will advance healthcare delivery and become a trusted ally rather than just a tool in the noble quest to provide the best possible care for patients.
We will use the power of innovation to transform the healthcare landscape as we delve deeper into the seemingly limitless potential of AI in healthcare. Let's now examine how AI is transforming radiology, a field where its effects have been particularly significant. AI in radiology is particularly profound like improved diagnostic precision, Rapid Diagnosis, Effortless Workflow, Customized Treatment Programs, Disease Early Detection, cost reduction, Electronic Health Records (EHRs) integration, Ethics-Related Matters, Constant Improvements, Patient-Centric Methodology.
II. HEALTHCARE DEVELOPMENT PRIOR TO AI IN RADIOLOGY:
Healthcare faced a number of difficulties in the field of medical imaging before the introduction of artificial intelligence (AI) in radiology. It took a lot of time and effort for radiologists to manually study and interpret complex medical images. Consequently, diagnosis and treatment were frequently delayed. Despite their great level of expertise, human radiologists were prone to subjectivity in their readings. When analysing the same set of images, various radiologists may come to slightly different interpretations, which may have an impact on patient care decisions. In some areas, there was a dearth of skilled radiologists, which increased the length of time patients had to wait for diagnosis and image interpretation. Healthcare organizations frequently struggled to efficiently distribute resources, like imaging technology and radiologists, which led to a delay in diagnoses and higher expenses. Because they required a high level of knowledge and experience to recognize, subtle or early indicators of diseases were occasionally missed. This affected patient outcomes and the start of the treatment. It was a major logistical difficulty to manage and store enormous amounts of medical imaging data in a safe and convenient manner. The traditional radiology procedure required a lot of infrastructure and labour, which raised the cost of healthcare as a whole. Using AI, healthcare practitioners may optimally allocate radiologists and imaging technology, reducing patient wait times and maximizing resource utilization. By standardizing the analysis of medical pictures, AI-driven systems can offer reliable quality assurance. As a result, there is less chance of human error and each patient receives the same amount of rigorous inspection. AI makes it easier for healthcare workers to work together by enabling the sharing of medical images and insights across many locations, leading to better patient care coordination. Artificial intelligence (AI) technologies can automate the documentation of radiology reports and conclusions, easing the administrative strain on healthcare personnel and ensuring thorough records for future reference. Thanks to AI-driven telemedicine solutions, patients in underserved or remote areas can obtain specialized radiological services without having to physically travel. Thanks to AI solutions that give patients access to their own medical images and data, promoting informed decision- making, patients are increasingly taking an active role in their healthcare journey. New directions in medical research are being sparked by the quantity of data produced by AI-enhanced radiology, which is resulting in advancements in the knowledge of diseases, the creation of treatments, and healthcare policy. In order to protect patient safety and data privacy, the integration of AI in radiology has forced the development of regulatory frameworks. In order for healthcare personnel to keep up with these technological breakthroughs, they must get continual training and education.
III. HEALTHCARE DEVELOPMENT FTER THE AI IN RADIOLOGY
AI systems can help radiologists find abnormalities and make diagnoses that are more precise. This can result in earlier disease detection, lowering the possibility of misdiagnosis or missing diagnoses. By automating basic tasks like image analysis, AI can help radiologists focus on more difficult situations by streamlining radiological workflows. This could improve the effectiveness of healthcare delivery and shorten patient wait times. AI can assist reduce healthcare expenses by improving radiology departments' productivity and minimizing the need for repeat tests and pointless treatments. A great deal of patient data can be analysed by AI to produce more individualized therapy recommendations. This may result in more individualized treatment approaches that are less likely to have negative side effects. AI-driven radiology tools can be incorporated into telemedicine platforms, allowing for remote medical picture interpretation. This is especially helpful in remote or underserved locations with limited access to specialized healthcare. Artificial intelligence (AI) can aid with the analysis of huge datasets to find trends and patterns in the occurrence of diseases, assisting healthcare professionals and policymakers in making well-informed decisions about public health initiatives.
By evaluating big datasets and finding promising targets for further exploration, AI can support drug discovery, illness modeling, and medical research. However, the use of AI in radiology also brings up moral and legal issues, such as worries about data privacy, algorithm bias, and the necessity of thorough AI algorithm validation. Additionally, radiologists and other healthcare workers could need to learn new responsibilities and develop AI tool collaboration abilities. In general, incorporating AI into radiology has the potential to improve the effectiveness and quality of healthcare, but it also needs to be carefully implemented and continually monitored to guarantee patient safety and data protection. As rules and technology progress, the effect on healthcare may continue to change. AI can aid in standardization and enhance the consistency of radiological reports. It can lessen variety in how findings are documented by automating the reporting process and using standardized templates. By prioritizing urgent cases, indicating potential problems for review, and minimizing administrative tasks for radiologists, AI can assist radiology departments optimize their workflow. AI can be utilized as a training and educational tool in the field of radiology. Medical students and residents who use it can receive performance evaluation and learn how to evaluate medical images. Artificial intelligence (AI) can be a useful tool for offering second thoughts. Radiologists can consult AI algorithms to increase the accuracy of their diagnoses and utilize AI to help with their assessments. AI can help with patient triage and case prioritization based on the seriousness of the findings. This can ensure that urgent patients get the care they require. AI can help a healthcare system allocate resources more efficiently by recognizing cases that call for more time and attention from radiologists. AIdriven analysis of medical pictures has the potential to advance medical science by fostering the creation of new diagnostic methods and therapeutic modalities. To handle the enormous amounts of medical imaging data created by the integration of AI, reliable data management solutions are required. Engagement of Patients: AI techniques can be used to involve patients by giving them access to their medical images and assisting them in understanding their ailments and available treatments. The use of AI in radiology introduces regulatory challenges, including the need for validation, quality control, and adherence to healthcare regulations and standards. AI tools can be used to engage patients by providing them with access to their medical images and helping them better understand their conditions and treatment options. Healthcare organizations need to make sure AI solutions can easily connect with current infrastructure and work with other medical technology. The ethical application of AI in radiology entails addressing concerns about patient consent, data privacy, algorithm bias, and decision-making openness. Healthcare organizations must evaluate the cost-effectiveness of using AI in radiology, taking into account elements including the initial investment, ongoing expenses, and possible savings. AI has the ability to completely transform radiology by enhancing productivity, precision, and patient care.
IV. DATASETS USED FOR TRAINING THE AI MODEL
Machine learning algorithms in radiology are trained and validated using a variety of medical imaging datasets. For tasks like picture classification, object detection, segmentation, and disease diagnosis, these datasets are essential for creating and testing AI models. In the study and development of AI radiology, the following datasets are frequently used are The Cancer Imaging Archive (TCIA) which is a comprehensive repository for cancer imaging data, comprising datasets from several imaging modalities like CT, MRI, and PET scans. It has data from a variety of cancer types and National Lung Screening Trial (NLST) is a crucial tool for the early diagnosis and study of lung cancer since it collects CT scans from people who are at high risk for the disease. The Digital Database for Screening Mammography (DDSM) is a dataset made up of mammograms and the ground truth labels that go with them. It is primarily used to identify breast cancer. ImageNet is a sizable dataset used for convolutional neural networks (CNNs) training, despite not being specifically related to radiology. On ImageNet, researchers may train CNNs in advance and then fine-tune them for radiological tasks. OpenI is a collection of open-access chest X-rays and the radiology reports that go with them is known as OpenI. It is frequently employed in radiology research pertaining to text-based image retrieval and NLP. ChestX-ray14 is a dataset, which contains more than 100,000 chest X-ray images labeled for a variety of thoracic disorders, is valuable for creating AI models for analysing chest X-rays. Lung Image Database Consortium and Image Database Resource Initiative (LICD-IDRI) is a useful tool for identifying and characterizing lung nodules is LIDC-IDRI, which has lung CT scans annotated for nodules. Brain MRI Datasets contains a number of brain MRI scan datasets are available for activities including detecting brain tumours, segmenting them, and classifying diseases. The Alzheimer's Disease Neuroimaging Initiative (ADNI) dataset is one example. Prostate MRI Datasets is a ProstateX dataset is a famous example of a dataset of prostate MRI images used for the detection and diagnosis of prostate cancer. Retinal imaging datasets are one example of a dataset with retinal images is the Kaggle Diabetic Retinopathy Detection dataset, which is used to identify diabetic retinopathy. Datasets of cardiac pictures, such as echocardiograms and cardiac MRI scans, are utilized for activities linked to the diagnosis and evaluation of heart illness. Pediatric Imaging Datasets are the NIH Pediatric MRI Data Repository is one of the datasets utilized in pediatric radiology research that includes medical pictures of children. Mammography Images are the dataset help with breast cancer detection.
MRI Brain Images is used to understand issues like Alzheimer's disease. CT Scans are detailed images used for finding things like lung nodules or problems in the liver and kidneys. Histopathology Images are the Pictures of tissue samples help in cancer detection. For the purpose of advancing radiology AI research, these datasets are frequently annotated and maintained. It is critical to remember that while working with medical imaging data, researchers must adhere to data usage and privacy restrictions and that access to some of these datasets may be restricted. In addition, developing fresh, customized datasets can be required for certain research aims and therapeutic applications.
V. ALGORITHM USED TO READ THE DATASET TO TRAIN THE AI MODEL
Convolutional Neural Networks (CNNs) go through a number of processes to read and process datasets for training AI models, notably for image-related applications. The dataset must first be loaded into memory. This entails accessing the dataset files and getting them ready for input using programming libraries and tools. For picture datasets, this can entail reading image files along with any labels or annotations they may have. To make raw data appropriate for training, preparation is frequently necessary. Common preprocessing are resizing, normalization, OneHot Encoding. Images can be downsized to a standard resolution to maintain uniform dimensions. In order to stabilize training and boost convergence, pixel values are scaled to have a mean of 0 and a standard deviation of 1. Labels are frequently one-hot encoded when classification is the task, converting categorical labels into a binary vector format. Convolutional layers are the main constituents of CNNs. These layers run the incoming data through a series of trainable filters (kernels). Slided over the input, these filters compute dot products and generate feature maps that identify regional patterns or characteristics. Pooling layers are frequently used after convolutional layers to decrease computational complexity and spatial dimensions while preserving crucial features. Max-pooling and average-pooling are two common pooling techniques. Lattening is a one-dimensional vector is created using the feature maps that the convolutional and pooling layers have produced. The information is now ready to be entered into a fully linked neural network. Layers that are fully connected link every neuron in one layer to every neuron in the one above. To make final predictions, fully connected layers are often used toward the conclusion of the CNN design. They may have several submerged layers. For classification tasks, the output layer typically has the same number of neurons as the classes in the dataset. It might just have one neuron for regression tasks. To add non-linearity to the network, activation functions like ReLU (Rectified Linear Unit), Sigmoid, or Softmax are applied at each layer. In Loss Function CNNs measure the error between the predicted outputs and the ground truth labels using a loss function (for example, cross-entropy for classification). Optimization is to update the weights of the network and minimize the loss function, gradient descent optimization methods are utilized (e.g., Adam, SGD). During training, preprocessed input data are fed into the CNN in batches, and backpropagation is used to update the weights. The model is trained for a predetermined number of epochs or until it reaches an acceptable performance level. Validation is to keep track of the model's generalizability and prevent overfitting, its performance is periodically assessed on a different validation dataset. Testing is to evaluate the model's performance in the real world, a test dataset is used after training is finished and the model has demonstrated success on the validation set. In deployment the learned CNN model may be used to make predictions on fresh, unforeseen data following successful training and testing.
VI. BEFORE AND AFTER THE AI IN RADIOLOGY
The introduction of AI in radiology has significantly changed the discipline and brought about a number of notable adjustments and advancements in a number of different areas of radiology. Here are some significant findings and modifications noted both before and after the application of AI to radiology. Before AI in radiology it is fully Manual Interpretation, Restricted speed, Variability, Workload. Radiologists relied primarily on their knowledge and the laborious, time-consuming, and error-prone interpretation of medical pictures. There could be delays in diagnosis and treatment planning due to the somewhat lengthy process of evaluating and interpreting a huge amount of medical images. Different radiologists' interpretations could differ from one another, which could result in inconsistent diagnoses. Radiologists frequently had tremendous workloads, particularly in hectic medical environments, which could lead to burnout and exhaustion. After AI in radiology, AI- powered algorithms can analyse and interpret medical pictures quickly, enabling quicker and more accurate reporting and diagnosis. AI systems can serve as a second set of "eyes" for radiologists, assisting them in spotting anomalies and potential problems in pictures and decreasing the likelihood that a diagnosis would be overlooked. AI can automate repetitive and routine processes like image segmentation and measuring, freeing radiologists to concentrate on more complicated situations and clinical decision-making. AI systems offer reliable interpretations that are standardized and consistent, lowering interobserver variability. AI may make photos clearer and more informative by denoising, boosting contrast, and optimizing image capture parameters. AI can help radiologists prioritize critical cases and manage to-do lists, improving productivity.
AI has the ability to find patterns and trendsin vast datasets of medical picturesthat were previously difficult to notice, advancing patient care and advancing medical research. AI can speed up access to expert opinions and facilitate remote consultations by automating preliminary reports. Artificial intelligence (AI) can be utilized as a tool for education and training, enabling radiology practitioners and students to learn and hone interpretation abilities under the guidance of AI. While AI has greatly aided radiology, it is crucial to remember that human radiologists are still required.
VII. CHALLENGES
To ensure patient safety and data privacy, the application of AI in healthcare requires adherence to stringent regulatory norms and ethical principles. It can be difficult to integrate AI systems with the current healthcare IT infrastructure, and getting there is still a big problem. Collaboration between radiologists and AI systems needs clear communication, the development of trust, and the resolving of concerns about job displacement. AI models rely largely on a wide range of high-quality datasets. It can be difficult to guarantee that these datasets are accessible. However, people will be clear about their problem only when they communicate with the healthcare professionals. And also people will never believe that they have a certain problem unless the doctor tell them even after the patient seeing their report generated by Artificial Intelligence. Since, everything is maintained by the AI, the security plays the major role. But still the system is designed to protect the patients data. It may also lead to data overflow.
VIII. FUTURE SCOPE
With improved diagnostic accuracy, faster procedures, and tailored medication, AI in radiology has a bright future. AI systems have the potential to help radiologists identify anomalies more accurately, which would enable earlier illness identification and more efficient treatment. Improved productivity is promised by automating repetitive processes like image segmentation, freeing radiologists to concentrate on difficult decision-making. It is anticipated that the integration of AI with Electronic Health Records (EHR) will yield a thorough patient history for well- informed decision-making. Furthermore, AI's application in remote diagnostics and telemedicine may increase access to specialized care. AI uses massive datasets for pattern recognition to support research and drug discovery in addition to diagnosis.
Responsible AI implementation will require legal frameworks, ethical concerns, and cooperation between healthcare practitioners and AI developers. AI has the potential to completely transform radiology in the years to come by bringing forth innovations like quantitative imaging, which offers precise measures of the course of a disease and how well a treatment is working. Higher resolution and more precise diagnosis are expected when AI is included into current imaging methods. AI's contribution to personalized medicine is also anticipated to result in more effective treatments by customizing treatment strategies based on unique patient features. Access to healthcare services would likely improve as a result of AI's role in enabling telemedicine and remote diagnostics, particularly in underprivileged areas. As artificial intelligence (AI) becomes more pervasive in healthcare operations, developing ethical standards and legal frameworks will be essential to maintaining patient privacy, data security, and responsible technology use. As the area develops, cooperation between regulators, medical practitioners, and AI developers will be crucial to realizing AI's full promise in radiology, which might lead to better patient outcomes and more effective healthcare delivery.
Conclusion
In conclusion, the use of artificial intelligence (AI) to radiography has led to notable developments and enhancements in medical care. AI has completely changed how medical images are handled, analysed, and used for diagnosis and treatment planning. AI technologies help radiologists identify irregularities and probable diseases more accurately, lowering the possibility of making an incorrect diagnosis and enhancing patient outcomes. AI quickens the radiological report turnaround time by accelerating the image analysis process. This effectiveness is especially useful in crisis situations. By ensuring uniform and consistent interpretations, artificial intelligence lowers diagnostic variability among radiologists. AI improves resource allocation, prioritizes urgent cases, and automates mundane procedures to streamline radiology workflows. AI can improve image quality, making it simpler for radiologists to spot tiny anomalies and raising the standard of patient care in general. AI can evaluate enormous amounts of imaging data to provide significant insights, trends, and patterns that might help with population health management, research, and treatment procedures. AI makes telemedicine possible by enabling distant consultations, automating preliminary reports, and enhancing access to specialized care. AI is a useful tool for medical education since it enables practitioners and students to learn new skills and hone existing ones under the guidance of AI.
References
[1] Artificial Intelligence in Radiology, Ahmed Hosny, Chintan Parmar, John Quackenbush, Lawrence H. Schwartz, and Hugo J. W. L. Aerts, 2018 Nov 30, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6268174/ [2] Artificial Intelligence in disease diagnosis, Yogesh Kumar, Apeksha Koul, Ruchi Singla, Muhammad Fazal ljaz, 2022 Jan 13, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8754556/ [3] The Role of Artificial Intelligence in medical imaging research, Xiaoli Tang, 2019 Nov 28, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7594889/ [4] Radiomics: Images Are More than Pictures, They Are Data, Robert J. Gillies, Paul E. Kinhan, Hedvig Hricak, 2015 Nov 15, https://doi.org/10.1148/radiol.2015151169 [5] Gender and Racial Bias in Radiology Residency Letters of Recommendation, Lars J Grimm, Rebecca A Redmond, James C Campbell, Ashleigh S Rosette, 2019 Sep 6, https://pubmed.ncbi.nlm.nih.gov/3149410 3/ [6] Safety of Magnetic Resonance Imaging in Patients With Cardiovascular Devices, Glenn N. Levine, Antoinette S. Gomes, Andrew E. Arai, David A. Bluemke, Scott D. Flamm, Emanuel Kanal, Warren J. Manning, Edward T. Martlin, J. Michael Smith, Norbert Wilke and Frank S. Shellock, 2007 Nov 19, https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.107.187256 [7] Radiology Needs Robust Dialogue, Joseph C. Thomas, BS Richard B. Gunderman, MD, PhD., 2018 15, https://www.jacr.org/article/S1546- 1440(18)30977-3/fulltext [8] Implementing a Software Solution Across Multiple Ultrasound Vendors to Auto-fill Reports with Measurement Values, Meir H Scheinfeld, Oleg Kaplun, Neville A Simmons, Jonathan Sterman, Shlomit Goldberg-Stein, 2018 Oct 7, https://pubmed.ncbi.nlm.nih.gov/30385132/
Copyright
Copyright © 2024 C. Santhosh. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET61755
Publish Date : 2024-05-07
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

